New Hampshire General Notice of Preexisting Condition Exclusion
Description
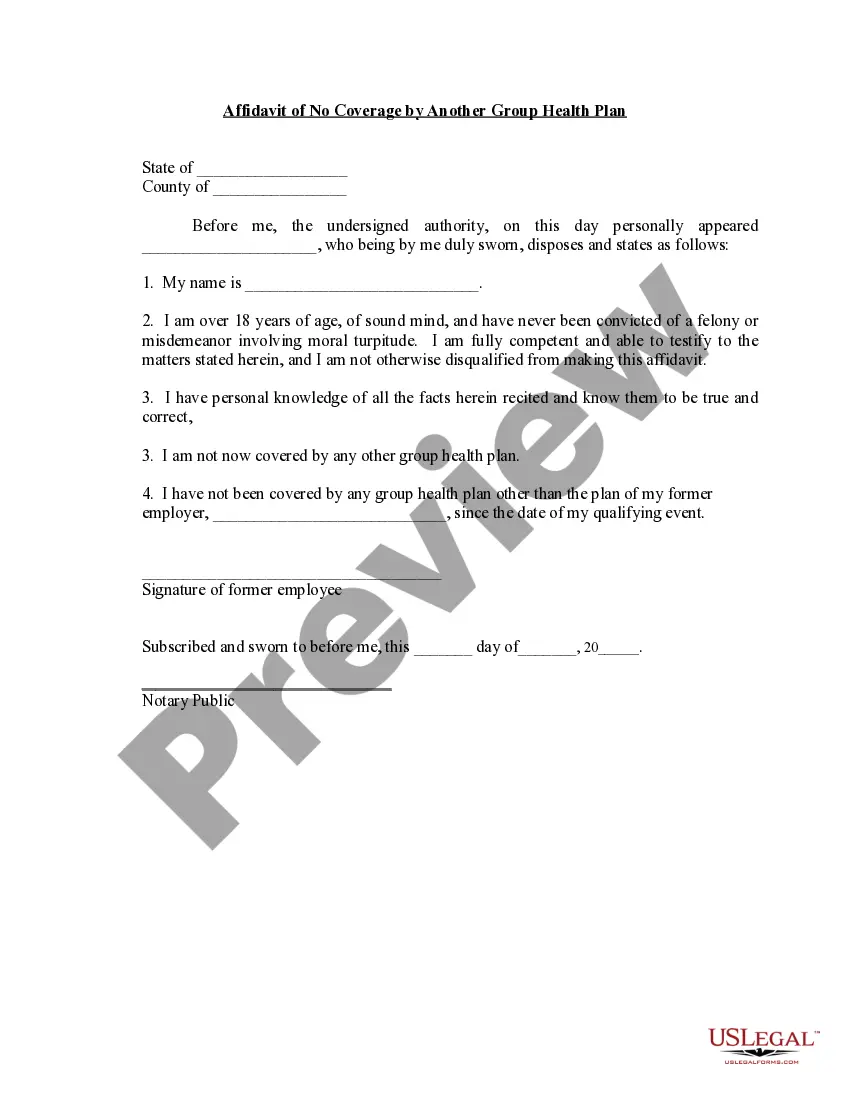
How to fill out General Notice Of Preexisting Condition Exclusion?
Locating the correct approved document format can be challenging.
Clearly, there is a range of web templates accessible online, but how can you acquire the sanctioned version you need.
