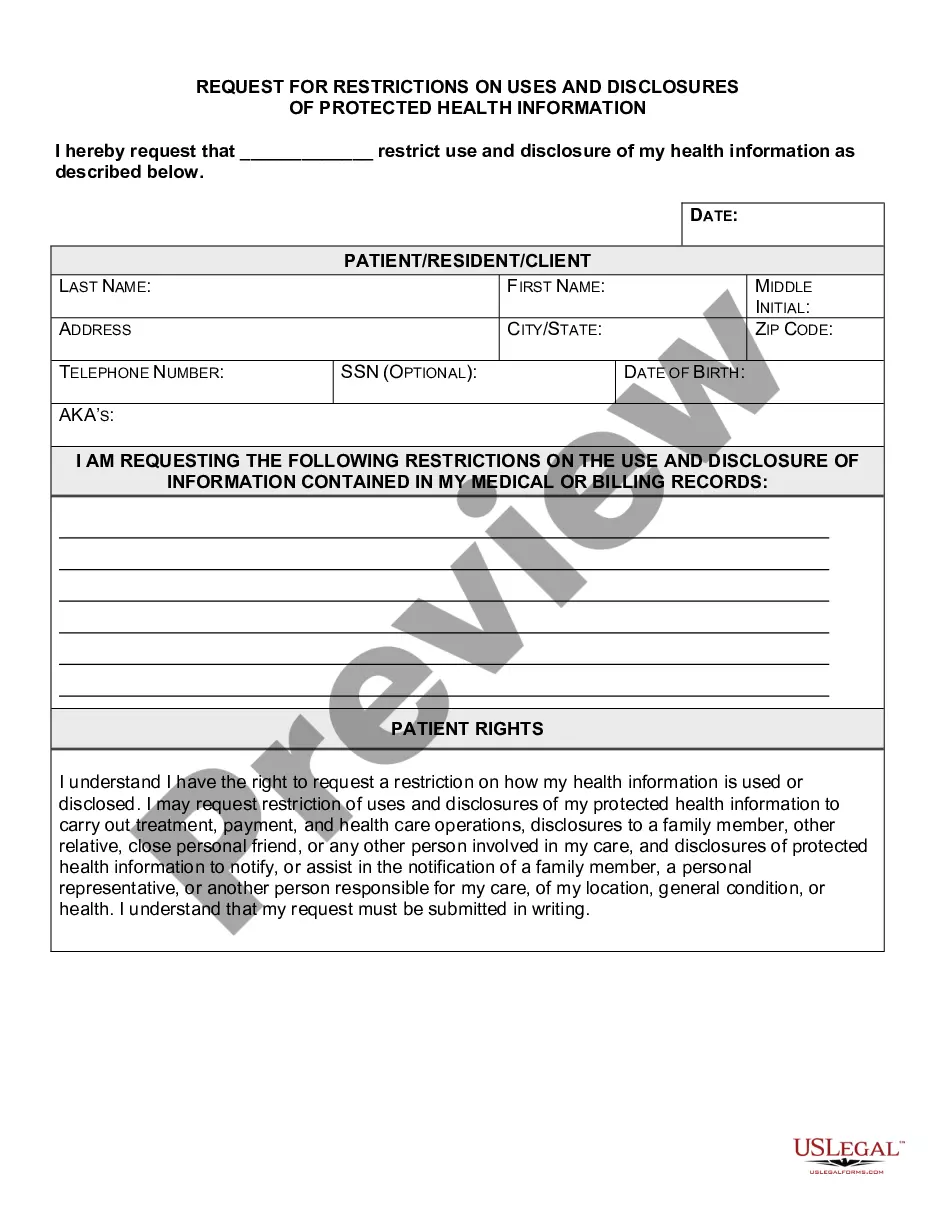
North Dakota Request for Restrictions on Uses and Disclosures of Protected Health Information
Description
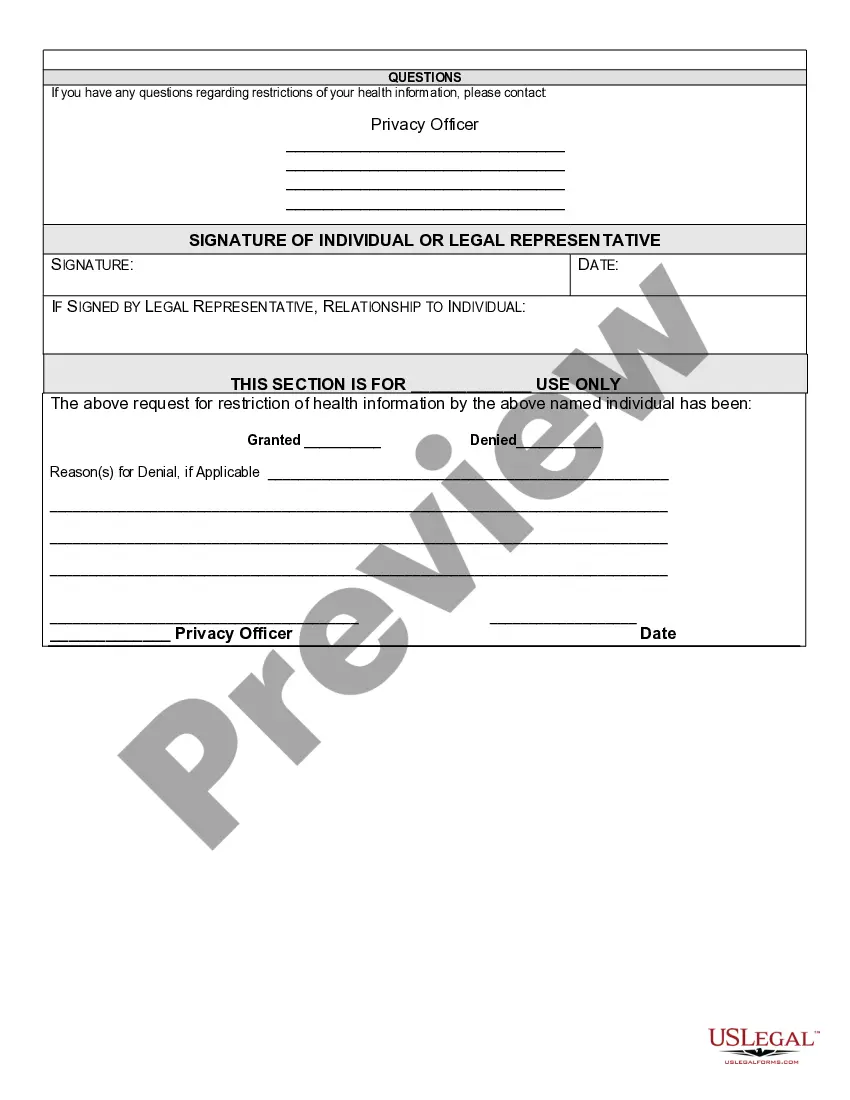
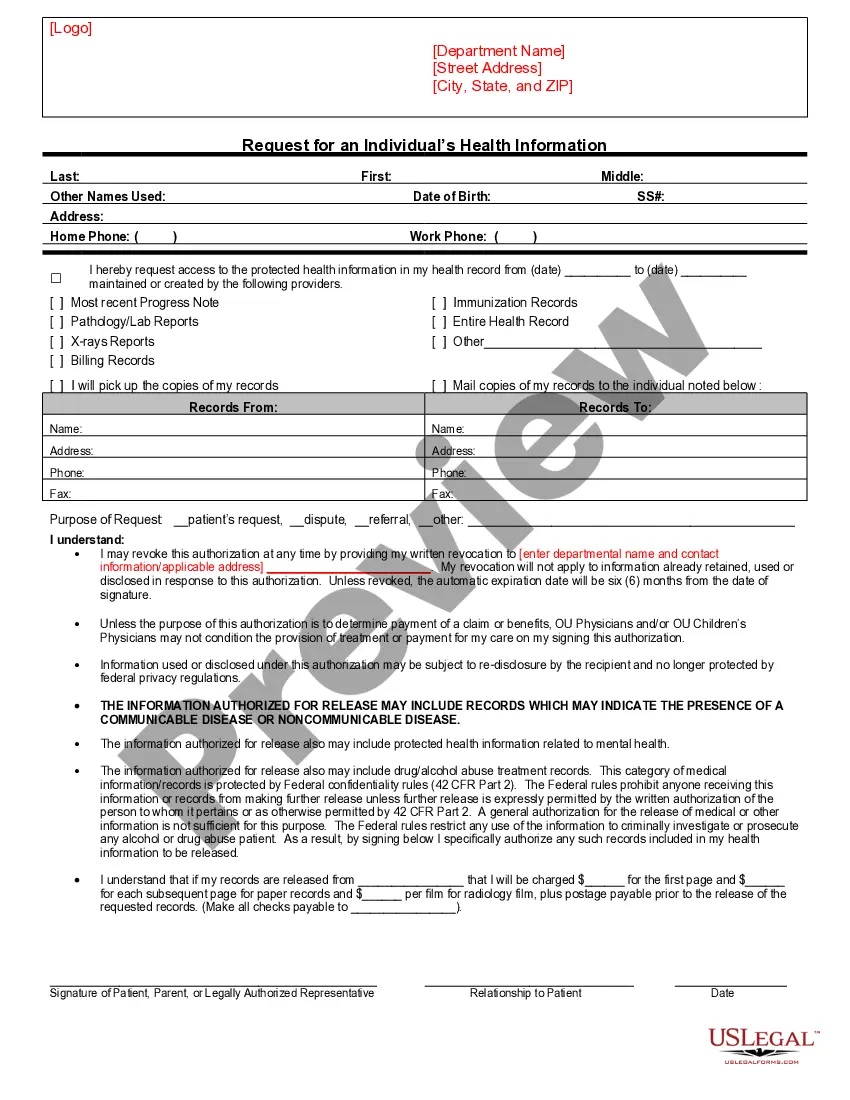
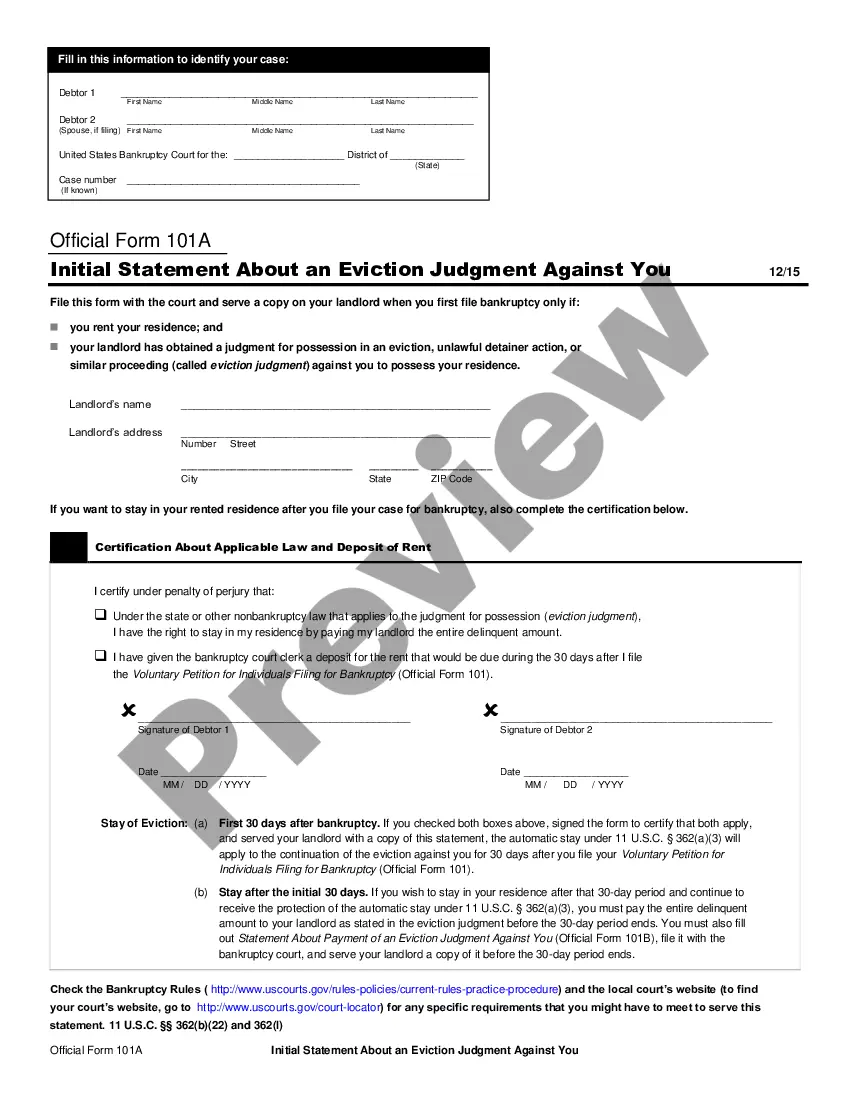
How to fill out Request For Restrictions On Uses And Disclosures Of Protected Health Information?
You might dedicate time online looking for the approved document template that fulfills the federal and state requirements you have.
US Legal Forms offers a vast array of legal templates that are examined by experts.
You can easily obtain or print the North Dakota Request for Restrictions on Uses and Disclosures of Protected Health Information through your service.
If you wish to find another version of the form, utilize the Search area to identify the template that meets your requirements and needs.
- If you already possess a US Legal Forms account, you may sign in and click on the Obtain button.
- Afterwards, you can fill out, edit, print, or sign the North Dakota Request for Restrictions on Uses and Disclosures of Protected Health Information.
- Every legal document template you buy is yours indefinitely.
- To get an additional copy of any purchased form, visit the My documents tab and click the relevant button.
- If you are using the US Legal Forms website for the first time, follow the simple instructions below.
- First, ensure that you have selected the correct document template for the state/city of your choice. Review the document description to confirm you have selected the correct template.
