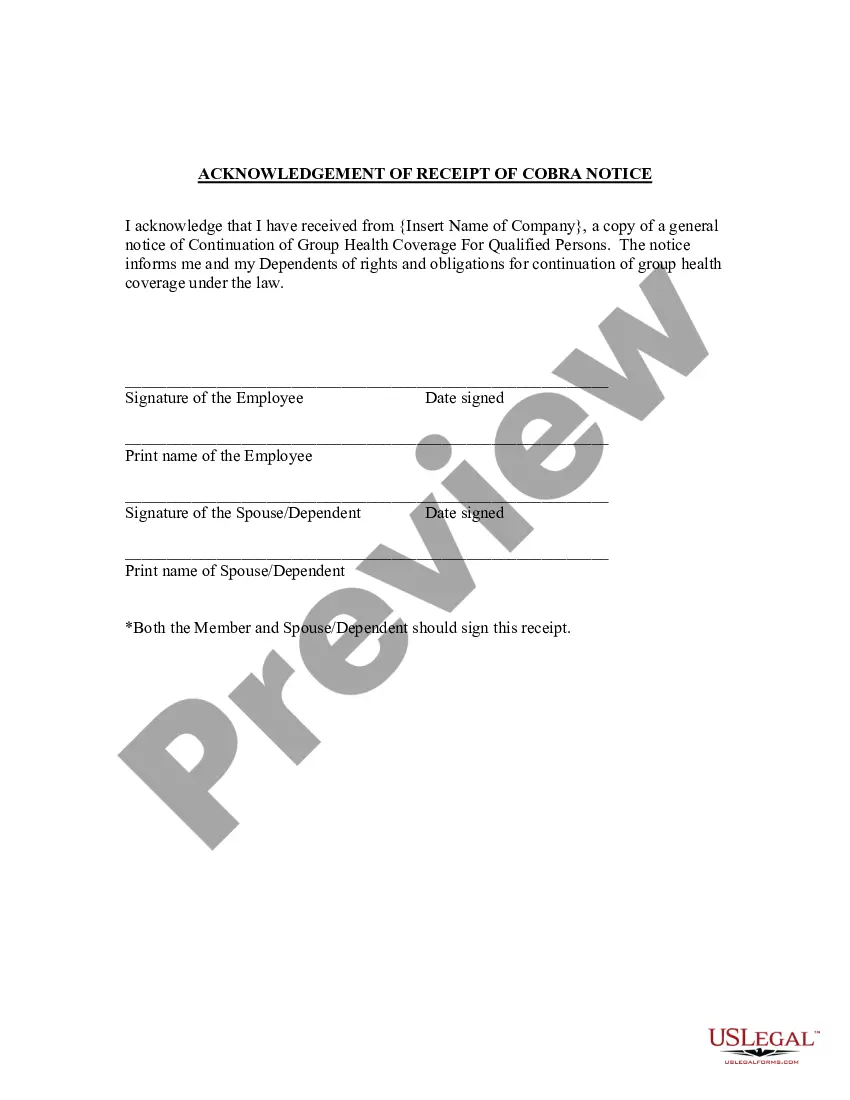
Nebraska Acknowledgment of Receipt of COBRA Notice
Description
How to fill out Acknowledgment Of Receipt Of COBRA Notice?
If you're in need of complete, acquire, or create official document templates, utilize US Legal Forms, the premier selection of legal forms available online.
Employ the site's straightforward and user-friendly search to locate the documents you require.
Various templates for corporate and personal purposes are categorized by groups and indicates, or keywords.
Each legal document template you acquire is yours indefinitely. You have access to every form you downloaded in your account.
Complete and download, and print the Nebraska Acknowledgment of Receipt of COBRA Notice with US Legal Forms. There are millions of professional and state-specific forms available for your business or personal needs.
- Utilize US Legal Forms to quickly find the Nebraska Acknowledgment of Receipt of COBRA Notice.
- If you're already a US Legal Forms user, Log In to your account and click on the Obtain button to access the Nebraska Acknowledgment of Receipt of COBRA Notice.
- You can also reach templates you've previously downloaded in the My documents tab of your account.
- If you're using US Legal Forms for the first time, follow these instructions.
