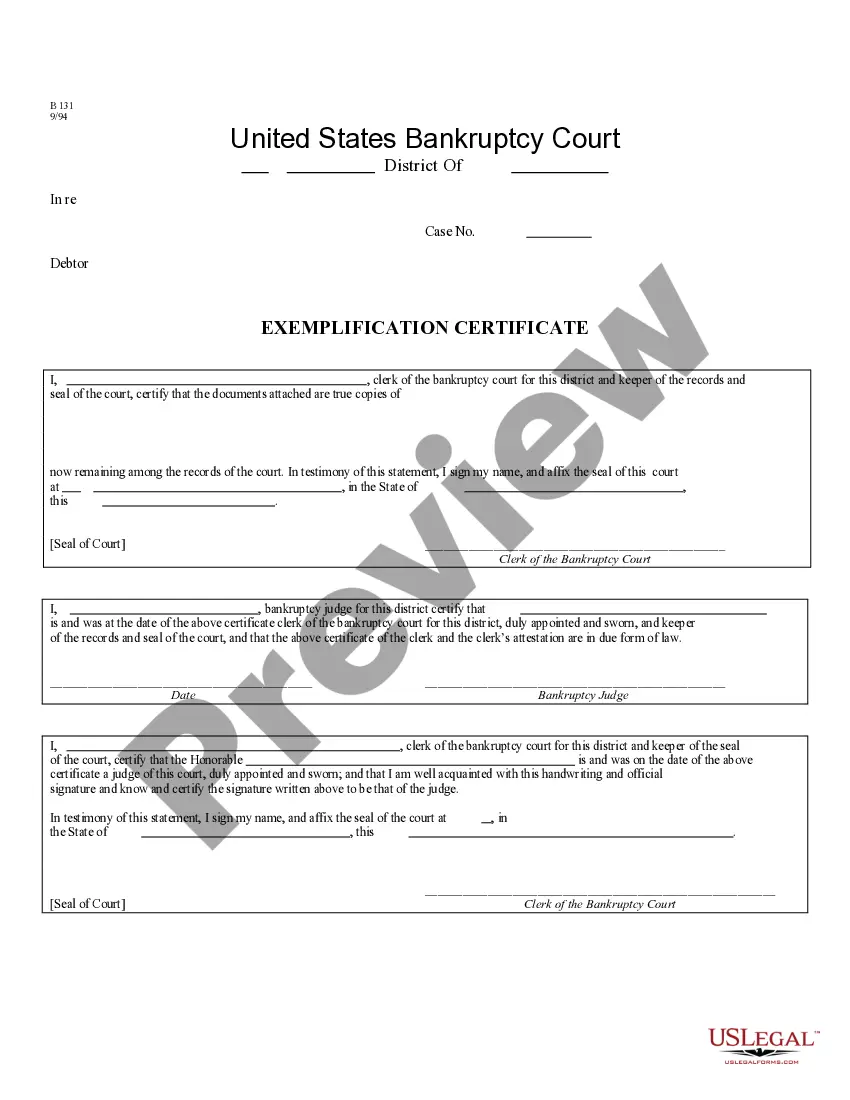
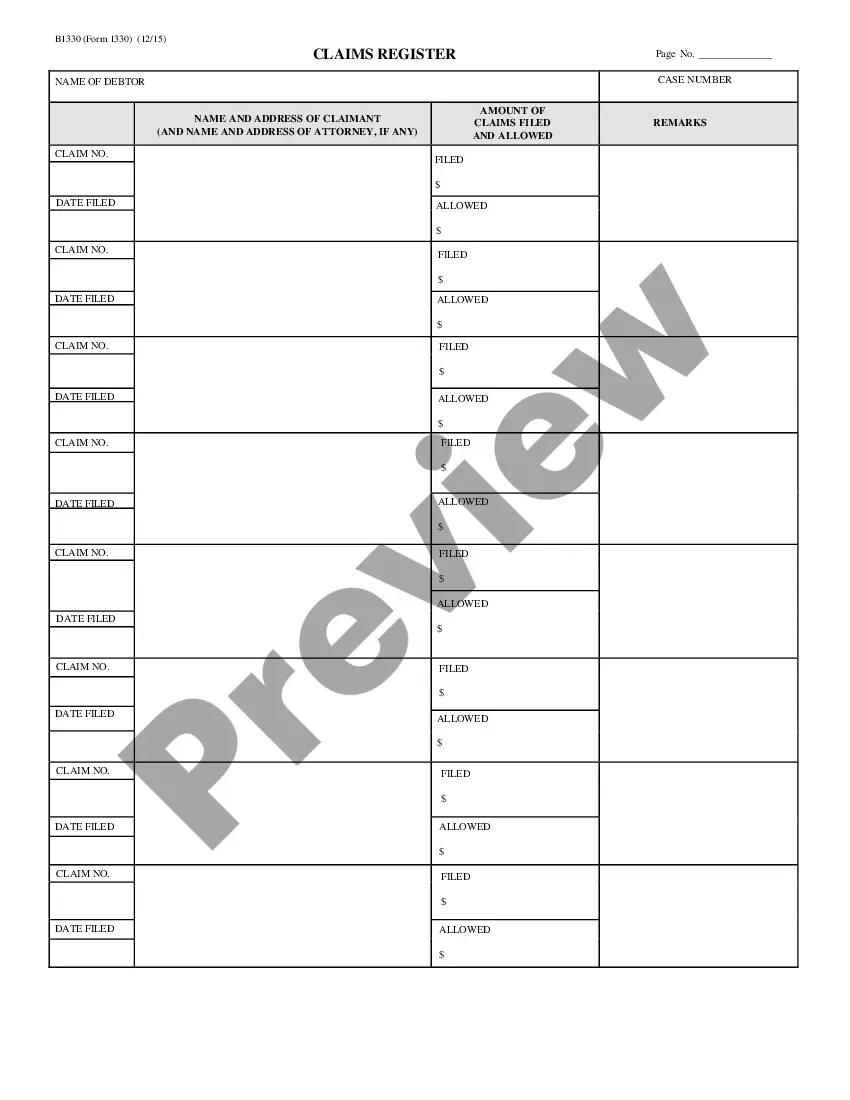
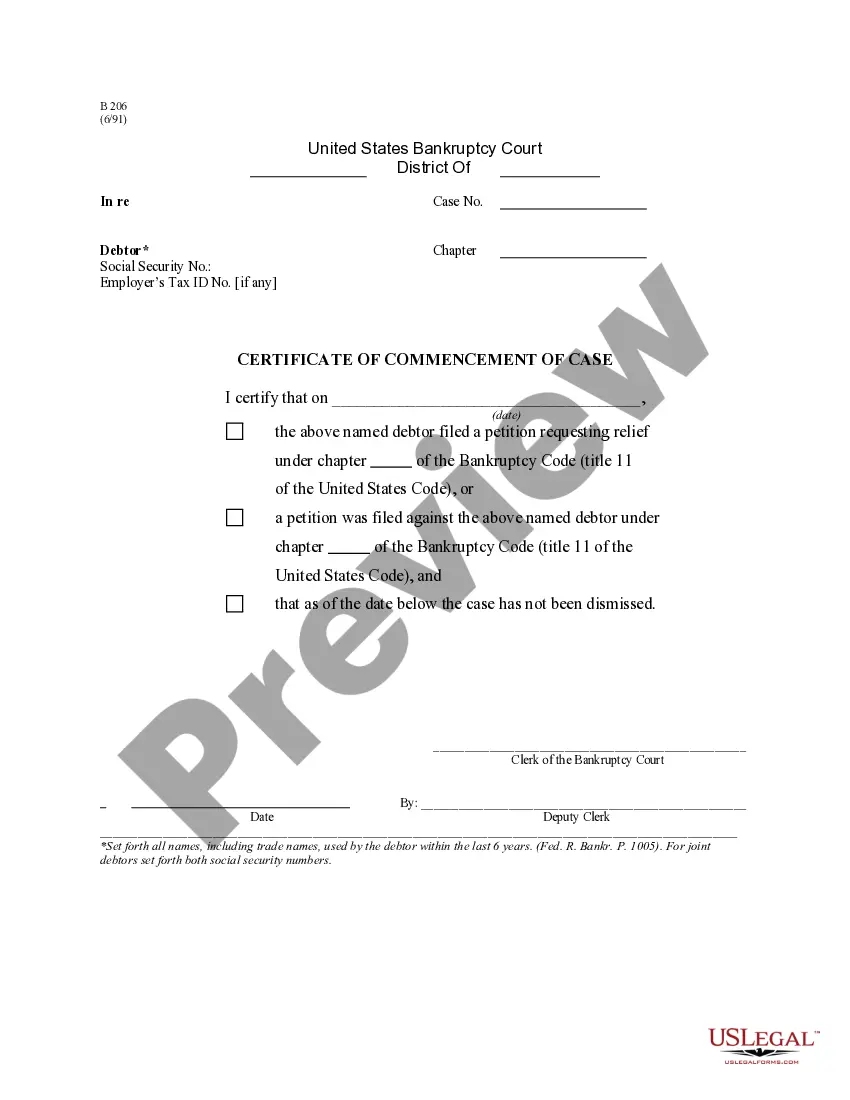
Tennessee Claims Register - B 133
Description
How to fill out Claims Register - B 133?
