Virgin Islands Model COBRA Continuation Coverage Election Notice
Description
How to fill out Model COBRA Continuation Coverage Election Notice?
Are you currently in a circumstance where you require documents for either business or personal purposes almost every day.
There are numerous legitimate document templates available online, but locating reliable versions can be challenging.
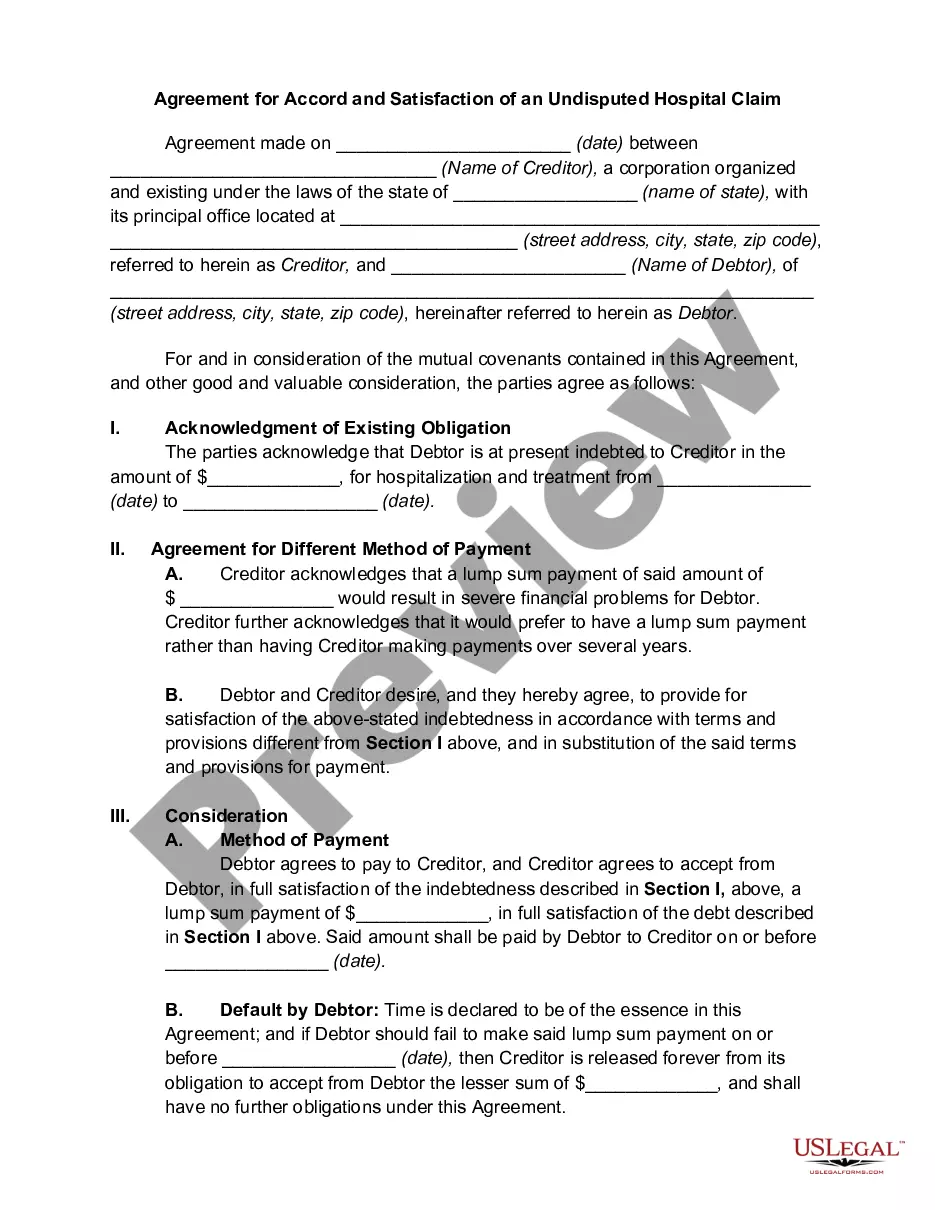
US Legal Forms offers a wide range of form templates, including the Virgin Islands Model COBRA Continuation Coverage Election Notice, designed to satisfy state and federal regulations.
Once you find the right form, click on Buy now.
Choose a suitable pricing plan, fill in the required details to create your account, and pay for your order using PayPal or a credit card.
- If you are already familiar with the US Legal Forms website and have an account, simply Log In.
- Then, you can download the Virgin Islands Model COBRA Continuation Coverage Election Notice template.
- If you do not have an account and wish to start using US Legal Forms, follow these steps.
- Find the form you need and ensure it is for the correct city/region.
- Use the Review option to examine the form.
- Check the details to confirm that you have selected the appropriate form.
- If the form is not what you are looking for, use the Look for section to find a form that meets your needs and requirements.
