New Jersey Notice of Qualifying Event from Employer to Plan Administrator
Description
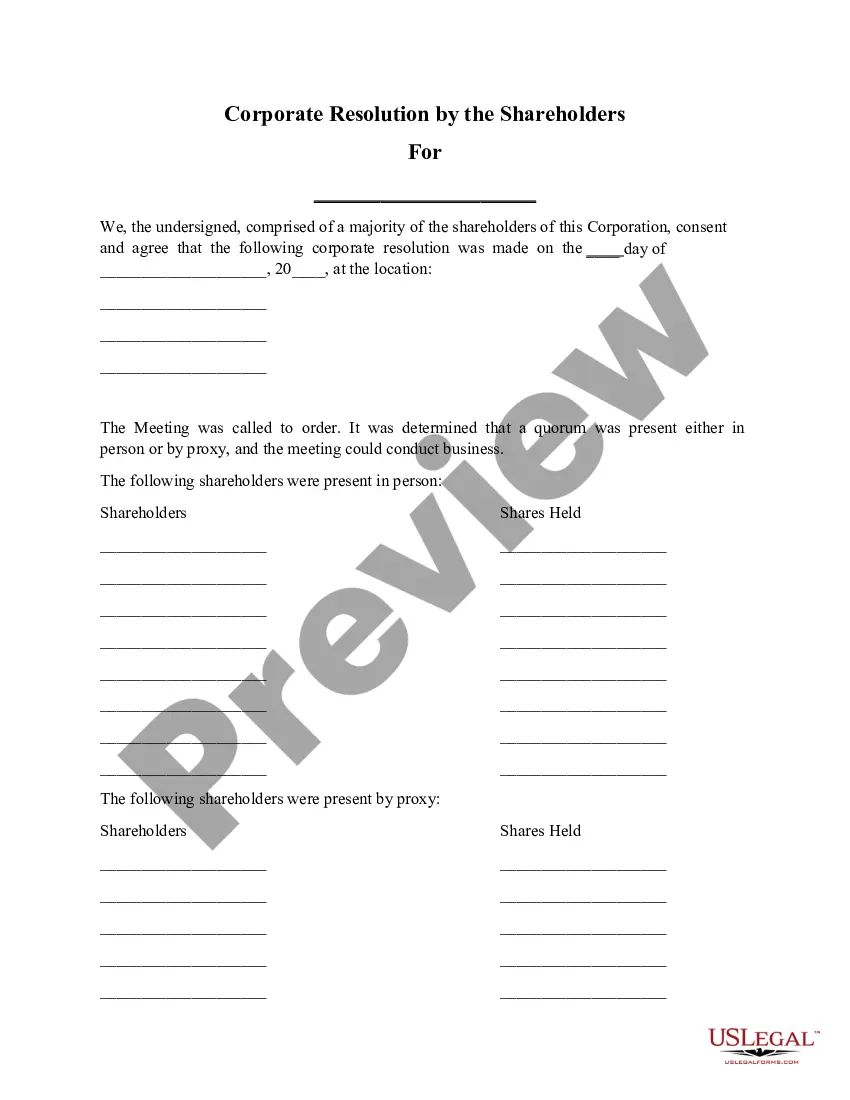
