Pennsylvania Acknowledgment of Receipt of COBRA Notice
Description
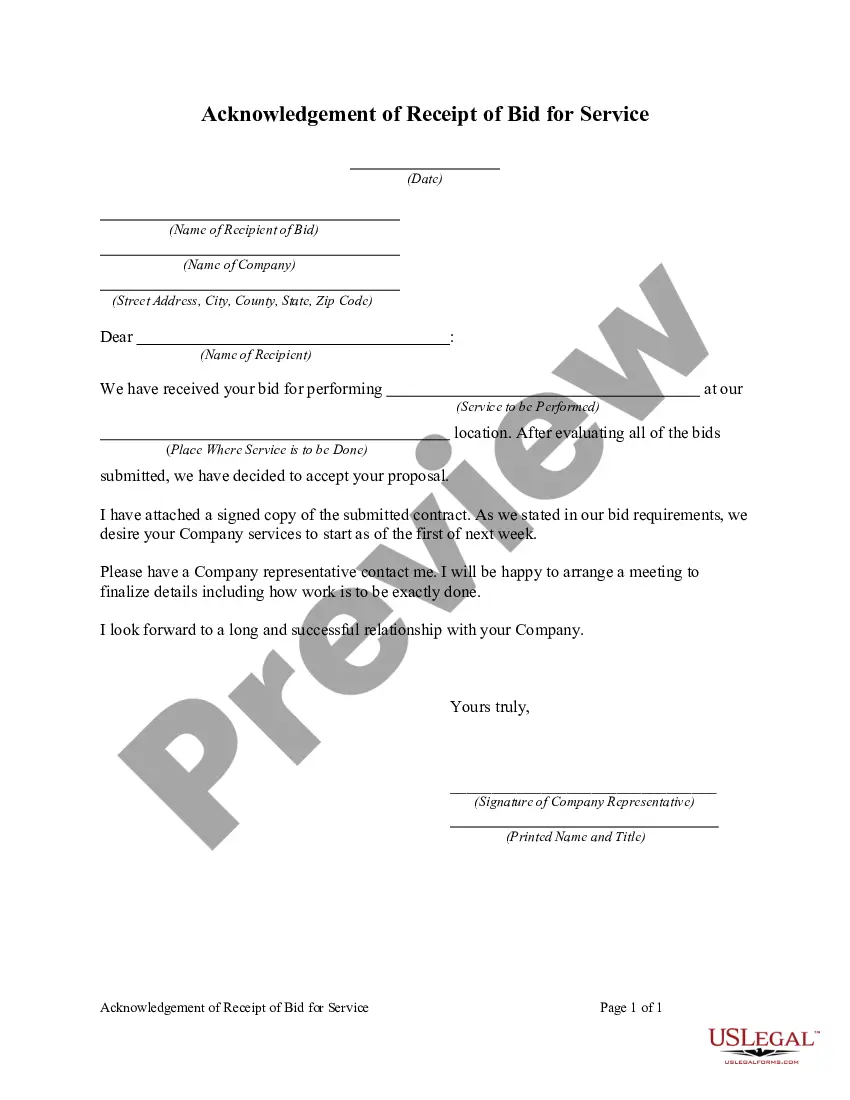
How to fill out Acknowledgment Of Receipt Of COBRA Notice?
You can invest time online seeking the legal document template that meets the federal and state requirements you desire.
US Legal Forms offers thousands of legal templates that can be reviewed by specialists.
It is easy to download or create the Pennsylvania Acknowledgment of Receipt of COBRA Notice from our service.
If desired, use the Preview button to view the document template as well.
- If you possess a US Legal Forms account, you can Log In and click on the Obtain button.
- After that, you can complete, modify, print, or sign the Pennsylvania Acknowledgment of Receipt of COBRA Notice.
- Every legal document template you purchase is yours eternally.
- To get another copy of any purchased template, visit the My documents tab and click on the corresponding button.
- If you are using the US Legal Forms website for the first time, follow the straightforward instructions provided below.
- First, ensure that you have chosen the correct document template for the area/city of your preference.
- Review the template description to confirm you have selected the appropriate document.