Discovering the right lawful file format can be quite a struggle. Naturally, there are a lot of themes available on the net, but how can you obtain the lawful kind you want? Make use of the US Legal Forms website. The support provides thousands of themes, including the Tennessee Claims Register - B 133, that can be used for company and personal needs. Every one of the kinds are examined by specialists and fulfill federal and state specifications.
If you are presently registered, log in to your bank account and then click the Down load button to have the Tennessee Claims Register - B 133. Use your bank account to look from the lawful kinds you have bought in the past. Visit the My Forms tab of your own bank account and obtain an additional copy of the file you want.
If you are a whole new consumer of US Legal Forms, listed below are straightforward guidelines that you can stick to:
- First, make certain you have chosen the appropriate kind for the city/area. It is possible to look through the shape while using Preview button and browse the shape description to make sure it is the right one for you.
- In the event the kind is not going to fulfill your expectations, utilize the Seach field to discover the appropriate kind.
- When you are sure that the shape is suitable, click the Purchase now button to have the kind.
- Choose the rates prepare you would like and enter in the necessary info. Create your bank account and purchase an order making use of your PayPal bank account or Visa or Mastercard.
- Choose the data file formatting and obtain the lawful file format to your system.
- Complete, change and printing and indication the attained Tennessee Claims Register - B 133.
US Legal Forms may be the greatest catalogue of lawful kinds for which you can see different file themes. Make use of the company to obtain skillfully-made documents that stick to status specifications.
Form popularity
FAQ
If Medicare denies payment: You're responsible for paying. However, since a claim was submitted, you can appeal to Medicare. If Medicare does pay: Your provider or supplier will refund any payments you made (not including your copayments or deductibles).
What Is the Medicare Claims Processing Manual? The CMS Claims Processing Manual is part of the Internet-Only Manual (IOM) repository, which provides access to comprehensive information about CMS-administered programming.
Confirm or update basic information like addresses, phone numbers, employer, and insurance plan at every patient encounter. Verify eligibility and authorization before the date of service ? These steps are critical for submitting clean claims yet account for about a quarter of all denials.
Dual-eligible beneficiaries are those beneficiaries who are eligible for coverage by both Medicare (either Medicare Part A, Part B or both) and Medi-Cal. Typically, claims for services rendered to dual-eligible beneficiaries are first processed by Medicare and are then sent electronically to Medi-Cal.
Your Medigap (supplemental insurance) company or retiree plan receives claims for your services 1 of 3 ways: Directly from Medicare through electronic claims processing. This is done online. Directly from your provider, if he/she accepts Medicare assignment.
A crossover claim is a claim for a recipient who is eligible for both Medicare and Medicaid, where Medicare pays a portion of the claim, and Medicaid is billed for any remaining deductible and/or coinsurance.
Your provider sends your claim to Medicare and your insurer. Medicare is primary payer and sends payment directly to the provider. The insurer is secondary payer and pays what they owe directly to the provider. Then the insurer sends you an Explanation of Benefits (EOB) saying what you owe, if anything.
Medicare Crossover is the process by which Medicare, as the primary payer, automatically forwards Medicare Part A (hospital) and Part B (medical) including Durable Medical Equipment (DME) claims to a secondary payer for processing.