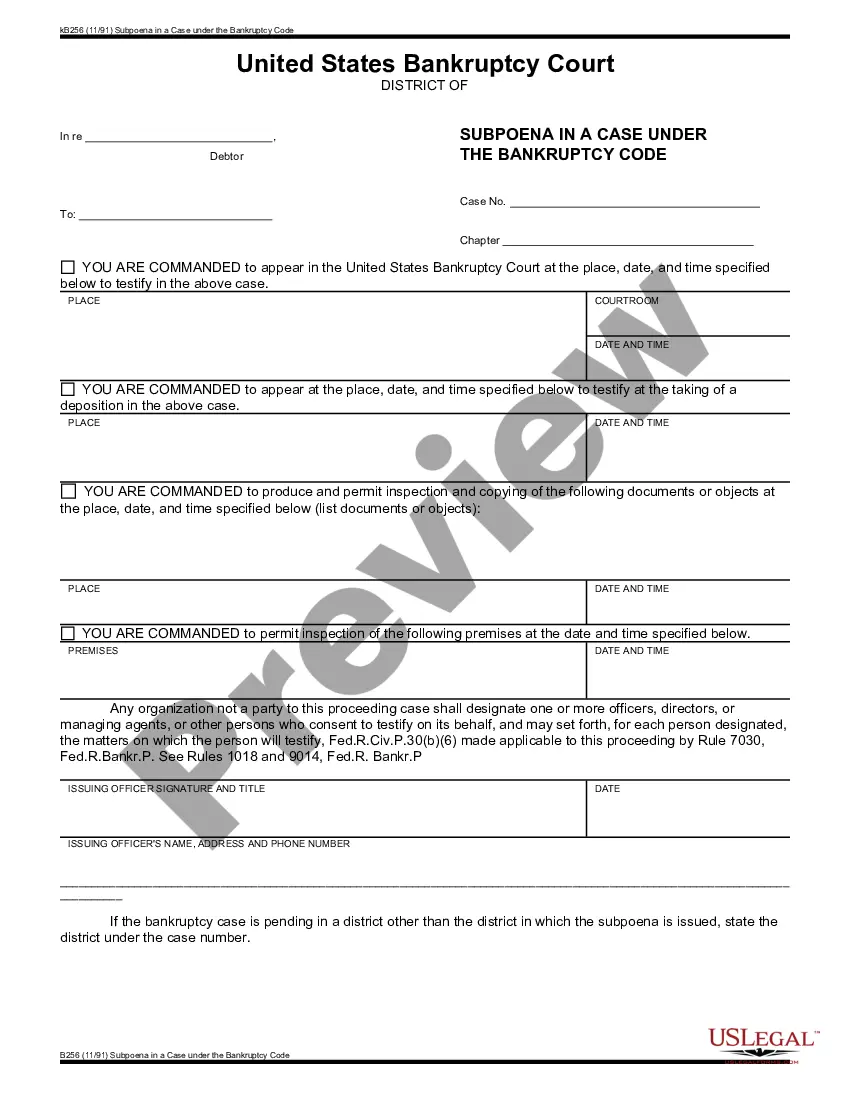
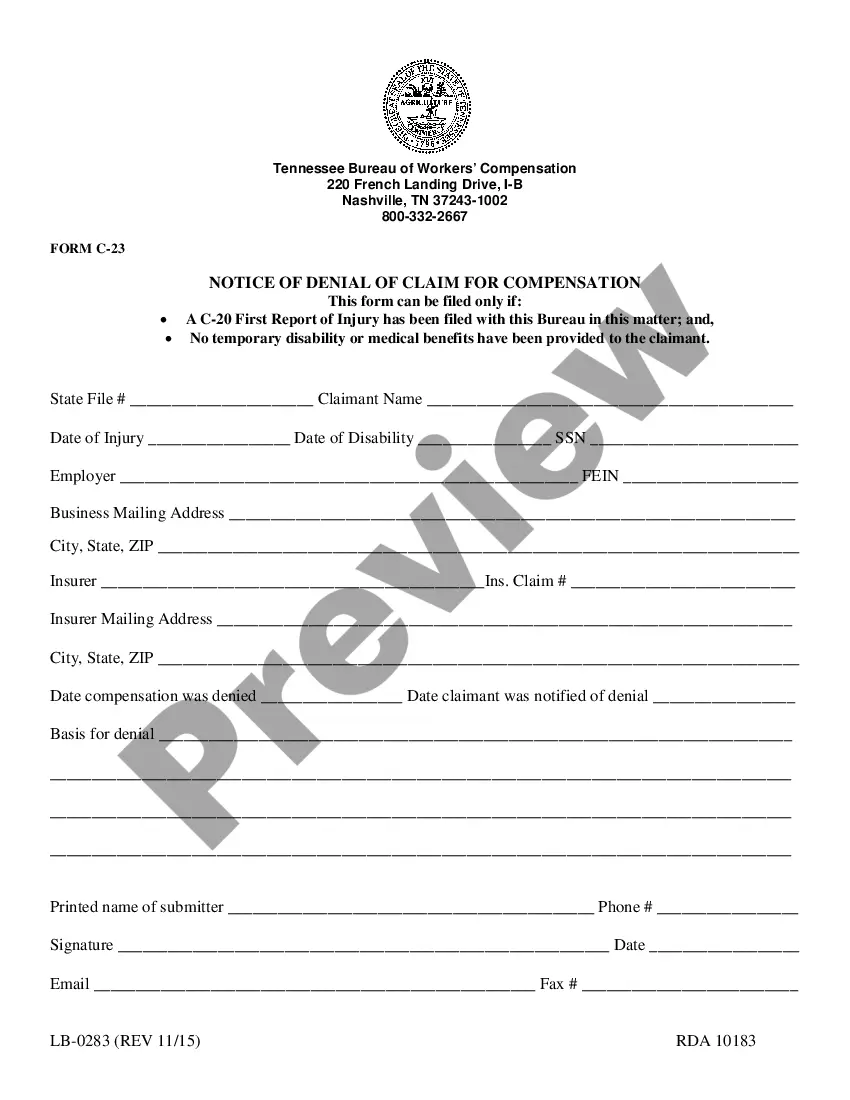
How to fill out Notice Of Qualifying Event From Employer To Plan Administrator?