- If available, use the Preview button to view the document template simultaneously.
Form popularity
FAQ
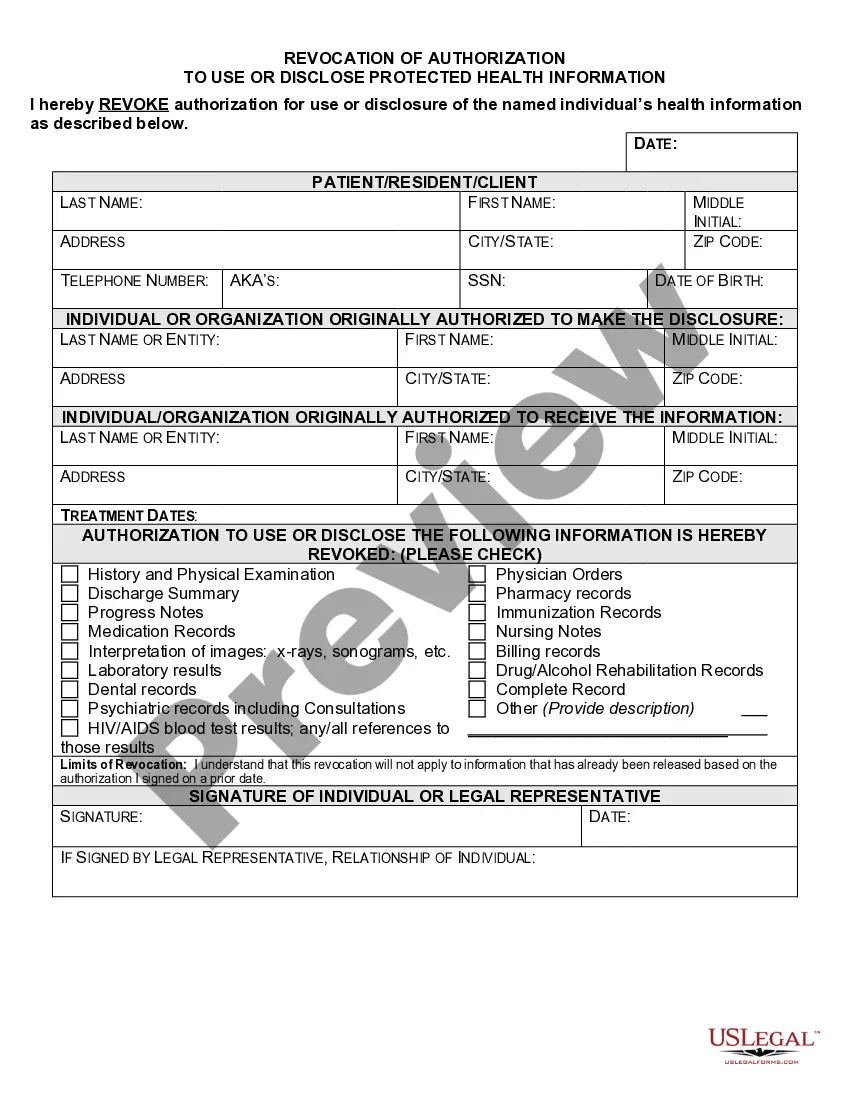
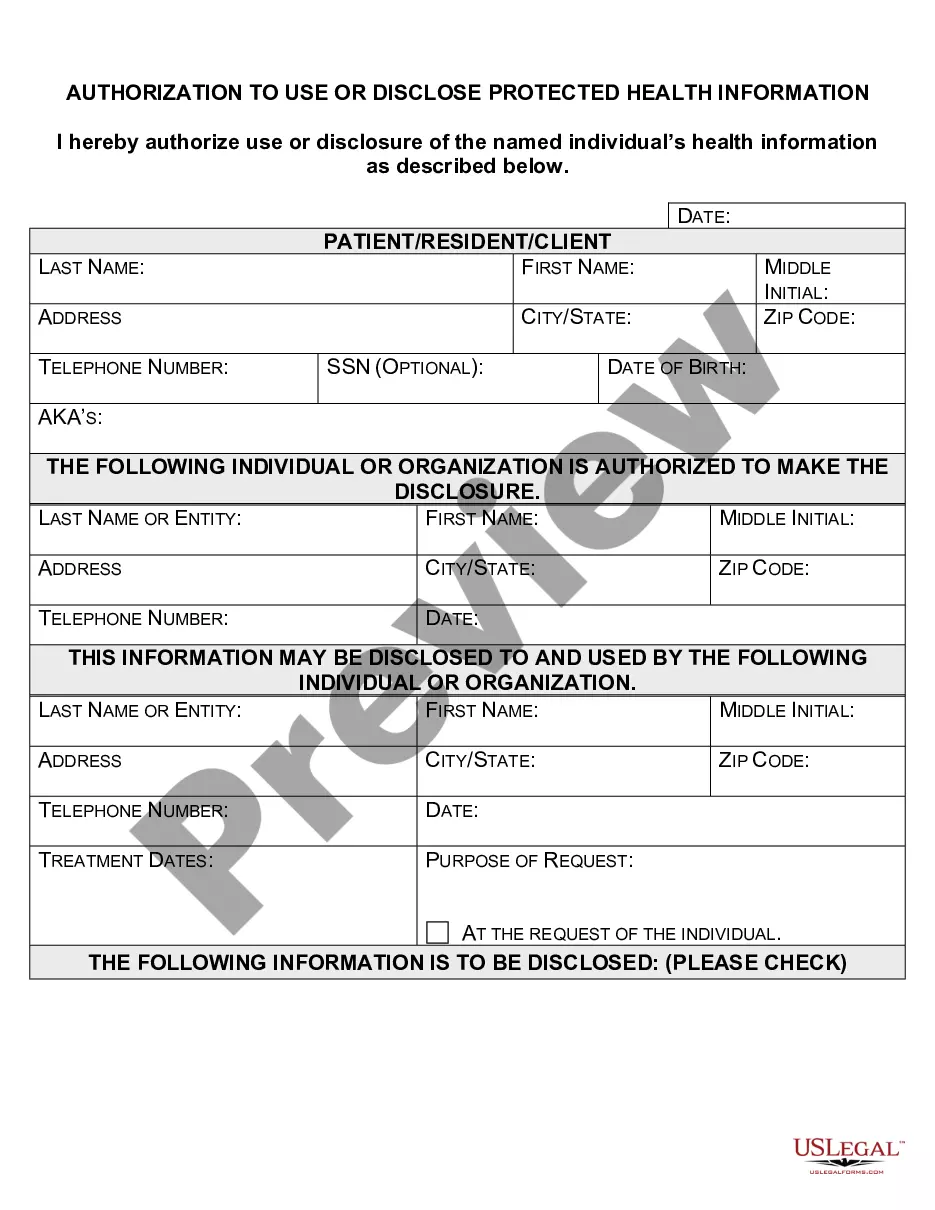
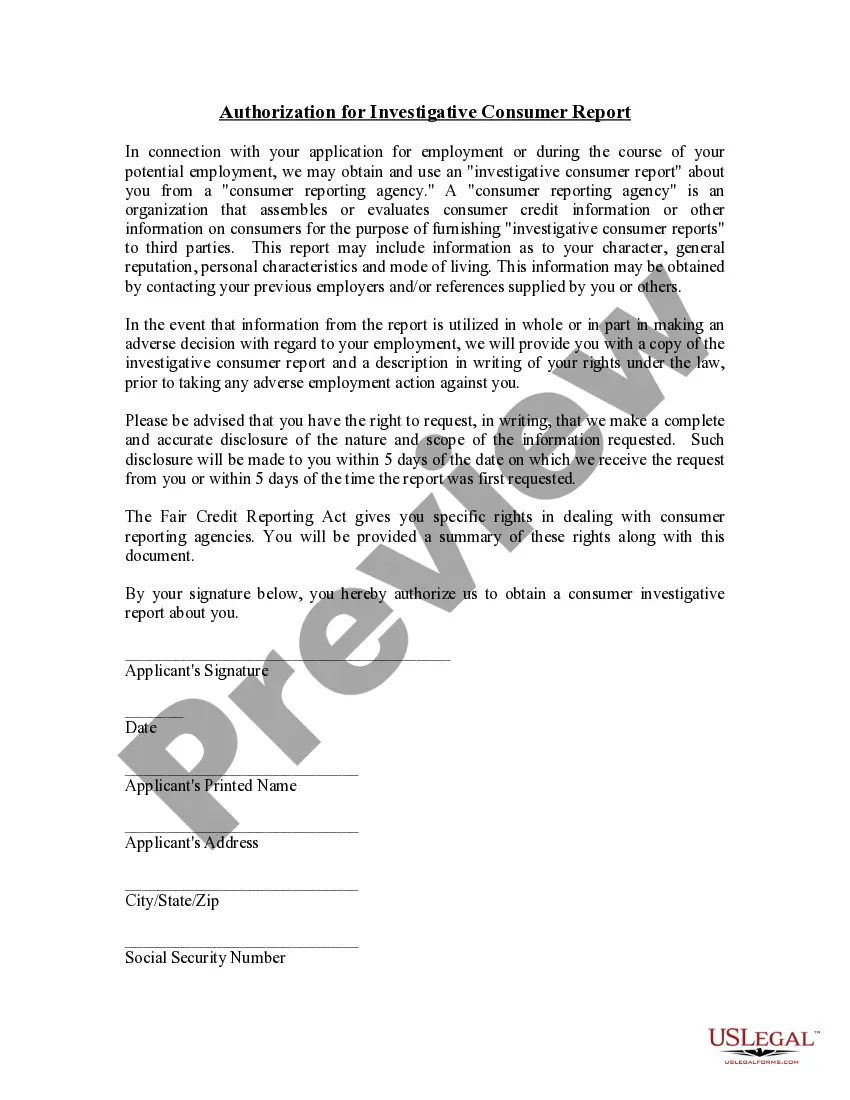
An authorization form for the release of protected health information is a legal document that allows your healthcare provider to share your PHI with other entities. Completing this authorization ensures that you maintain control over who accesses your health information. In North Dakota, submitting a North Dakota Request for Restrictions on Uses and Disclosures of Protected Health Information can also be part of this process, giving you additional leverage in protecting your data. You can find templates for these forms through platforms like US Legal Forms.