- Step 1. Verify you have selected the form for the appropriate city/county.
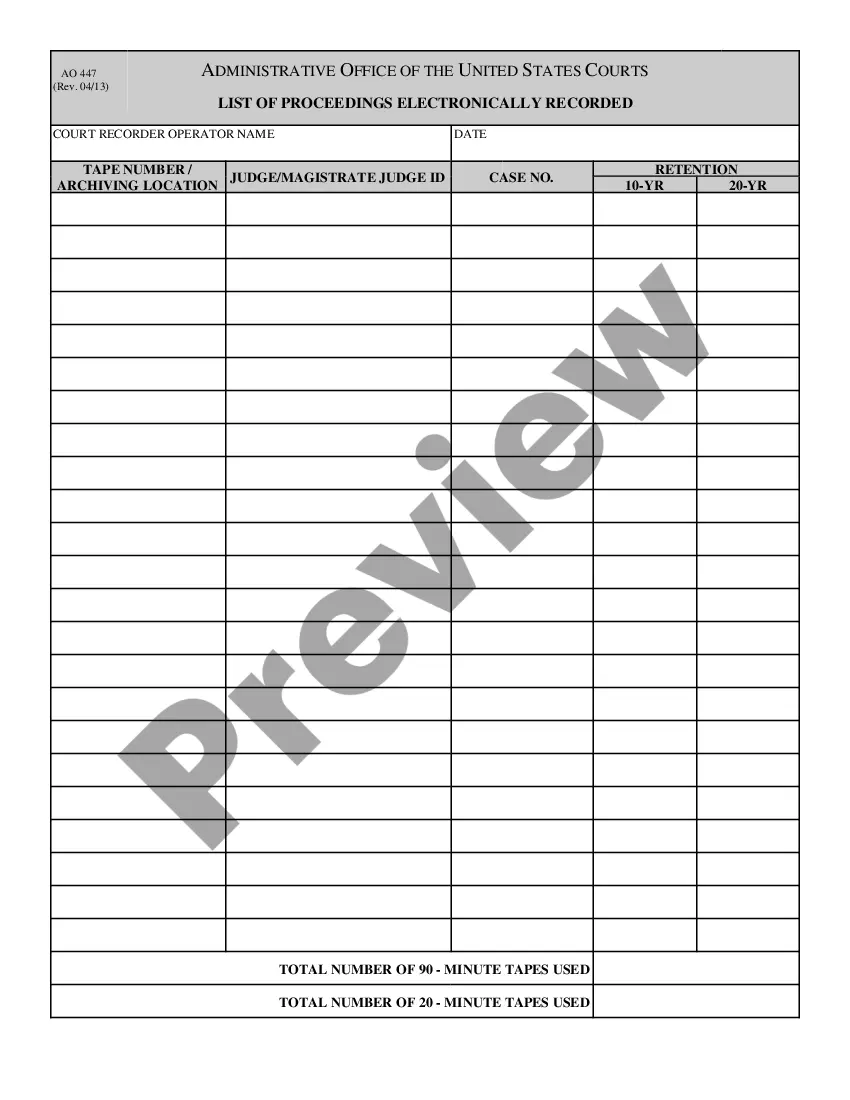
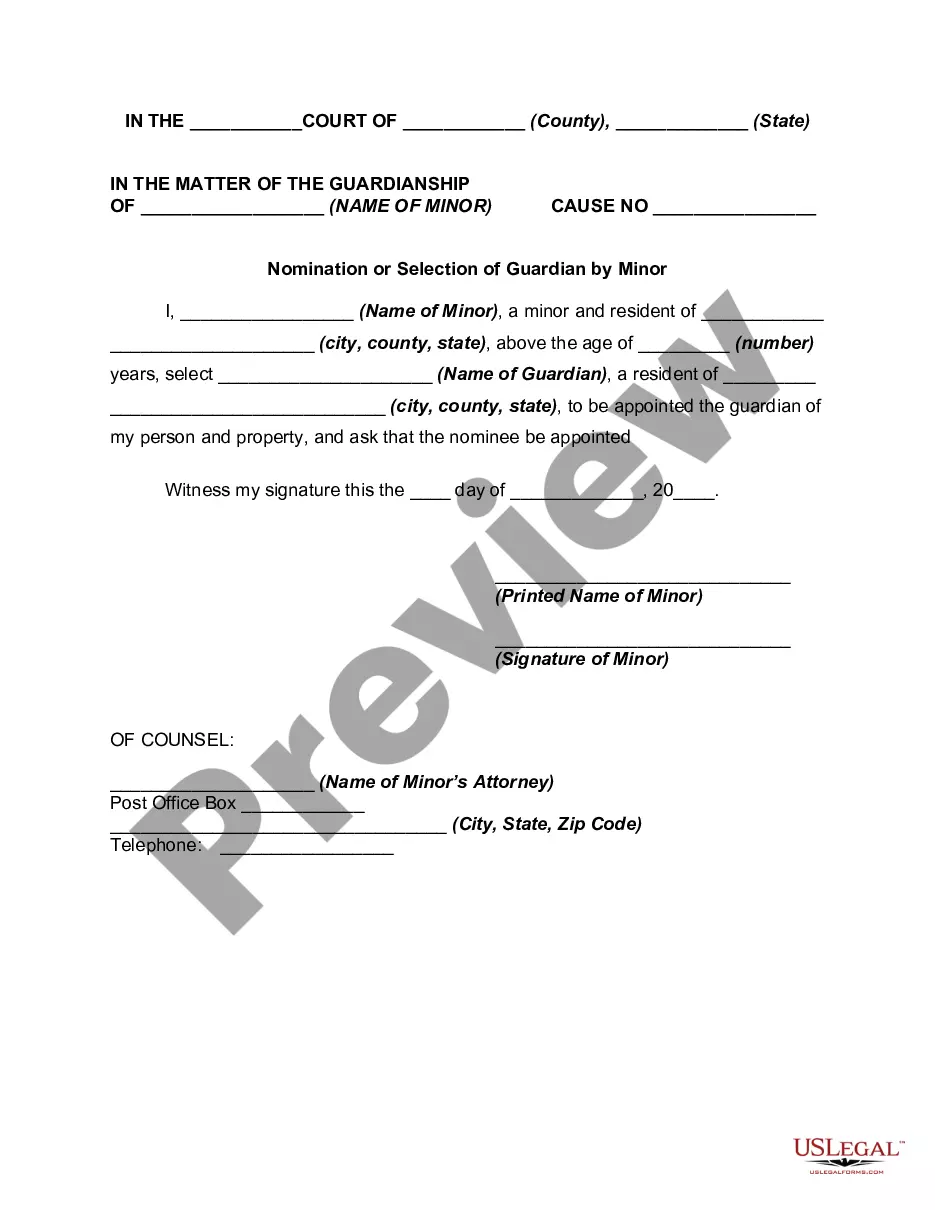
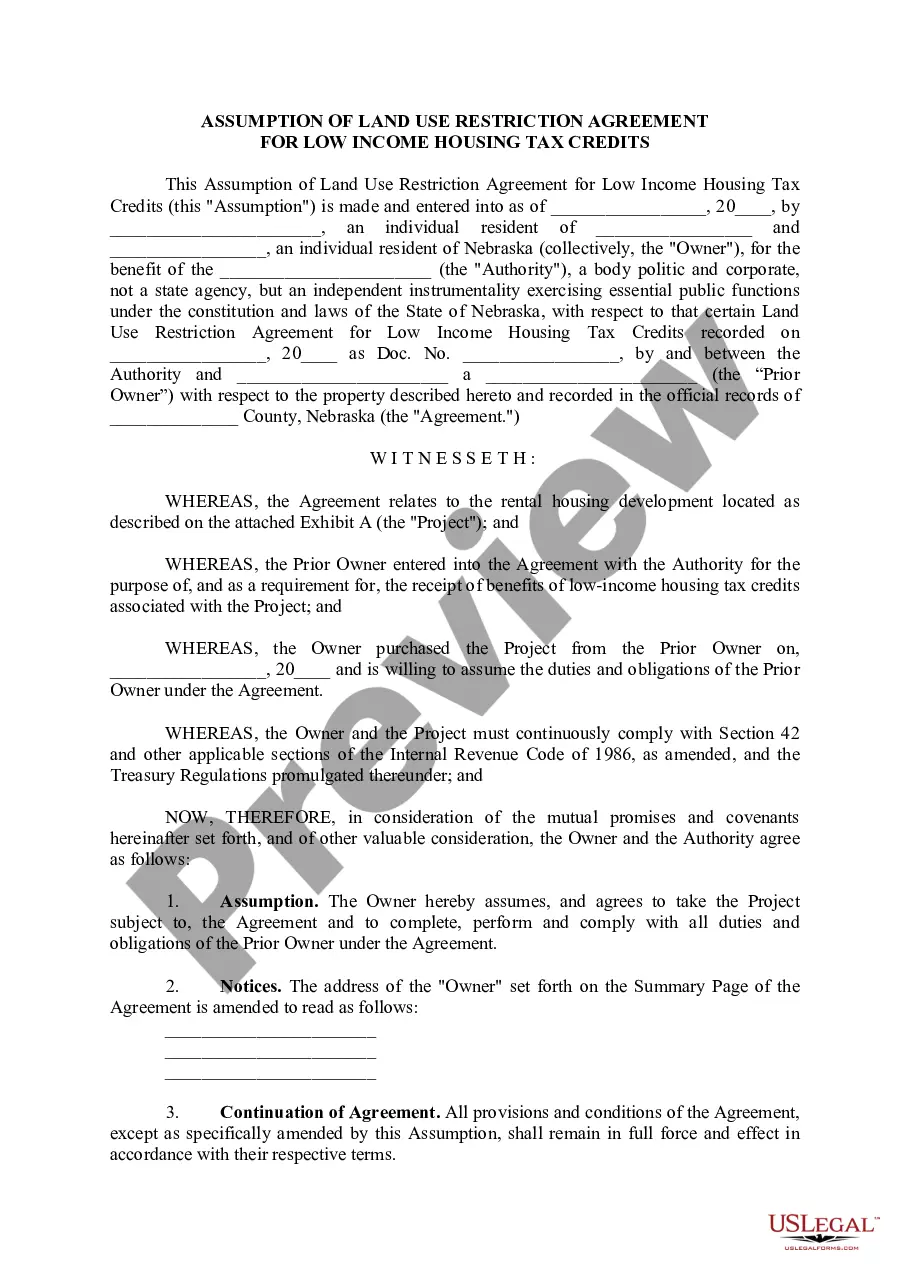
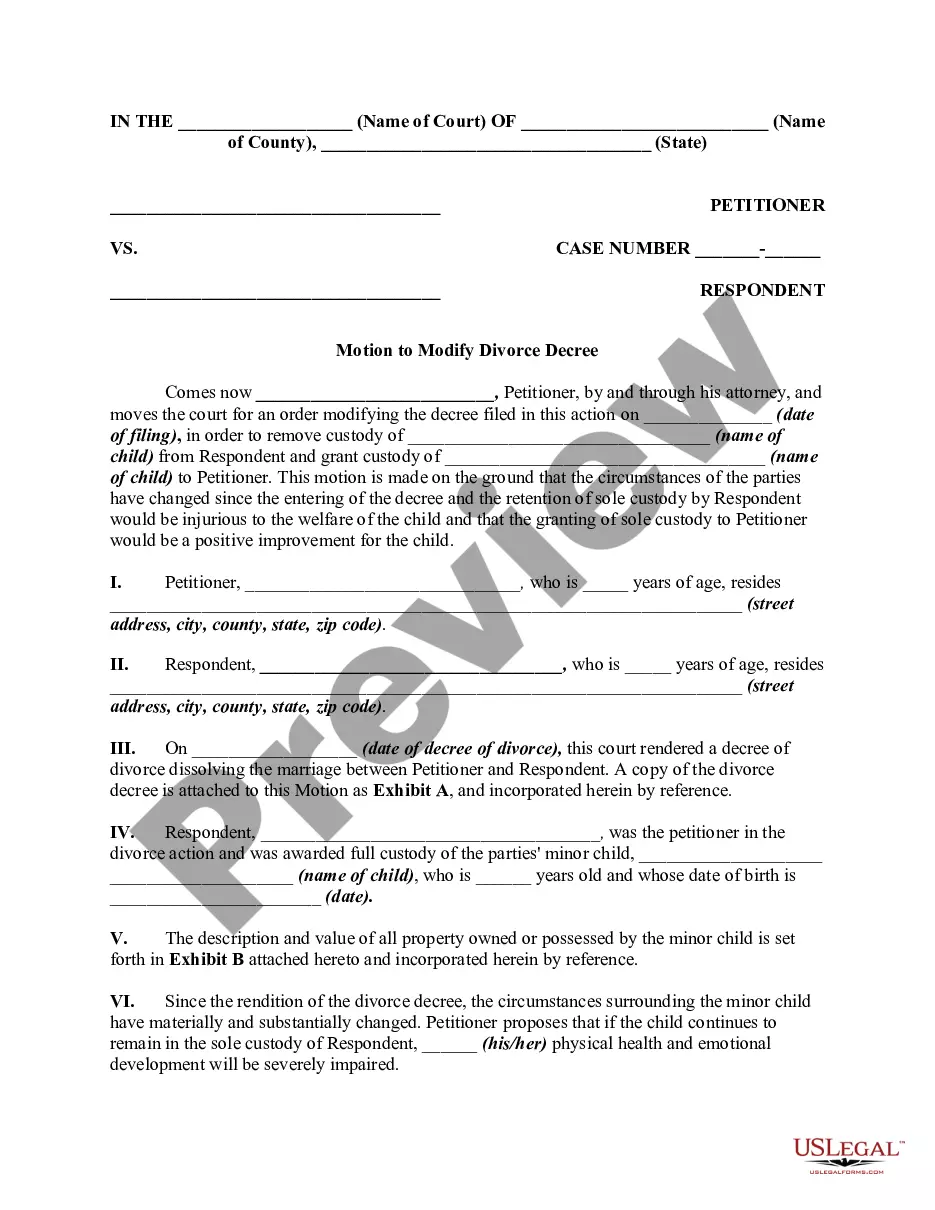
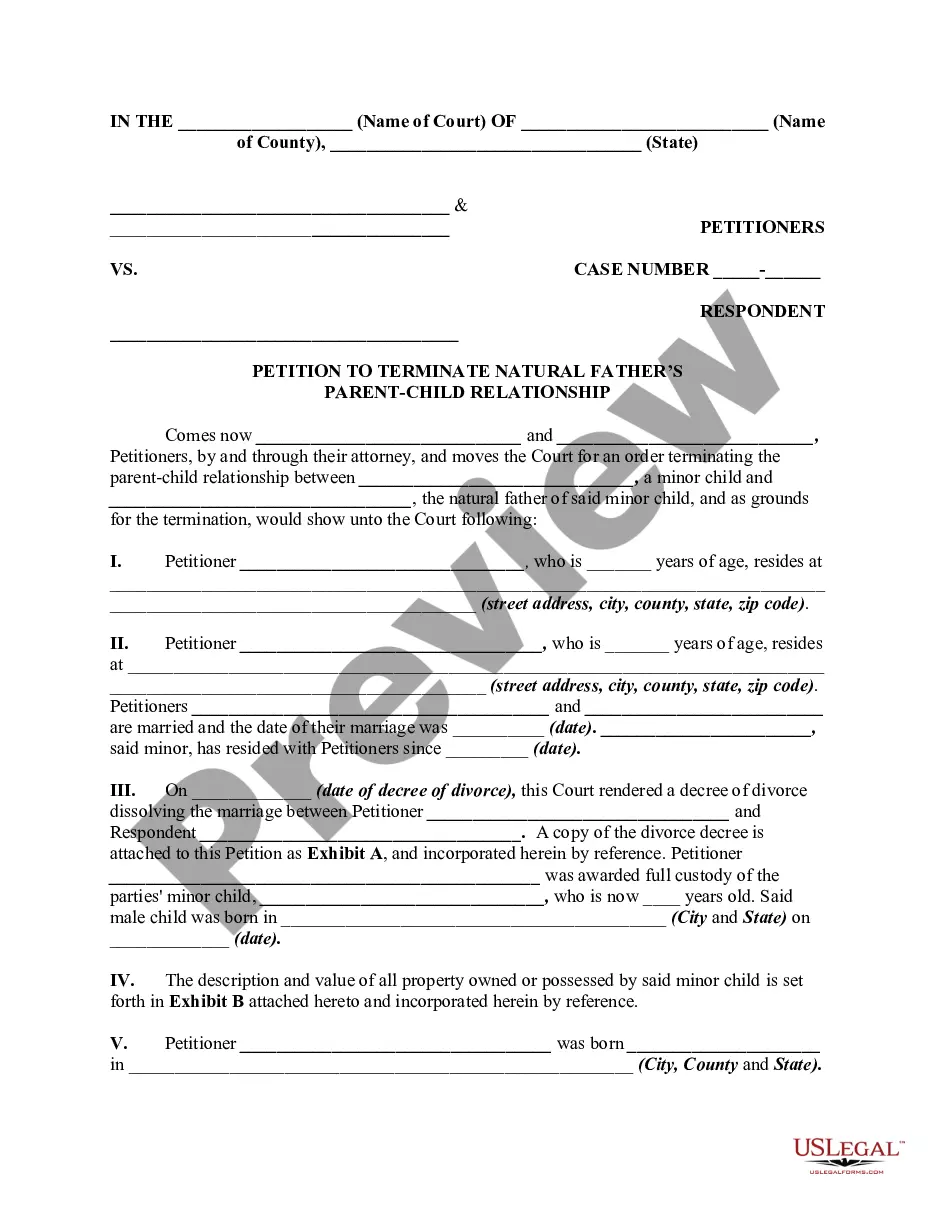
- Step 2. Use the Preview option to review the form's content. Don’t forget to check the description.
- Step 3. If you're not satisfied with the form, utilize the Search field at the top of the screen to find alternative versions of the legal form template.
- Step 4. Once you have found the form you need, click the Get now button. Choose the pricing plan you prefer and provide your credentials to register for an account.