Form popularity
FAQ
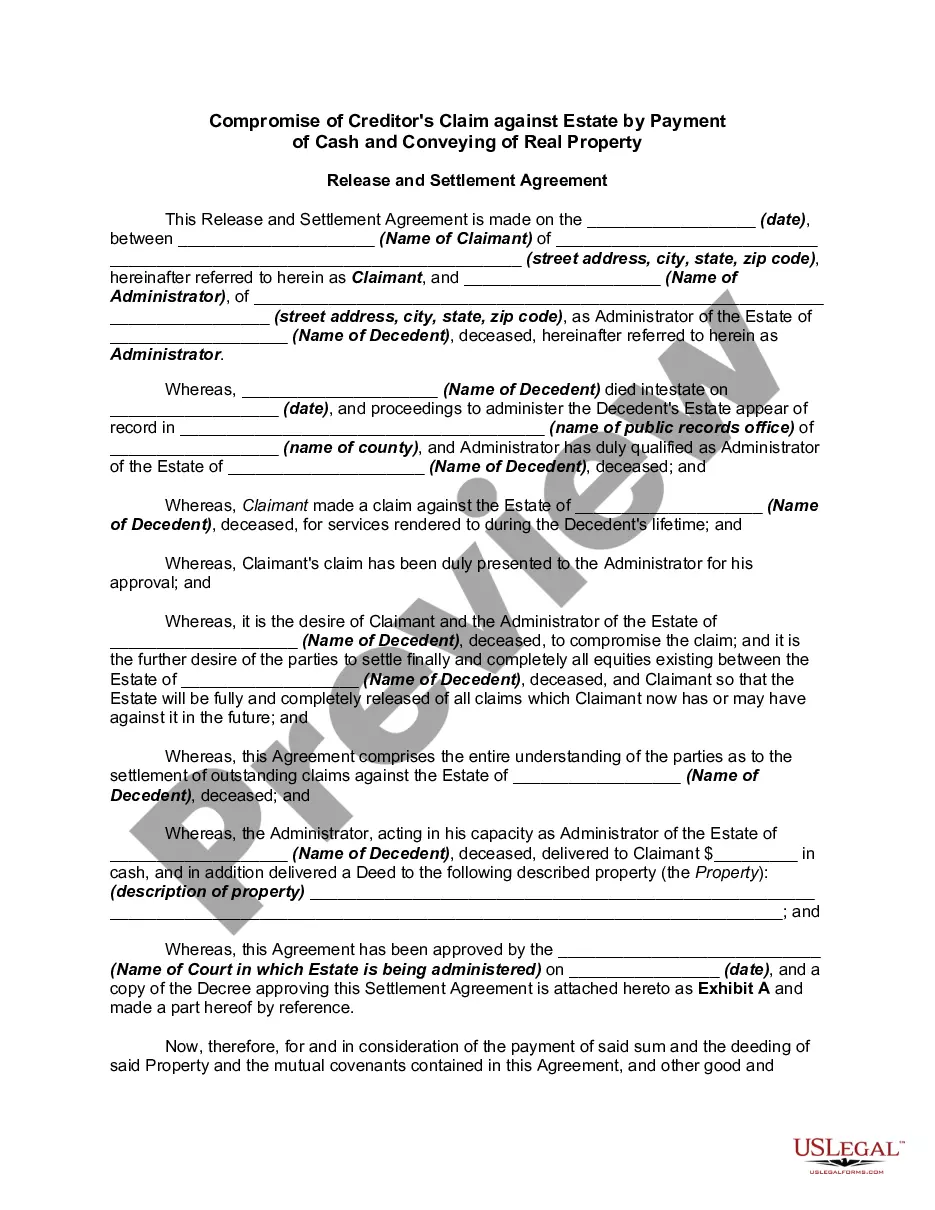
In addition, the law does not apply to plans sponsored by the governments of the District of Columbia or any territory or possession of the United States, certain church-related organizations, or the federal government.
Q2: What is public sector COBRA? Title XXII of the Public Health Service (PHS) Act, 42 U.S.C. ? 300bb-1 through 300bb-8, applies COBRA requirements to group health plans that are sponsored by state or local government employers.
Federal law requires that most group health plans (including this Plan) give employees and their families the opportunity to continue their health care coverage through COBRA continuation coverage when there's a qualifying event that would result in a loss of coverage under an employer's plan.
COBRA the Consolidated Omnibus Budget Reconciliation Act -- requires group health plans to offer continuation coverage to covered employees, former employees, spouses, former spouses, and dependent children when group health coverage would otherwise be lost due to certain events.
Do they have to offer employees COBRA? This rule is generally clear. Small U.S. companies deciding if they are a COBRA eligible employer must include all employees in the controlled group including overseas non-resident aliens without U.S. source income.
The general notice describes general COBRA rights and employee obligations. This notice must be provided to each covered employee and each covered spouse of an employee who becomes covered under the plan. The notice must be provided within the first 90 days of coverage under the group health plan.
COBRA SPECIFICS COBRA applies to nearly all businesses that have more than 20 employees and offer a group health care plan. The only exceptions are churches, church-related tax-exempt organizations, and some federal employees.
Q: What coverage does COBRA offer if I travel outside the US? A: COBRA is a federal law and applies regardless of residency.
The following are qualifying events: the death of the covered employee; a covered employee's termination of employment or reduction of the hours of employment; the covered employee becoming entitled to Medicare; divorce or legal separation from the covered employee; or a dependent child ceasing to be a dependent under