North Carolina Affidavit of No Coverage by Another Group Health Plan
Description
How to fill out Affidavit Of No Coverage By Another Group Health Plan?
Are you presently involved in a scenario where you require documents for possibly business or specific objectives almost every day.
There are numerous legitimate document templates accessible online, but finding versions you can trust is challenging.
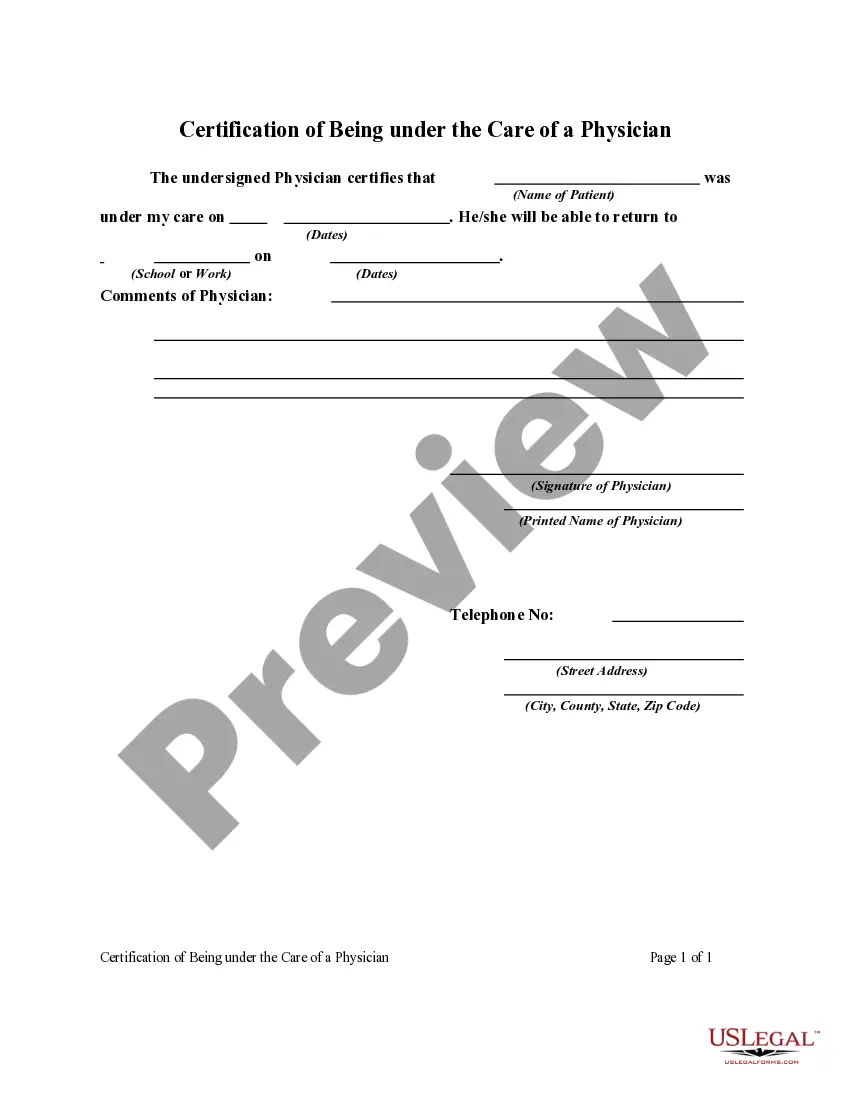
US Legal Forms offers thousands of template forms, such as the North Carolina Affidavit of No Coverage by Another Group Health Plan, designed to meet federal and state requirements.
When you find the appropriate form, click Acquire now.
Choose the payment method you prefer, fill in the required details to create your account, and complete your purchase using your PayPal or credit card.
- If you are already familiar with the US Legal Forms website and possess an account, simply Log In.
- Then, you can download the North Carolina Affidavit of No Coverage by Another Group Health Plan template.
- If you don’t have an account and wish to start using US Legal Forms, follow these steps.
- Select the form you need and ensure it is for the correct town/area.
