Pennsylvania Individual Notice of Preexisting Condition Exclusion
Description
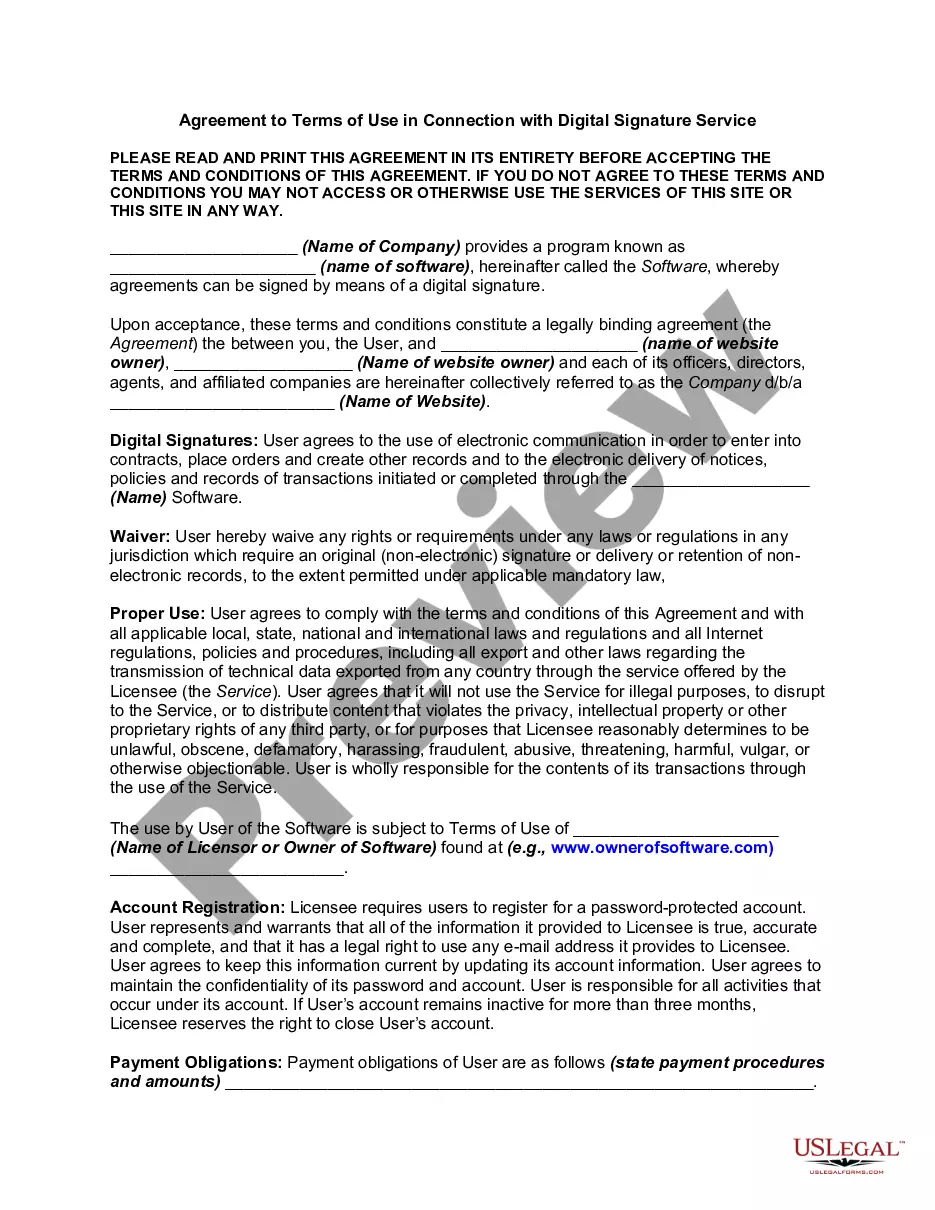
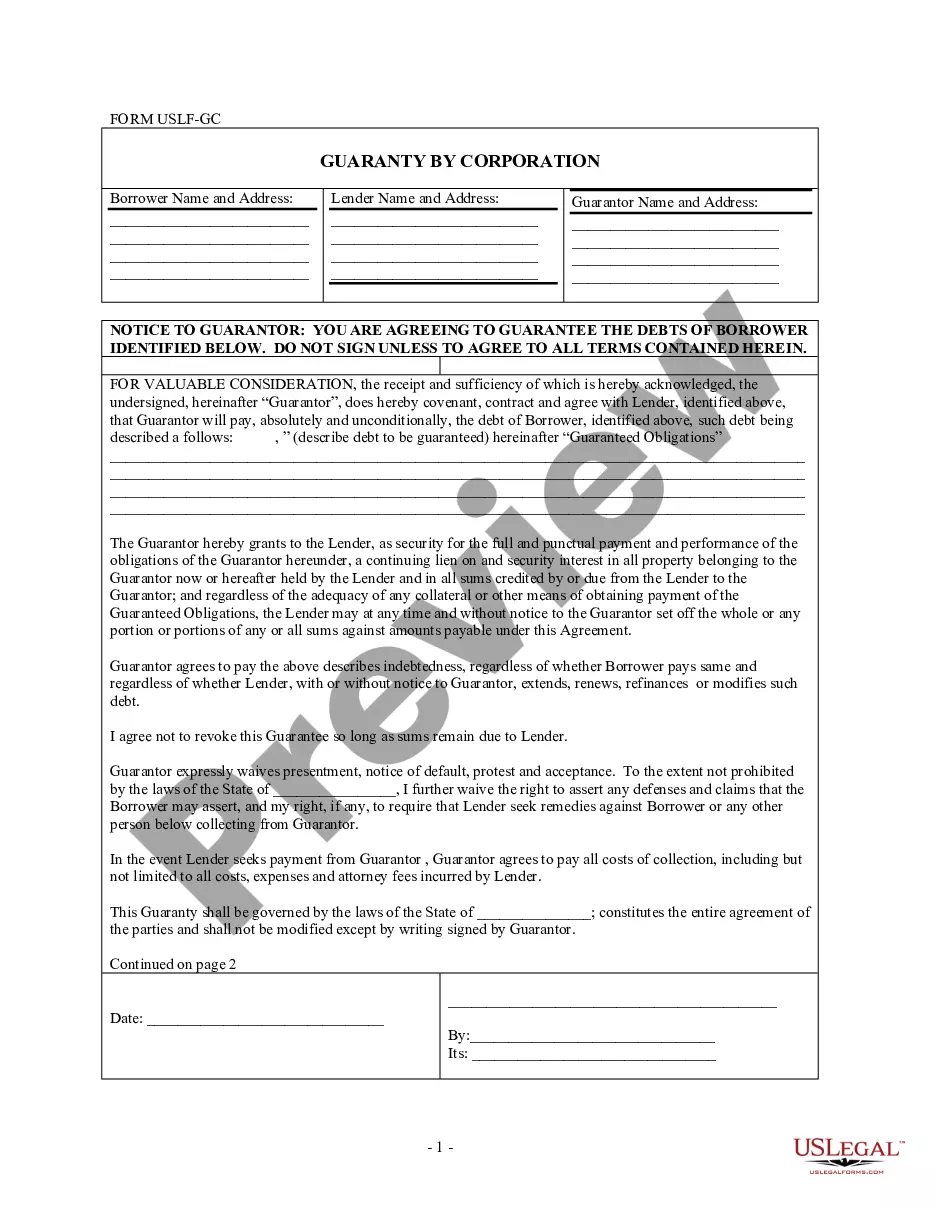
How to fill out Individual Notice Of Preexisting Condition Exclusion?
If you wish to finish, acquire, or print legitimate document templates, utilize US Legal Forms, the largest selection of legal forms available online.
Employ the site's straightforward and user-friendly search to find the documents you require.
Various templates for business and personal purposes are organized by categories and states, or keywords.
Step 4. Once you find the form you need, click the Get now button. Choose your preferred payment plan and enter your details to create an account.
Step 5. Complete the transaction. You can use your credit card or PayPal account to finalize the purchase.
- Utilize US Legal Forms to locate the Pennsylvania Individual Notice of Preexisting Condition Exclusion in just a few clicks.
- If you are already a US Legal Forms member, Log In to your account and click on the Download option to obtain the Pennsylvania Individual Notice of Preexisting Condition Exclusion.
- You can also access forms you previously downloaded from the My documents tab in your account.
- If you are using US Legal Forms for the first time, follow the instructions below.
- Step 1. Ensure you have selected the form for the correct city/state.
- Step 2. Use the Preview feature to review the form's content. Be sure to check the summary.
- Step 3. If you are dissatisfied with the form, use the Search field at the top of the screen to find other versions of your legal form template.
Form popularity
FAQ
It limits the time a new employer plan can exclude the pre-existing condition from being covered. An employer health plan can avoid covering costs of medical care for a pre-existing condition for no more than 12 months after the person is accepted into the plan.