If you need to be thorough, acquire, or create authorized document templates, utilize US Legal Forms, the largest selection of legal forms available online.
Take advantage of the site’s simple and user-friendly search to find the documents you require.
Different templates for business and personal purposes are organized by categories and states, or keywords.
Every legal document template you obtain is yours indefinitely. You will have access to every form you downloaded through your account.
Check the My documents section and choose a form to print or download again. Stay competitive and download, and print the New Jersey Notice of Qualifying Event from Employer to Plan Administrator with US Legal Forms. There are millions of professional and state-specific forms available for your business or personal needs.
- Use US Legal Forms to procure the New Jersey Notice of Qualifying Event from Employer to Plan Administrator in just a few clicks.
- If you are already a US Legal Forms user, Log In to your account and click on the Download option to access the New Jersey Notice of Qualifying Event from Employer to Plan Administrator.
- You can also find forms you previously downloaded in the My documents tab of your account.
- If you're using US Legal Forms for the first time, follow the instructions below.
- Step 1. Ensure you have selected the form for the correct city/state.
- Step 2. Utilize the Preview option to review the form’s details. Don’t forget to check the specifics.
- Step 3. If you are not satisfied with the form, use the Lookup section at the top of the screen to find other variations of the legal form template.
- Step 4. After identifying the form you desire, choose the Buy now option. Select your desired pricing plan and enter your credentials to register for an account.
- Step 5. Process the payment. You can use your credit card or PayPal account to complete the transaction.
- Step 6. Select the format of your legal form and download it to your device.
- Step 7. Complete, modify, and print or sign the New Jersey Notice of Qualifying Event from Employer to Plan Administrator.
Form popularity
FAQ
The last day to enroll in New Jersey health insurance typically coincides with the end of the open enrollment period, but important exceptions apply after qualifying events. In situations outlined by the New Jersey Notice of Qualifying Event from Employer to Plan Administrator, you may have a limited window for enrollment. To avoid gaps in coverage, it’s essential to be aware of these timelines and act promptly.
Losing COBRA Benefits Here's the good news: Rolling off of COBRA coverage is a qualifying event that opens a special enrollment period for you to purchase your own health coverage. And you'll have more options, flexibility and control of your health plan outside of COBRA with an individual health insurance plan.