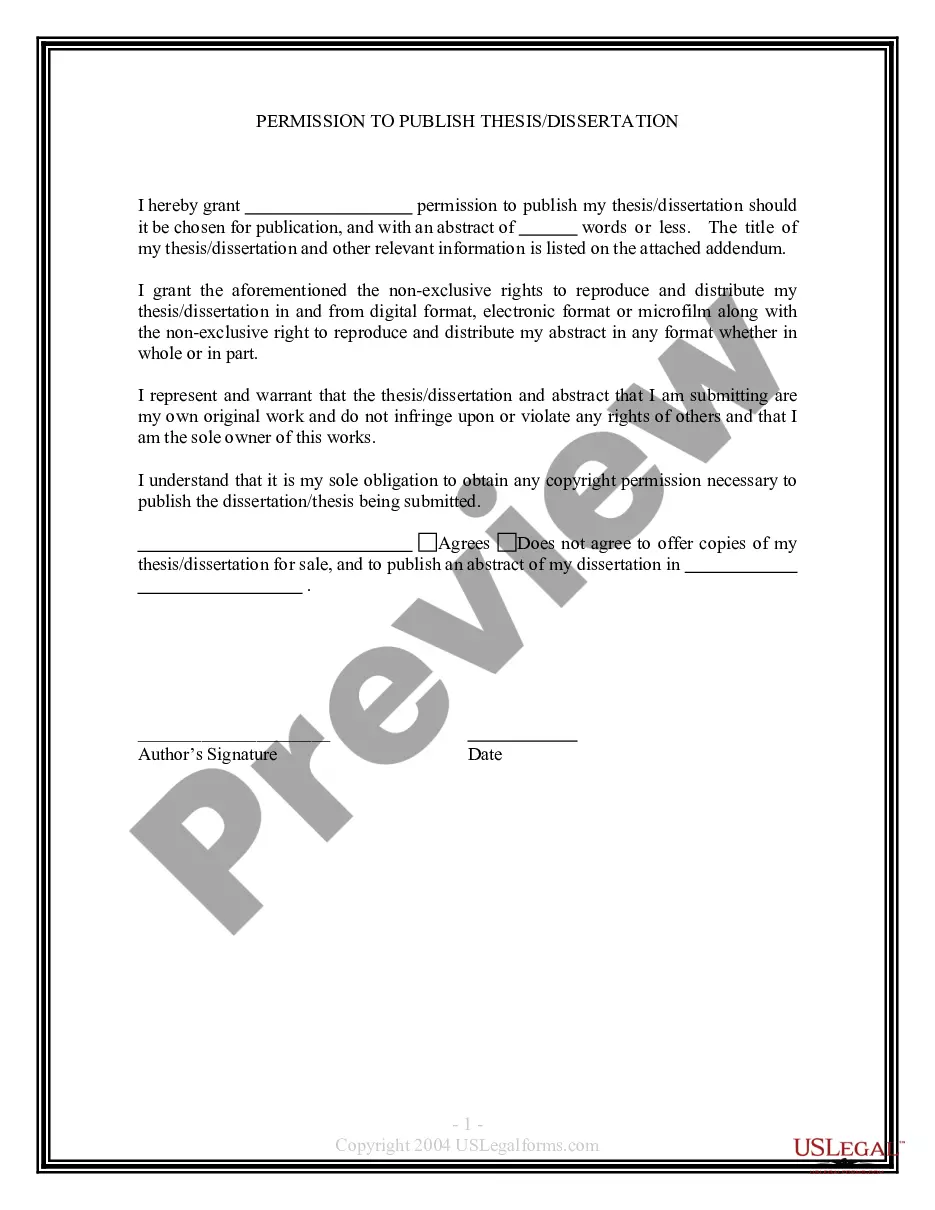
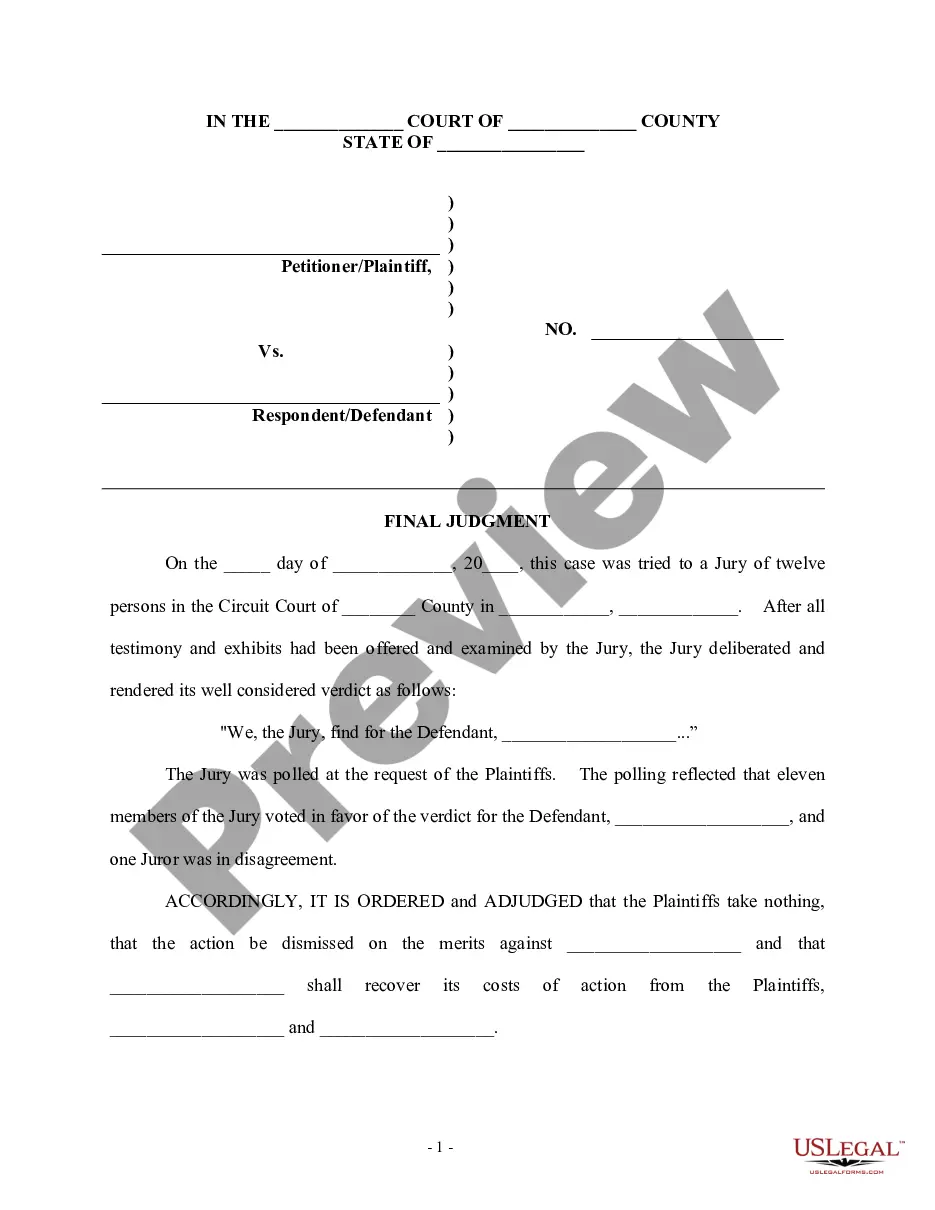
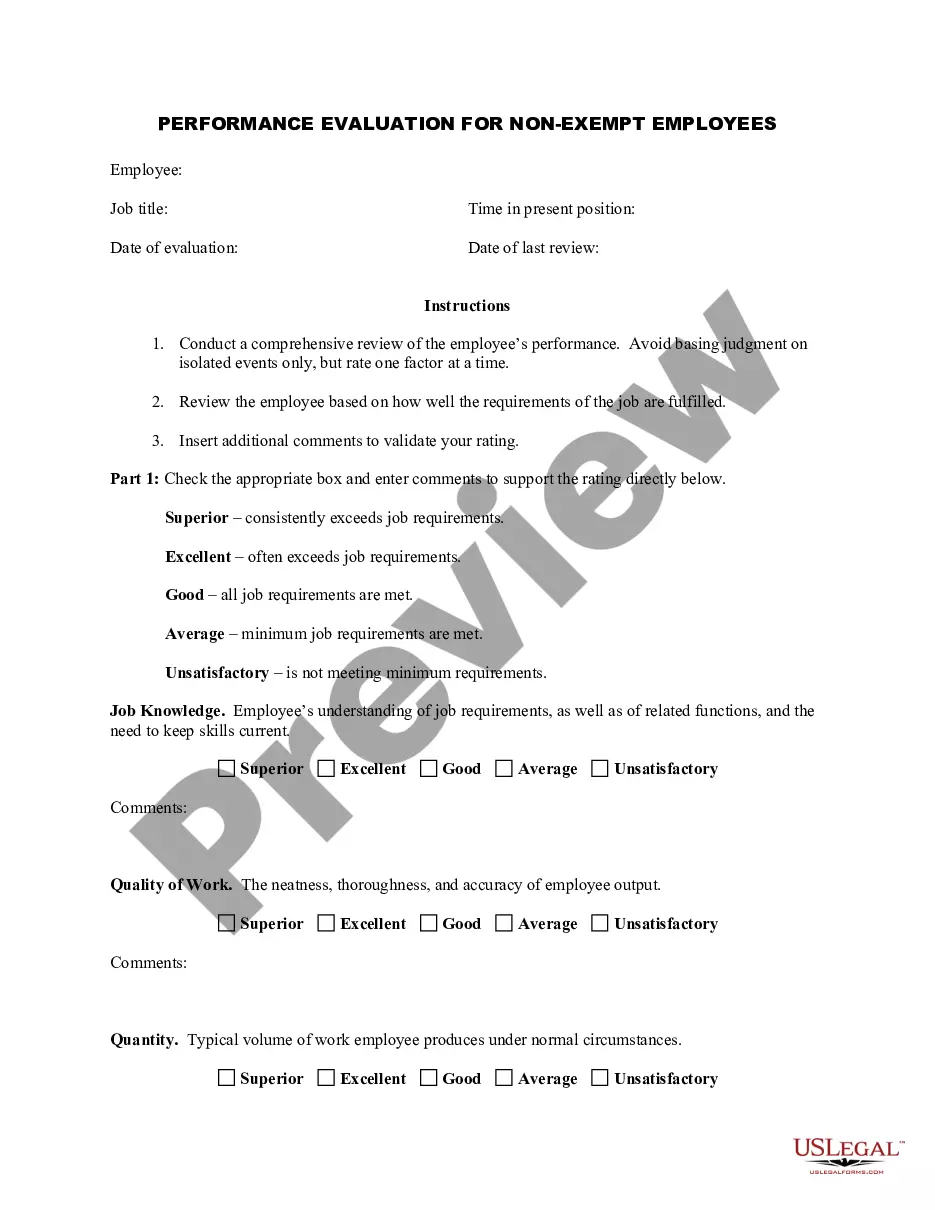
- Utilize the Preview button to review the form.
- Read the description to confirm that you have selected the right form.
- If the form isn’t what you seek, use the Search field to locate the form that suits your needs.
Form popularity
FAQ
How long will COBRA continuation coverage last? When loss of coverage due to end of employment or a reduction in hours of employment, coverage generally may be continued for up to a total of 18 months.
The short answer is no under the new healthcare reform, no North Carolina employer is required by law to offer health insurance coverage to their employees.
North Carolina residents are required to have health insurance per the Affordable Care Act (ACA). However, there is no North Carolina state law mandating employers to provide employees with group health plans.
