Montana General Notice of Preexisting Condition Exclusion
Description
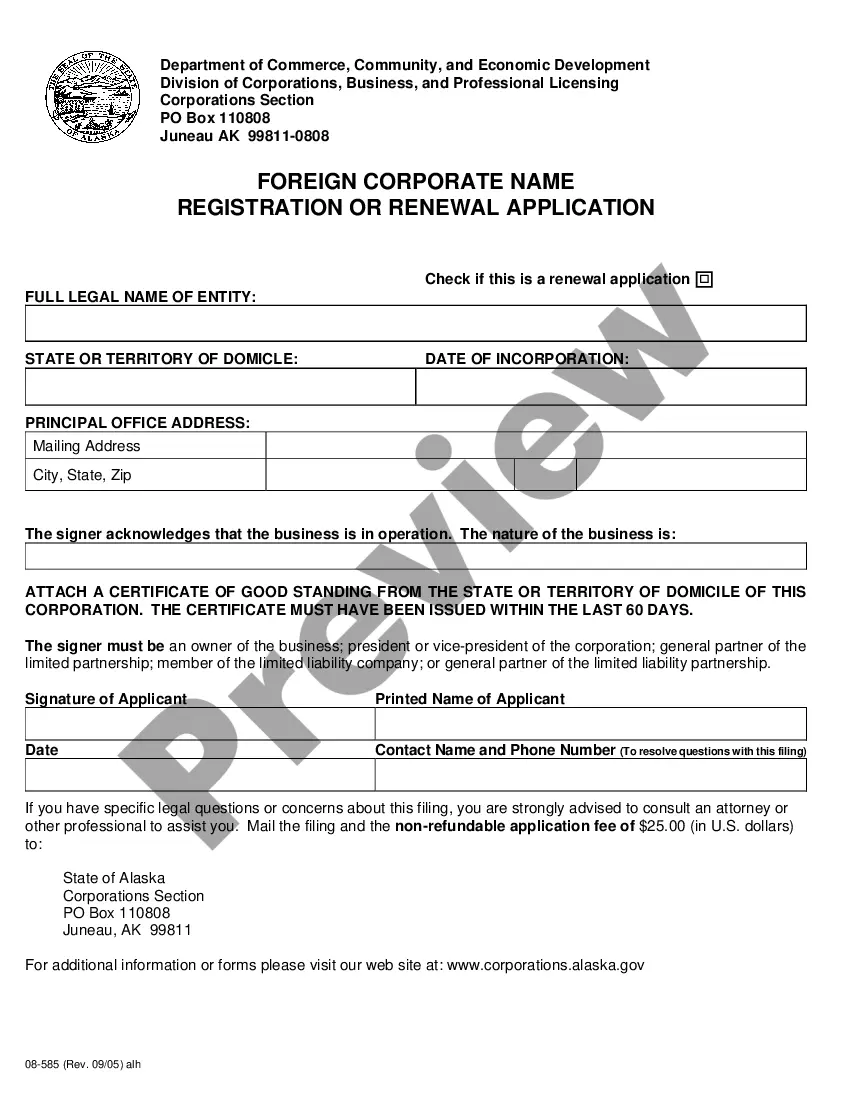