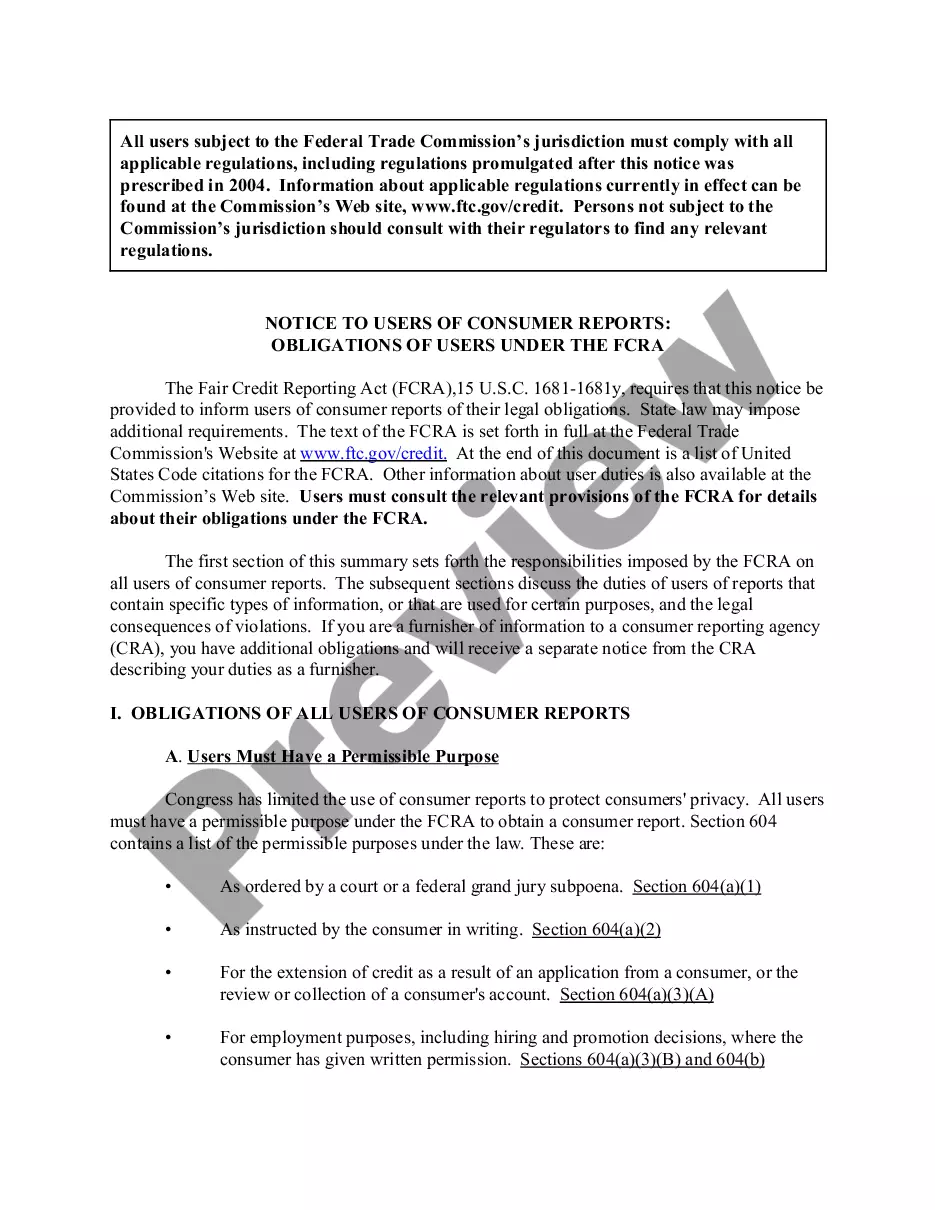
The following are qualifying events: the death of the covered employee; a covered employee's termination of employment or reduction of the hours of employment; the covered employee becoming entitled to Medicare; divorce or legal separation from the covered employee; or a dependent child ceasing to be a dependent under
The New Jersey State Health Benefits Program (SHBP) and School Employees' Health Benefits Program (SEHBP) offer employees and their covered dependents the opportunity to join a Direct Primary Care doctor's office at no additional cost.
Members enrolled in the State Health Benefits Program (SHBP) or School Employees' Health Benefits Program (SEHBP) can call 1-800-414-SHBP (7427) to access the nurse line and Horizon Health Guide services. Q.
The following are qualifying events: the death of the covered employee; a covered employee's termination of employment or reduction of the hours of employment; the covered employee becoming entitled to Medicare; divorce or legal separation from the covered employee; or a dependent child ceasing to be a dependent under
The federal Consolidated Omnibus Budget Rec- onciliation Act of 1985 (COBRA) requires that most employers sponsoring group health plans offer employees and their eligible dependents also known under COBRA as qualified beneficia- ries the opportunity to temporarily extend their group health coverage in certain
Second qualifying events may include the death of the covered employee, divorce or legal separation from the covered employee, the covered employee becoming entitled to Medicare benefits (under Part A, Part B or both), or a dependent child ceasing to be eligible for coverage as a dependent under the group health plan.
School Employees' Health Benefits Program Active Group Eligibility. Eligibility for Active Group coverage is determined by the School Employees' Health Benefits Program (SEHBP). All enrollments, changes to coverage, terminations, etc. must go through your employer. Full-time Employees.
COBRA Qualifying Event Notice The employer must notify the plan if the qualifying event is: Termination or reduction in hours of employment of the covered employee, 2022 Death of the covered employee, 2022 Covered employee becoming entitled to Medicare, or 2022 Employer bankruptcy.