Form popularity
FAQ
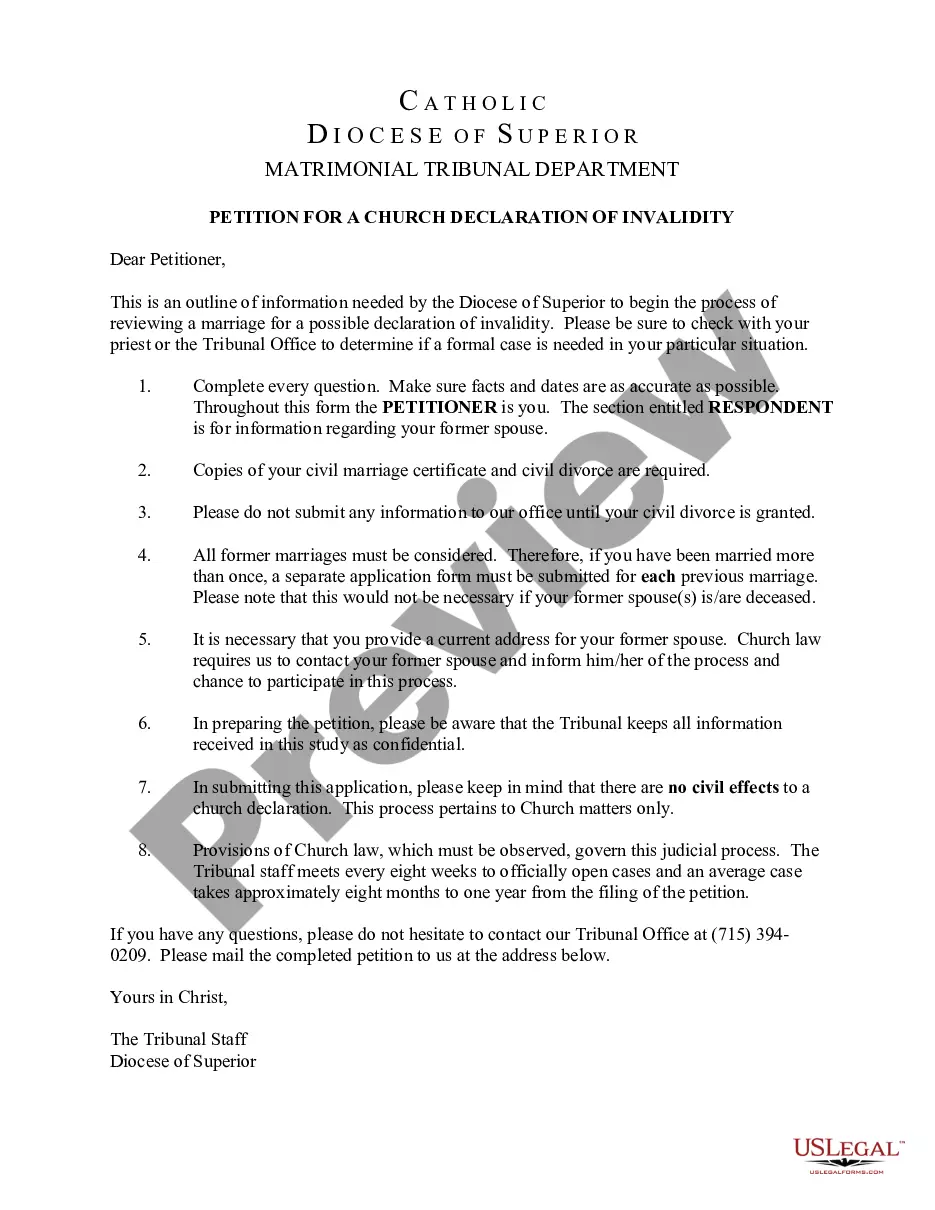
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
COBRA continuation coverage notices are documents that explain employees' rights under the Consolidated Omnibus Budget Reconciliation Act of 1985. These documents generally contain a variety of information, including the following: The name of the health insurance plan.
When does COBRA continuation coverage startCOBRA is always effective the day after your active coverage ends. For most, active coverage terminates at the end of a month and COBRA is effective on the first day of the next month.
In addition, employers can provide COBRA notices electronically (via email, text message, or through a website) during the Outbreak Period, if they reasonably believe that plan participants and beneficiaries have access to these electronic mediums.
If You Do Not Receive Your COBRA PaperworkReach out to the Human Resources Department and ask for the COBRA Administrator. They may use a third-party administrator to handle your enrollment. If the employer still does not comply you can call the Department of Labor at 1-866-487-2365.
The federal COBRA law allows employees at larger businesses (20 or more employees) to purchase continuation health coverage after they leave employment for 18 months (or, in some cases, 36 months) after their employment ends.
The COBRA Notice informs the qualified beneficiary of their rights under COBRA law, and the form allows the qualified beneficiary to elect COBRA coverage to continue enrollment in benefits.
Pennsylvania's Mini-COBRA applies to employees of smaller businesses (2-19 employees), though it only allows for 9 months of coverage.
If you are laid-off or quit your job, COBRA will pay your health care costs up until 18 months following termination of employment. However, you must have both dental and vision coverage while employed if you want them covered by Cobra after quitting.
COBRA costs an average of $599 per month. An Obamacare plan of similar quality costs $462 per monthbut 94% of people on HealthSherpa qualify for government subsidies, bringing the average cost down to $48 per month.