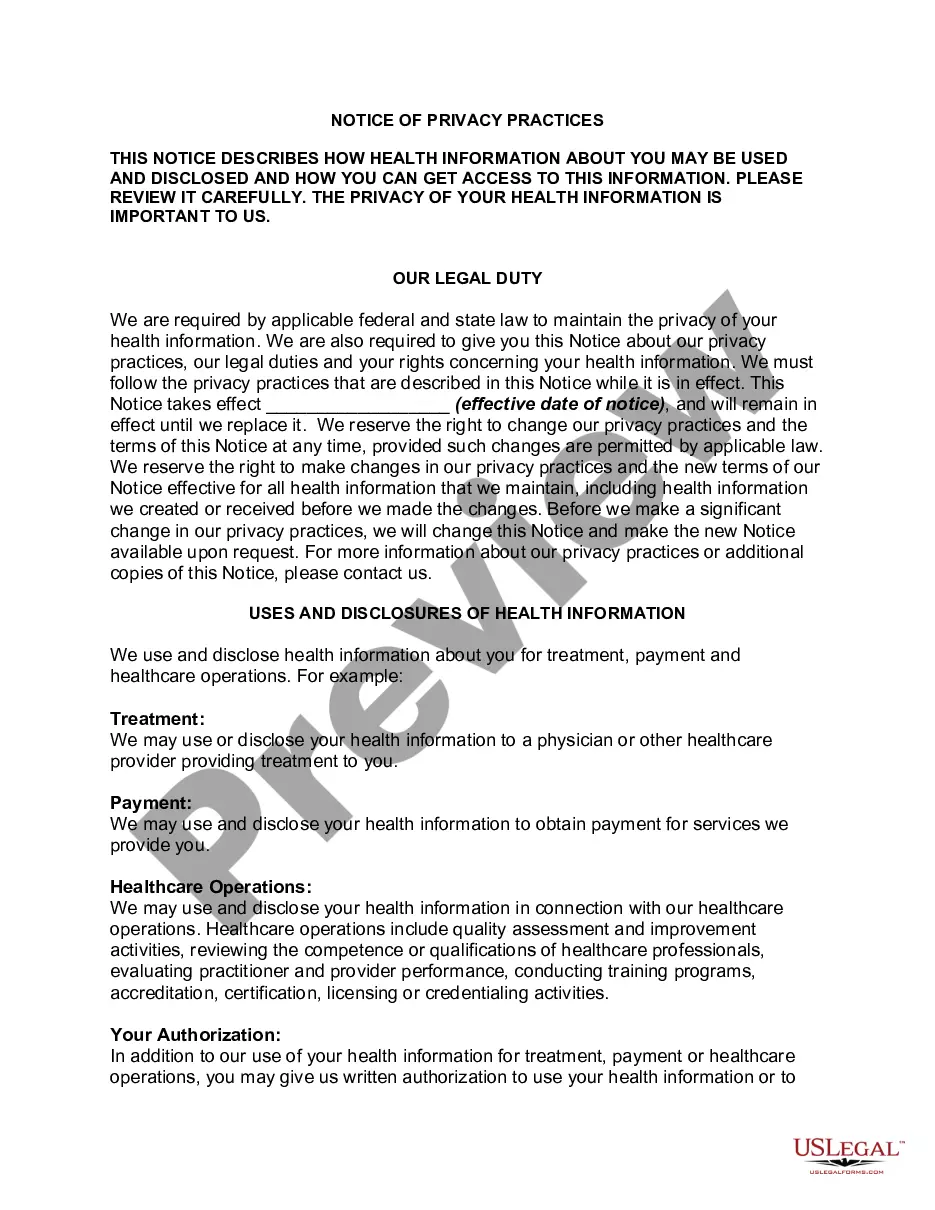
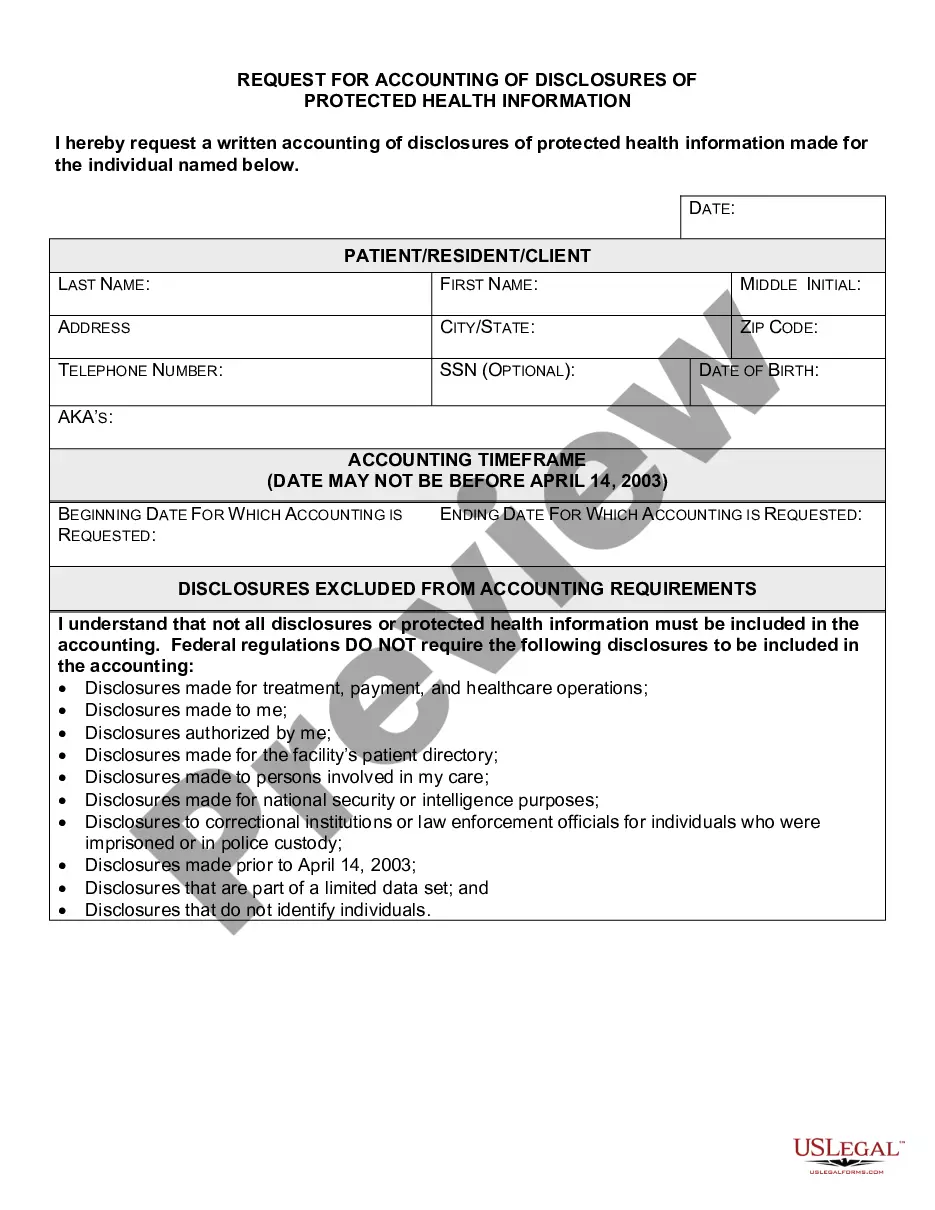
Covered entities may disclose protected health information to: Public health authorities authorized by law to collect or receive such information for preventing or controlling disease, injury, or disability. Public health or other government authorities authorized to receive reports of child abuse and neglect.
A covered entity is required to agree to an individual's request to restrict the disclosure of their PHI to a health plan when both of the following conditions are met: (1) the disclosure is for payment or health care operations and is not otherwise required by law; and (2) the PHI pertains solely to a health care item
Regardless of the method by which de-identification is achieved, the Privacy Rule does not restrict the use or disclosure of de-identified health information, as it is no longer considered protected health information, according to HHS.
