Oregon Affidavit of No Coverage by Another Group Health Plan
Description
How to fill out Affidavit Of No Coverage By Another Group Health Plan?
If you desire to complete, acquire, or print legal document templates, utilize US Legal Forms, the largest collection of legal forms available online.
Take advantage of the website's straightforward and user-friendly search to find the documents you need. Numerous templates for business and personal purposes are categorized by sectors and states, or keywords.
Use US Legal Forms to obtain the Oregon Affidavit of No Coverage by Another Group Health Plan in just a few clicks.
Each legal document template you obtain is yours for a lifetime. You will have access to every form you saved within your account. Click the My documents section and select a form to print or download again.
Complete and download, and print the Oregon Affidavit of No Coverage by Another Group Health Plan with US Legal Forms. There are millions of professional and state-specific forms you can use for your business or personal needs.
- If you are already a US Legal Forms customer, Log In to your account and then click the Download button to get the Oregon Affidavit of No Coverage by Another Group Health Plan.
- You can also access forms you previously saved in the My documents section of your account.
- If you are using US Legal Forms for the first time, follow the steps below.
- Step 1. Ensure you have selected the form for the appropriate state/country.
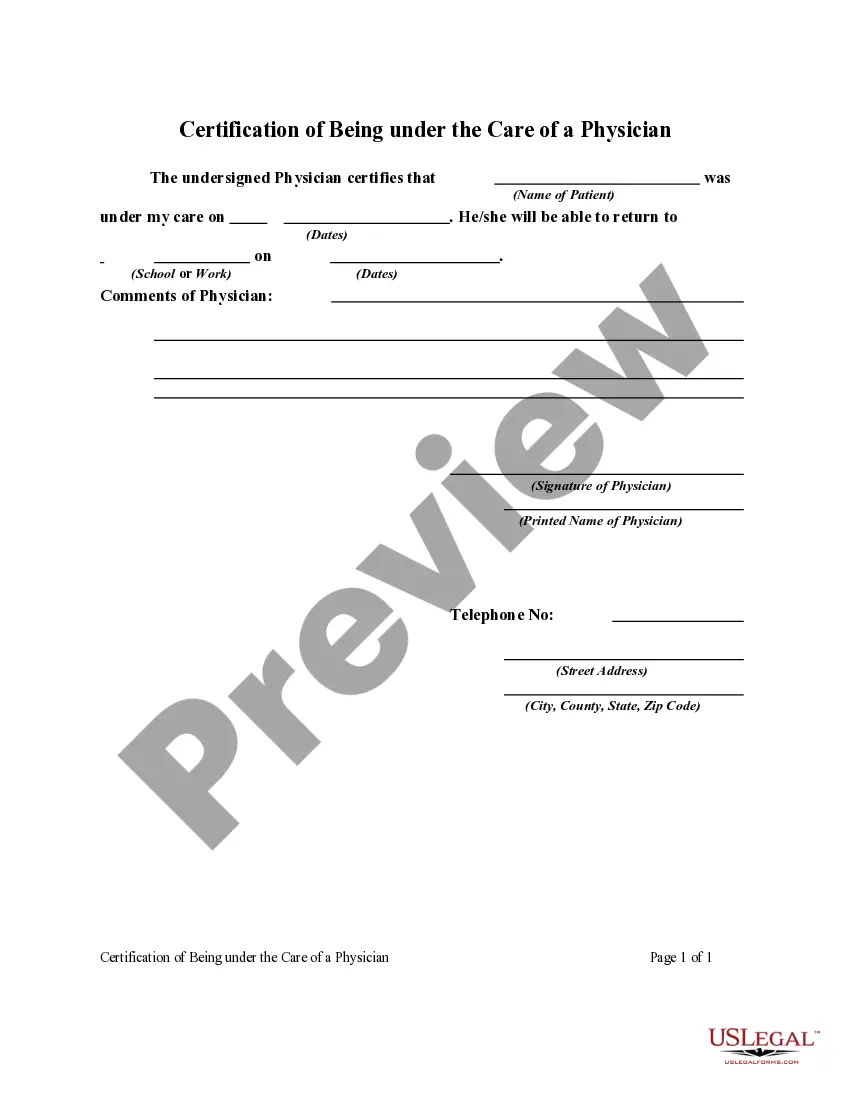
- Step 2. Use the Review option to examine the content of the form. Don’t forget to read the description.
- Step 3. If you are not satisfied with the form, use the Search field at the top of the screen to find other templates in the legal form category.
- Step 4. Once you have found the form you need, click the Get now button. Choose the pricing plan you prefer and enter your details to register for an account.
- Step 5. Process the payment. You can use your credit card or PayPal account to complete the transaction.
- Step 6. Pick the format of the legal form and download it to your device.