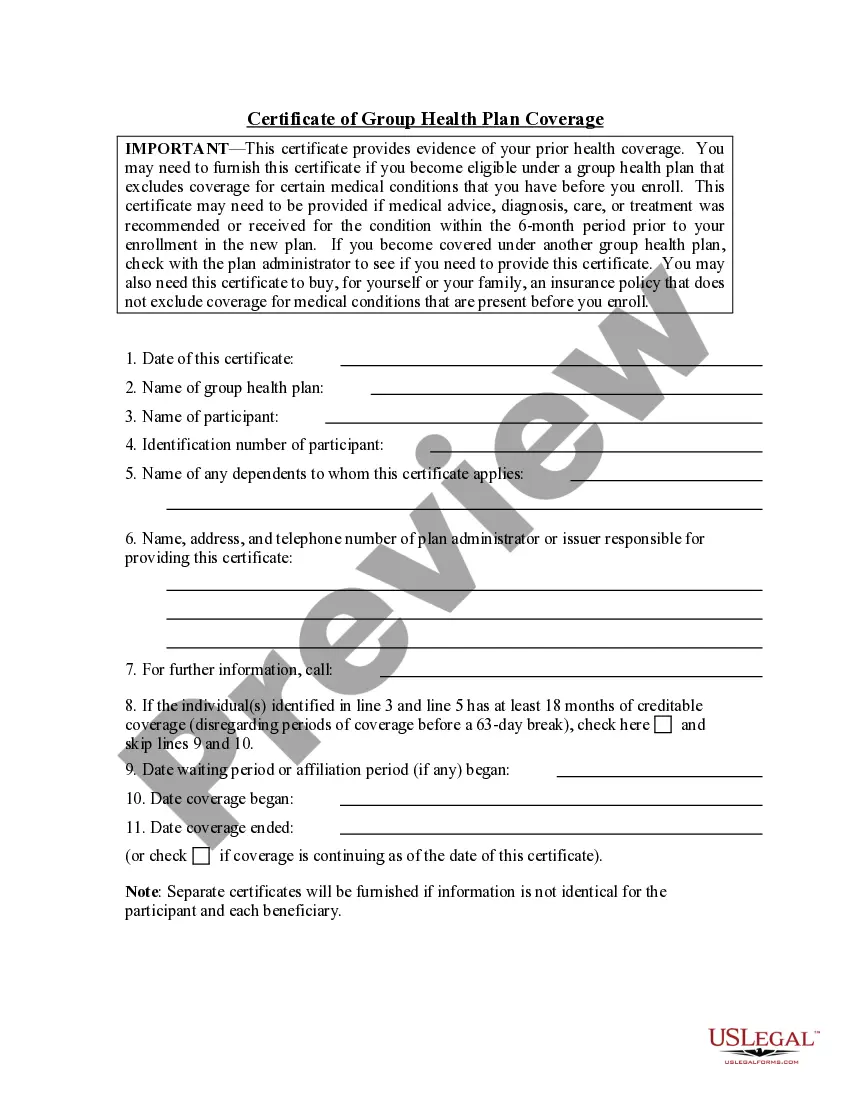
A certificate of Creditable Coverage (COCC) is a document provided by your previous insurance carrier that proves that your insurance has ended. This includes the name of the member to whom it applies as well as the coverage effective date and cancelation date.
This document explains the health benefits you and your dependents have under the plan. It details the services that will and will not be covered. Services that are not covered are called exclusions.
The primary purpose of the certificate is to show the amount of creditable coverage that you had under a group health plan or other health insurance coverage, because this can reduce or eliminate the length of time that any pre-existing condition clause in a new plan otherwise might apply to you.
Who is issued a certificate of insurance with a group insurance policy? The participant is issued a certificate of insurance with a group insurance policy.
If a Social Security agreement assigns coverage of the employee's work to the United States, the Social Security Administration issues a U.S. Certificate of Coverage. The certificate serves as proof that the employee and employer are exempt from the payment of Social Security taxes to the foreign country.
Continuation coverage allows someone who recently lost their employer-based health coverage to continue their current insurance policy as long as they pay the full monthly premiums.
Under COBRA, you and your family have the right to remain on whatever health plan your former employer has for up to 18 months. You must continue paying the full premium, which includes both your former employer's share and your share plus a 2 percent administrative fee.