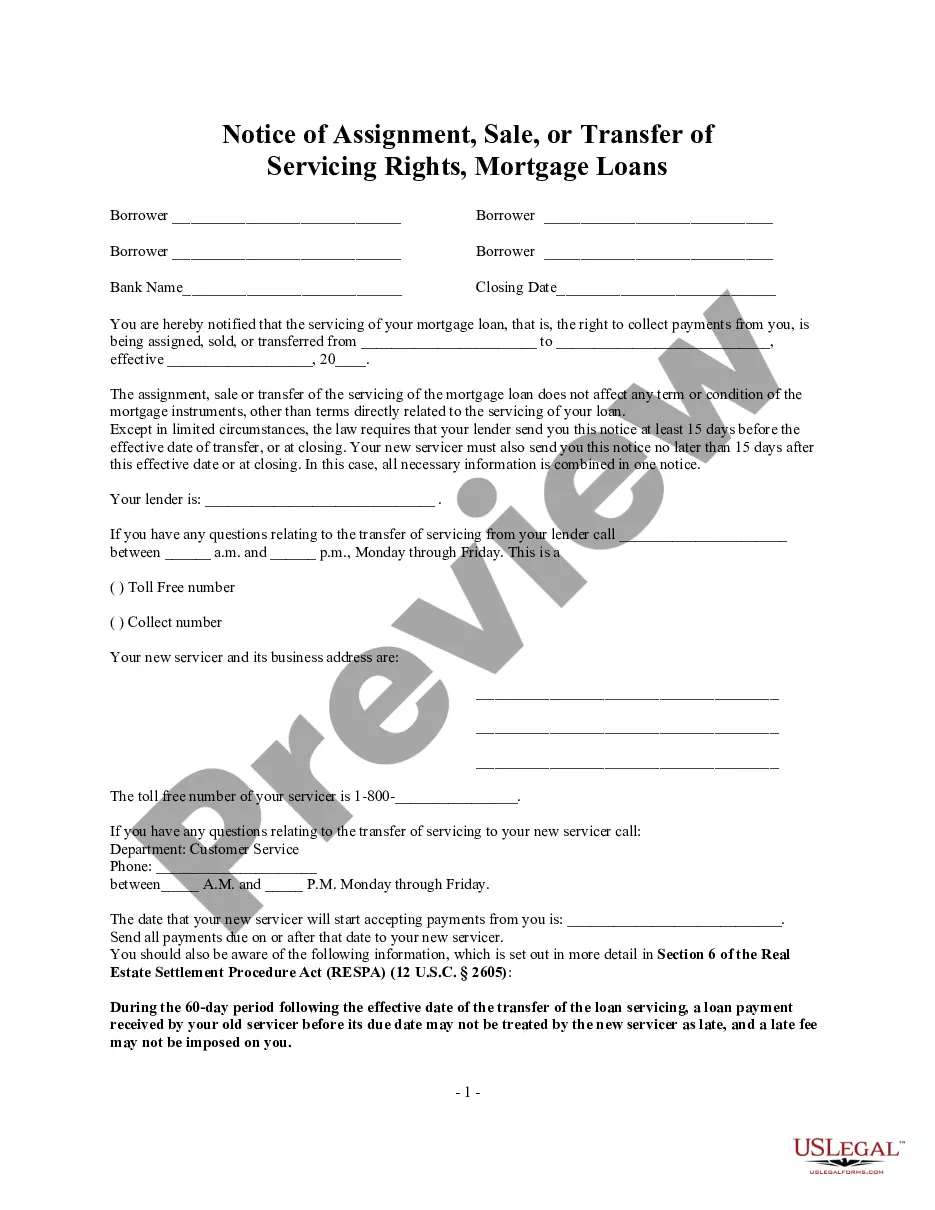
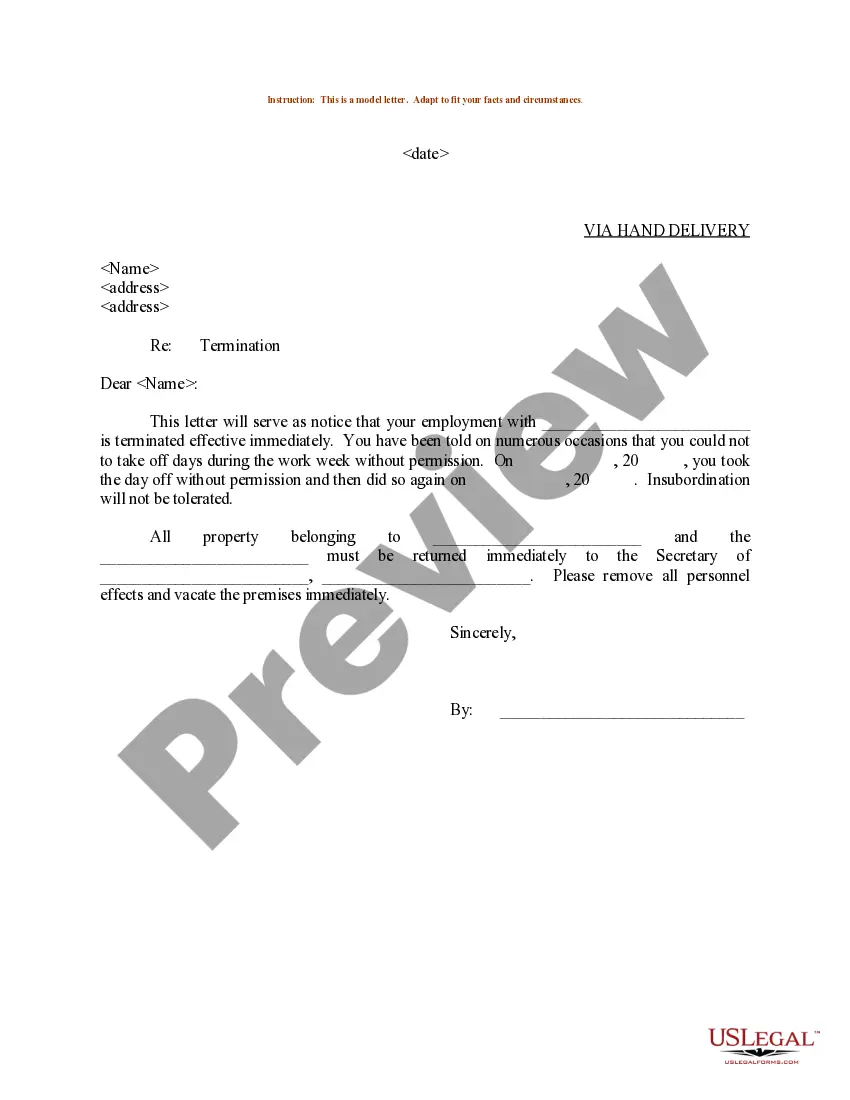
