New Jersey Notice from Employer to Employee Regarding Early Termination of Continuation Coverage
Description
How to fill out Notice From Employer To Employee Regarding Early Termination Of Continuation Coverage?
You can spend numerous hours online attempting to locate the valid document template that aligns with the federal and state standards you require. US Legal Forms provides thousands of valid forms that can be assessed by professionals.
You can effortlessly download or print the New Jersey Notice from Employer to Employee Regarding Early Termination of Continuation Coverage from your account.
If you possess a US Legal Forms account, you can Log In and click on the Download button. Subsequently, you can complete, modify, print, or sign the New Jersey Notice from Employer to Employee Regarding Early Termination of Continuation Coverage. Every valid document format you obtain is yours permanently.
Complete the transaction. You can use your credit card or PayPal account to purchase the valid document. Choose the format of the document and download it to your device. Make alterations to your document if possible. You can complete, modify, sign, and print the New Jersey Notice from Employer to Employee Regarding Early Termination of Continuation Coverage. Download and print thousands of document templates using the US Legal Forms website, which offers the largest selection of valid forms. Utilize professional and state-specific templates to handle your business or personal needs.
- To obtain another copy of a purchased form, navigate to the My documents section and click on the appropriate button.
- If you are using the US Legal Forms website for the first time, follow the simple guidelines below.
- First, ensure you have selected the correct document template for the region/city of your choice. Refer to the form description to confirm you have chosen the right form.
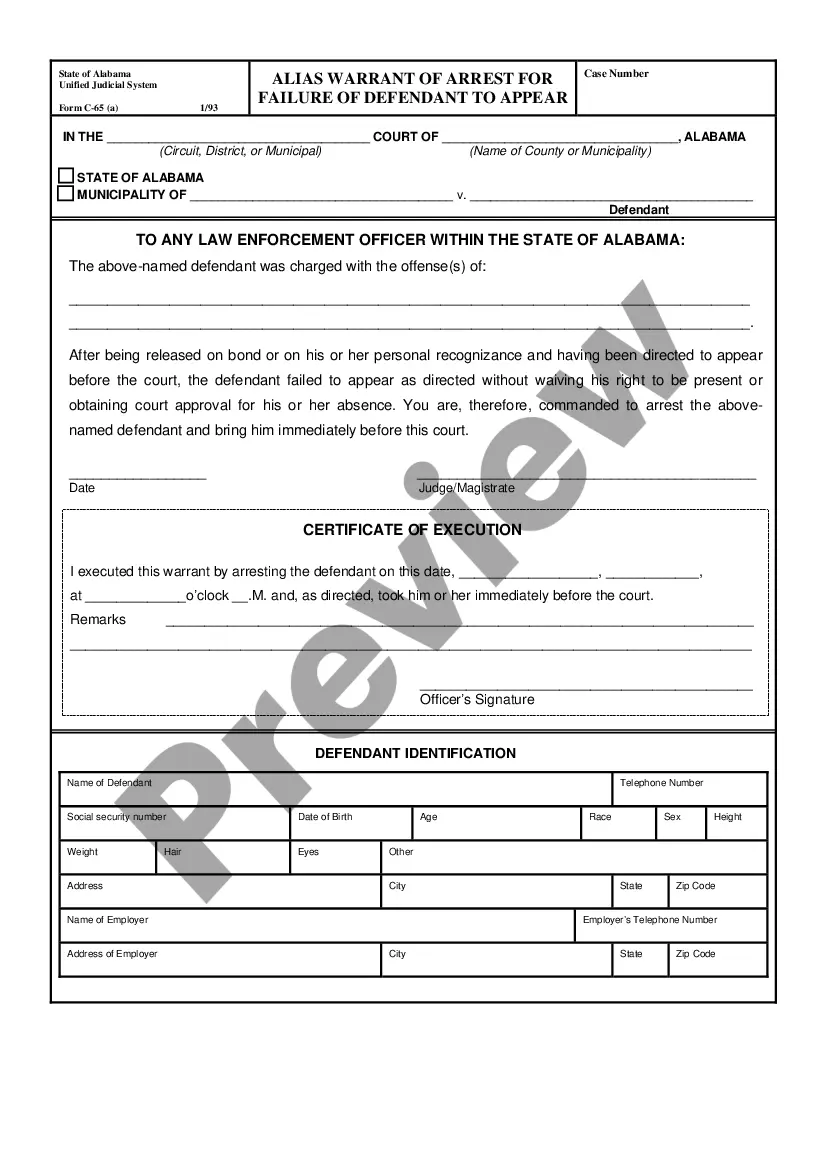
- If available, utilize the Review button to examine the document template as well.
- If you wish to find another version of the document, utilize the Search field to locate the template that fulfills your needs and requirements.
- Once you have found the desired template, click Purchase now to proceed.
- Select the pricing plan you prefer, enter your credentials, and register for an account on US Legal Forms.
Form popularity
FAQ
In addition, employers can provide COBRA notices electronically (via email, text message, or through a website) during the Outbreak Period, if they reasonably believe that plan participants and beneficiaries have access to these electronic mediums.
COBRA Notice of Early Termination of Continuation Coverage Continuation coverage must generally be made available for a maximum period (18, 29, or 36 months).
Continuation in the event of total disability New Jersey law (N.J.S.A. 17B:27-51.12 and N.J.S.A. E-32) requires that when a covered employee terminates employment due to total disability, the employee may continue coverage (including coverage for his or her dependents) under the group's health benefits plan.
Meet the Deadlines You should get a notice in the mail about your COBRA and Cal-COBRA rights. You have 60 days after being notified to sign up. If you are eligible for Federal COBRA and did not get a notice, contact your employer. If you are eligible for Cal-COBRA and did not get a notice, contact your health plan.
When a dependent makes a continuation election, he or she is entitled to continue coverage for up to 36 months.
Continuation coverage allows someone who recently lost their employer-based health coverage to continue their current insurance policy as long as they pay the full monthly premiums.
The Consolidated Omnibus Budget Reconciliation Act of 1986 (COBRA) amended the Public Health Service Act, the Internal Revenue Code and the Employee Retirement Income Security Act (ERISA) to require employers with 20 or more employees to provide temporary continuation of group health coverage in certain situations
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
COBRA is a federal law that may let you pay to stay on your employee health insurance for a limited time after your job ends (usually 18 months). You pay the full premium yourself, plus a small administrative fee. To learn about your COBRA options, contact your employer.
Initial COBRA notices must generally be provided within 14 days of the employer notifying the third-party administrator (TPA) of a qualifying event.