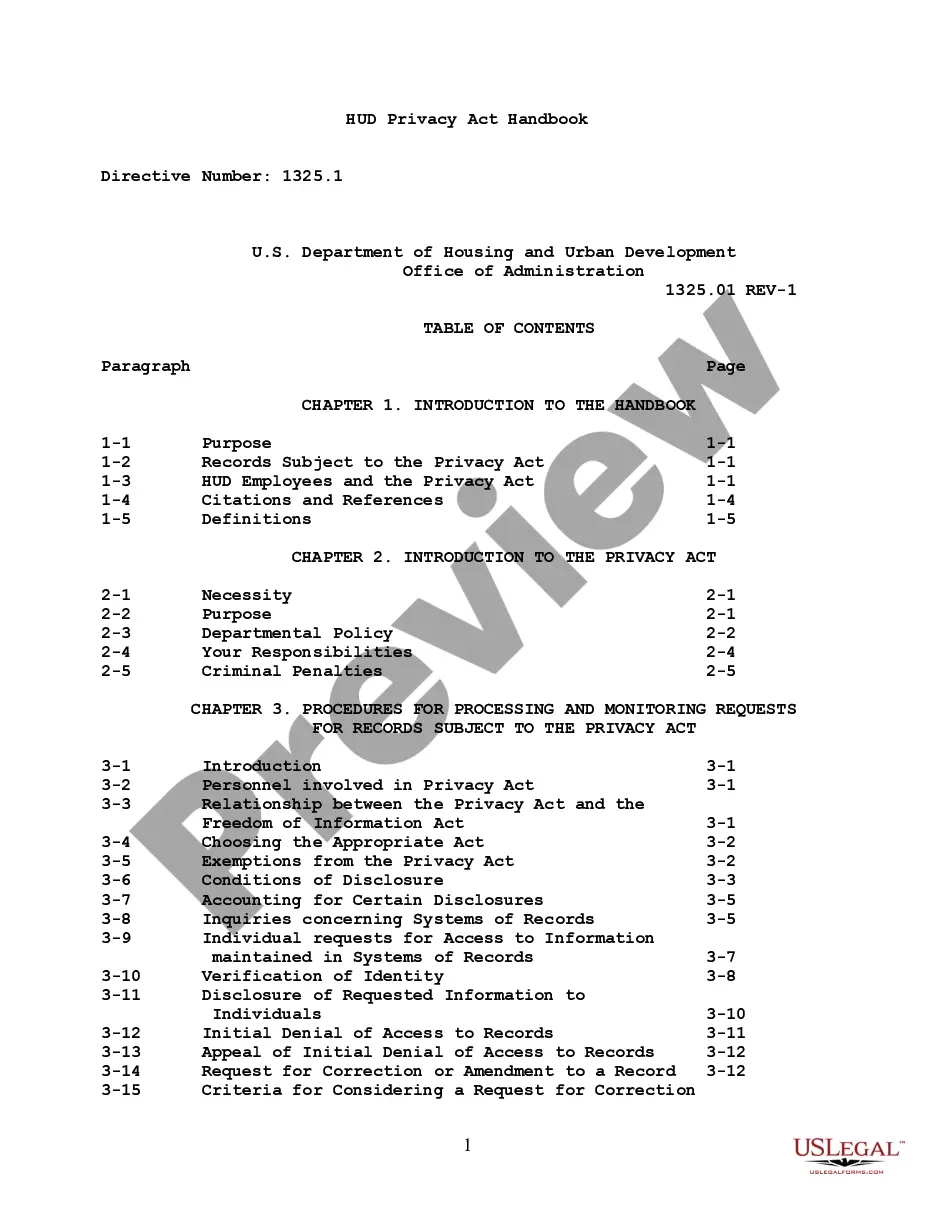
The Health Insurance Portability and Accountability Act of 1996 (HIPAA) is a federal law that required the creation of national standards to protect sensitive patient health information from being disclosed without the patient's consent or knowledge.
Covered entities may disclose protected health information that they believe is necessary to prevent or lessen a serious and imminent threat to a person or the public, when such disclosure is made to someone they believe can prevent or lessen the threat (including the target of the threat).
One fact sheet addresses Permitted Uses and Disclosures for Health Care Operations, and clarifies that an entity covered by HIPAA (covered entity), such as a physician or hospital, can disclose identifiable health information (referred to in HIPAA as protected health information or PHI) to another covered entity (or
A covered entity may disclose protected health information to the individual who is the subject of the information. (2) Treatment, Payment, Health Care Operations. A covered entity may use and disclose protected health information for its own treatment, payment, and health care operations activities.
Since its initial adoption, the Health Insurance Portability and Accountability Act of 1996 (HIPAA) Privacy Rule has granted individuals the right to request restrictions regarding the use and disclosure of their protected health information (PHI) for treatment, payment, and healthcare operations (TPO).
HIPAA Exceptions DefinedTo public health authorities to prevent or control disease, disability or injury. To foreign government agencies upon direction of a public health authority. To individuals who may be at risk of disease. To family or others caring for an individual, including notifying the public.