PA 600 L (AS) 1/20. Page 1. Medical Assistance (Medicaid) Financial Eligibility Application. for Long Term Care, Supports and Services. You can also apply online at: .
Identity Identity can be verified by a driver's license, state identification card or another piece of identification. Social Security Number (SSN) A SSN must be provided for each person applying for Medical Assistance.
Application for Benefits (SNAP, Health Care, Cash Assistance) - PA 600. Application for Medical Assistance for Workers with Disabilities - PA 600WD.
The Health Insurance Premium Payment (HIPP) Program is a program developed to help families, who have at least one person enrolled in Medical Assistance (MA), pay for private health insurance through an employer. HIPP is administered by Pennsylvania's Department of Human Services (DHS).
A health problem, like asthma, diabetes, or cancer, you had before the date that new health coverage starts. Insurance companies can't refuse to cover treatment for your pre-existing condition or charge you more.
To be eligible for Pennsylvania Medicaid, you must be a resident of the state of Pennsylvania, a U.S. national, citizen, permanent resident, or legal alien, in need of health care/insurance assistance, whose financial situation would be characterized as low income or very low income.
Health insurance companies cannot refuse coverage or charge you more just because you have a pre-existing condition that is, a health problem you had before the date that new health coverage starts.
Individual monthly income limit $1,426. Married couple monthly income limit $1,923. Individual resource limit $7,730. Married couple resource limit $11,600.
Conditions for Exclusion HIPAA did allow insurers to refuse to cover pre-existing medical conditions for up to the first 12 months after enrollment, or 18 months in the case of late enrollment.