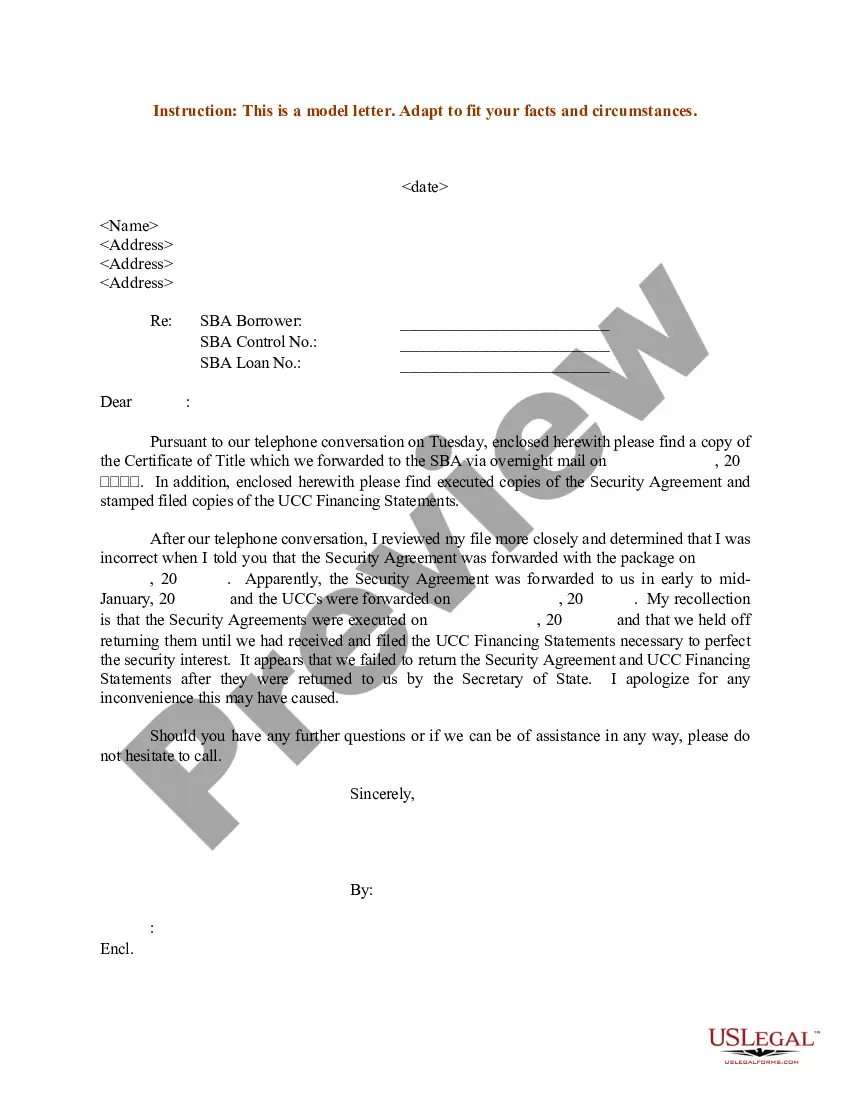
How to fill out General Notice Of Preexisting Condition Exclusion?