- Step 5. Complete the payment process. You can use your credit card or PayPal account to finalize the transaction.
- Step 6. Select the format of the legal form and download it to your device.
- Step 7. Fill out, modify, and print or sign the Nebraska Acknowledgment of Receipt of COBRA Notice.
Form popularity
FAQ
Employers should send notices by first-class mail, obtain a certificate of mailing from the post office, and keep a log of letters sent. Certified mailing should be avoided, as a returned receipt with no delivery acceptance signature proves the participant did not receive the required notice.
Nebraska Makes COBRA Available For Small BusinessesWhen you elect to continue your health insurance under COBRA, you are responsible for the entire insurance premium. You will need to arrange the continuation of health insurance coverage with the former employer's HR department.
In addition, employers can provide COBRA notices electronically (via email, text message, or through a website) during the Outbreak Period, if they reasonably believe that plan participants and beneficiaries have access to these electronic mediums.
How long does it take for COBRA to kick in? With all paperwork properly submitted, your COBRA coverage should begin on the first day of your qualifying event (for example, the first day you are no longer with your employer), ensuring no gaps in your coverage.
As COBRA is the same employer-sponsored you had previously, you would need to contact the COBRA Plan Administrator. If you are unsure you that is, contact the HR Department at the business who provided the group health plan.
COBRA is a federal law about health insurance. If you lose or leave your job, COBRA lets you keep your existing employer-based coverage for at least the next 18 months. Your existing healthcare plan will now cost you more. Under COBRA, you pay the whole premium including the share your former employer used to pay.
In addition, employers can provide COBRA notices electronically (via email, text message, or through a website) during the Outbreak Period, if they reasonably believe that plan participants and beneficiaries have access to these electronic mediums.
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
Key Takeaways. COBRA provides a good option for keeping your employer-sponsored health plan for a while after you leave your job. Although, the cost can be high. Make an informed choice by looking at all your options during the 60-day enrollment period, and don't focus on the premium alone.
You may be able to keep your job-based health plan through COBRA continuation coverage. COBRA is a federal law that may let you pay to stay on your employee health insurance for a limited time after your job ends (usually 18 months). You pay the full premium yourself, plus a small administrative fee.