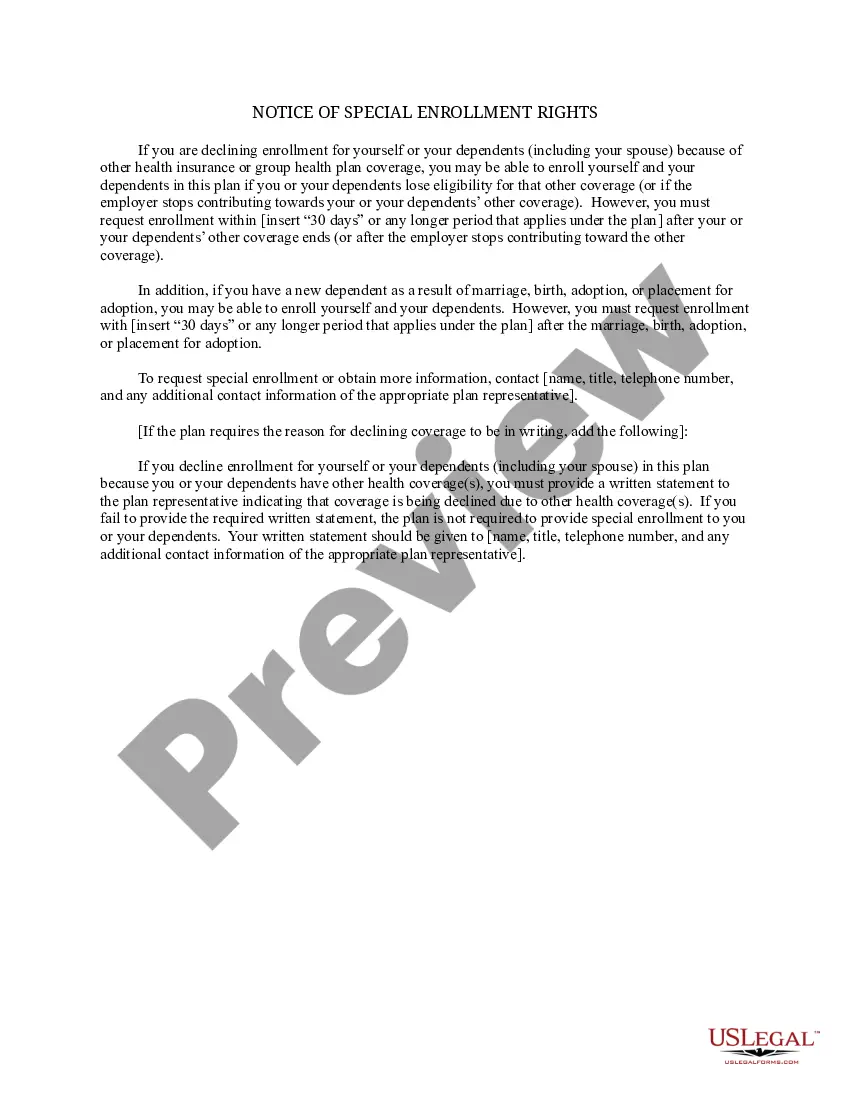
Utilize the US Legal Forms website. The service offers thousands of templates, including the New Hampshire General Notice of Preexisting Condition Exclusion, that you can utilize for business and personal purposes.
You can review the form using the Review button and read the description to confirm it is indeed the right one for you.
- All of the forms are reviewed by professionals and comply with state and federal regulations.
- If you are already registered, Log In to your account and click the Obtain button to access the New Hampshire General Notice of Preexisting Condition Exclusion.
- Use your account to browse through the legal forms you may have previously ordered.
- Visit the My documents section of your account and download another copy of the document you need.
- If you are a new user of US Legal Forms, here are simple instructions that you should follow.
- First, ensure you have selected the correct form for your city/area.
Form popularity
FAQ
The time period during which an individual policy won't pay for care relating to a pre-existing condition. Under an individual policy, conditions may be excluded permanently (known as an "exclusionary rider").
The percentage of costs of a covered health care service you pay (20%, for example) after you've paid your deductible. Let's say your health insurance plan's allowed amount for an office visit is $100 and your coinsurance is 20%. If you've paid your deductible: You pay 20% of $100, or $20.
It limits the time a new employer plan can exclude the pre-existing condition from being covered. An employer health plan can avoid covering costs of medical care for a pre-existing condition for no more than 12 months after the person is accepted into the plan.
A health problem, like asthma, diabetes, or cancer, you had before the date that new health coverage starts. Insurance companies can't refuse to cover treatment for your pre-existing condition or charge you more.
Pre-Existing Diseases (PED) Waiting Period Generally, the waiting period for pre-existing disease in health insurance plans is 1-4 years. However, the pre-existing disease waiting period varies with the health condition of the insured as well as the health insurance plan they choose.
Health insurance companies cannot refuse coverage or charge you more just because you have a pre-existing condition that is, a health problem you had before the date that new health coverage starts.
Conditions for Exclusion HIPAA did allow insurers to refuse to cover pre-existing medical conditions for up to the first 12 months after enrollment, or 18 months in the case of late enrollment.
National General Accident & Health offers short term medical coverage that helps people who are between major medical insurance to manage unexpected medical problems. Policies may cover doctor and emergency room visits as well as ambulance services, urgent care facilities and other services depending on the plan.
The National General STM plan provide an excellent base of protection. However, Short term medical (STM) plans do not cover all the services/treatments mandated under Obamacare (e.g. maternity, preventive care, outpatient mental health services and prescription drugs) and they do not cover any pre-existing conditions.
National General provides coverage across 35 states, using the Aetna network of healthcare providers. It offers good flexibility in terms of offering plans with differing levels of plan deductibles, coinsurance levels, out-of-pocket maximums and coverage period maximums.