- Step 7. Fill out, revise, and print or sign the Oregon Affidavit of No Coverage by Another Group Health Plan.
Form popularity
FAQ
Group insurance is a type of insurance plan that covers a number of people in the same contract. Such a plan provides the same level of insurance coverage to all members of a group irrespective of their age, gender, occupation or socio-economic status.
The term continuation coverage refers to the extended coverage provided under the group benefit plan in which an eligible employee or eligible dependent is currently enrolled.
Group Insurance health plans provide coverage to a group of members, usually comprised of company employees or members of an organization. Group health members usually receive insurance at a reduced cost because the insurer's risk is spread across a group of policyholders.
What Is Group Coverage? Group medical coverage refers to a single policy issued to a group (typically a business with employees, although there are other kinds of groups that can get coverage) that covers all eligible employees and sometimes their dependents.
Group plans are chosen by the employer to accommodate the needs of everyone being covered at the company, so they typically offer as many providers, locations, and services as possible. Individual plans are chosen by the employee for the employee, not based on the needs of coworkers.
A dependent is a person who is eligible to be covered by you under these plans.
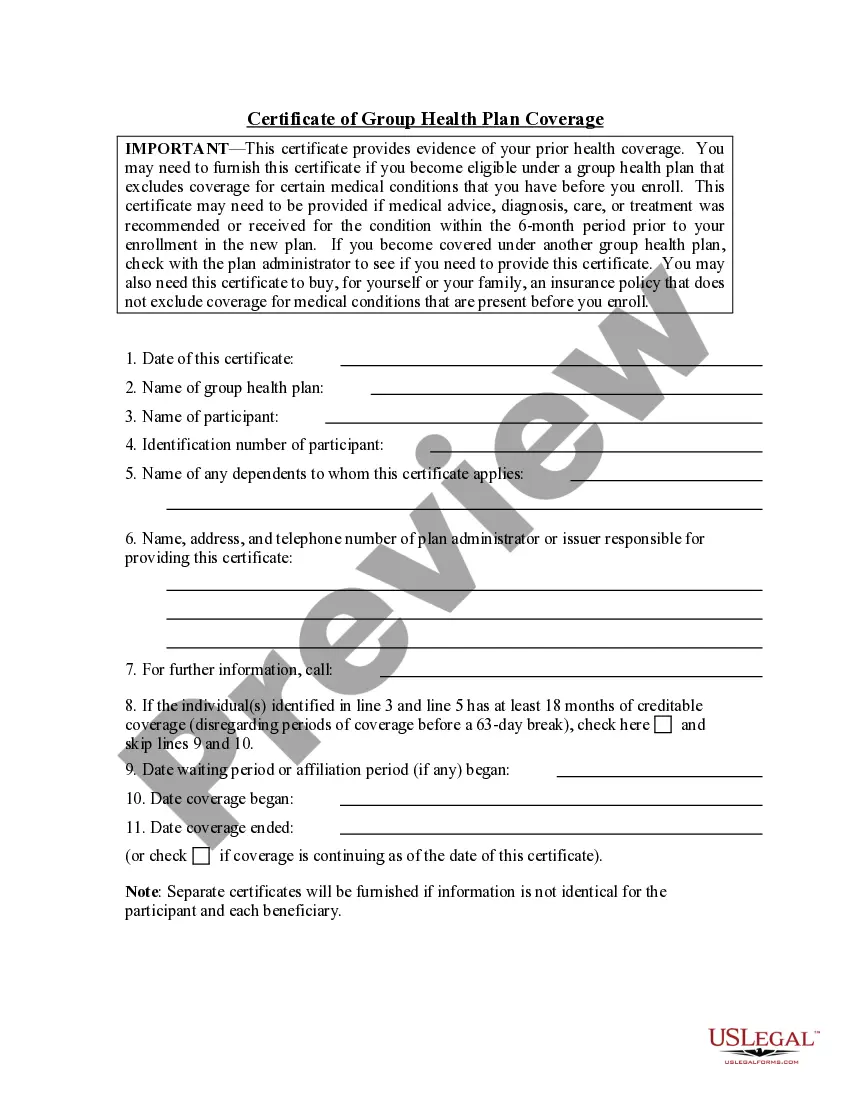
The primary purpose of the certificate is to show the amount of creditable coverage that you had under a group health plan or other health insurance coverage, because this can reduce or eliminate the length of time that any pre-existing condition clause in a new plan otherwise might apply to you.
COBRA generally requires that group health plans sponsored by employers with 20 or more employees in the prior year offer employees and their families the opportunity for a temporary extension of health coverage (called continuation coverage) in certain instances where coverage under the plan would otherwise end.
Continuation coverage allows someone who recently lost their employer-based health coverage to continue their current insurance policy as long as they pay the full monthly premiums.