You might spend hours online searching for the legal document format that meets the state and federal requirements you desire.
US Legal Forms offers thousands of legal templates that are reviewed by professionals.
You can conveniently download or print the Montana General Notice of Preexisting Condition Exclusion from my service.
Review the form description to confirm that you have chosen the appropriate document. If available, use the Preview button to browse through the document format as well.
- If you already possess a US Legal Forms account, you can sign in and click the Acquire button.
- Following that, you can complete, modify, print, or sign the Montana General Notice of Preexisting Condition Exclusion.
- Every legal document template you obtain is yours permanently.
- To obtain another copy of the acquired form, navigate to the My documents tab and click the corresponding button.
- If you are using the US Legal Forms website for the first time, follow the simple instructions below.
- First, ensure that you have selected the correct document format for the state/city of your choice.
Form popularity
FAQ
Yes, insurance companies have the ability to deny coverage based on pre-existing conditions, depending on the policy. However, the Montana General Notice of Preexisting Condition Exclusion regulates how these cases are handled. Familiarizing yourself with these regulations can help in planning your insurance application. Uslegalforms assists you in navigating these complex issues.
What Is the Pre-existing Condition Exclusion Period? The pre-existing condition exclusion period is a health insurance provision that limits or excludes benefits for a period of time. The determination is based on the policyholder having a medical condition prior to enrolling in a health plan.
A medical illness or injury that you have before you start a new health care plan may be considered a pre-existing condition. Conditions like diabetes, COPD, cancer, and sleep apnea, may be examples of pre-existing health conditions.
The time period during which an individual policy won't pay for care relating to a pre-existing condition. Under an individual policy, conditions may be excluded permanently (known as an "exclusionary rider").
The time period during which a health plan won't pay for care relating to a pre-existing condition. Under a job-based plan, this cannot exceed 12 months for a regular enrollee or 18 months for a late-enrollee.
A health insurance risk pool is a group of individuals whose medical costs are combined to calculate premiums. Pooling risks. together allows the higher costs of the less healthy to be offset by the relatively lower costs of the healthy, either in a plan overall or within a premium rating category.
When an insurance company sends a policy to the insured with an attached application, the element that makes the application part of the contract between the insured and the insurer is called the? Entire Contract provision. An insured must notify an insurer of a medical claim within how many days after an accident? 20.
Health insurers can no longer charge more or deny coverage to you or your child because of a pre-existing health condition like asthma, diabetes, or cancer, as well as pregnancy. They cannot limit benefits for that condition either.
Yes. Under the Affordable Care Act, health insurance companies can't refuse to cover you or charge you more just because you have a pre-existing condition that is, a health problem you had before the date that new health coverage starts.
Exclusion a provision of an insurance policy or bond referring to hazards, perils, circumstances, or property not covered by the policy. Exclusions are usually contained in the coverage form or causes of loss form used to construct the insurance policy.