Mississippi Sample COBRA Enrollment and / or Waiver Letter
Description
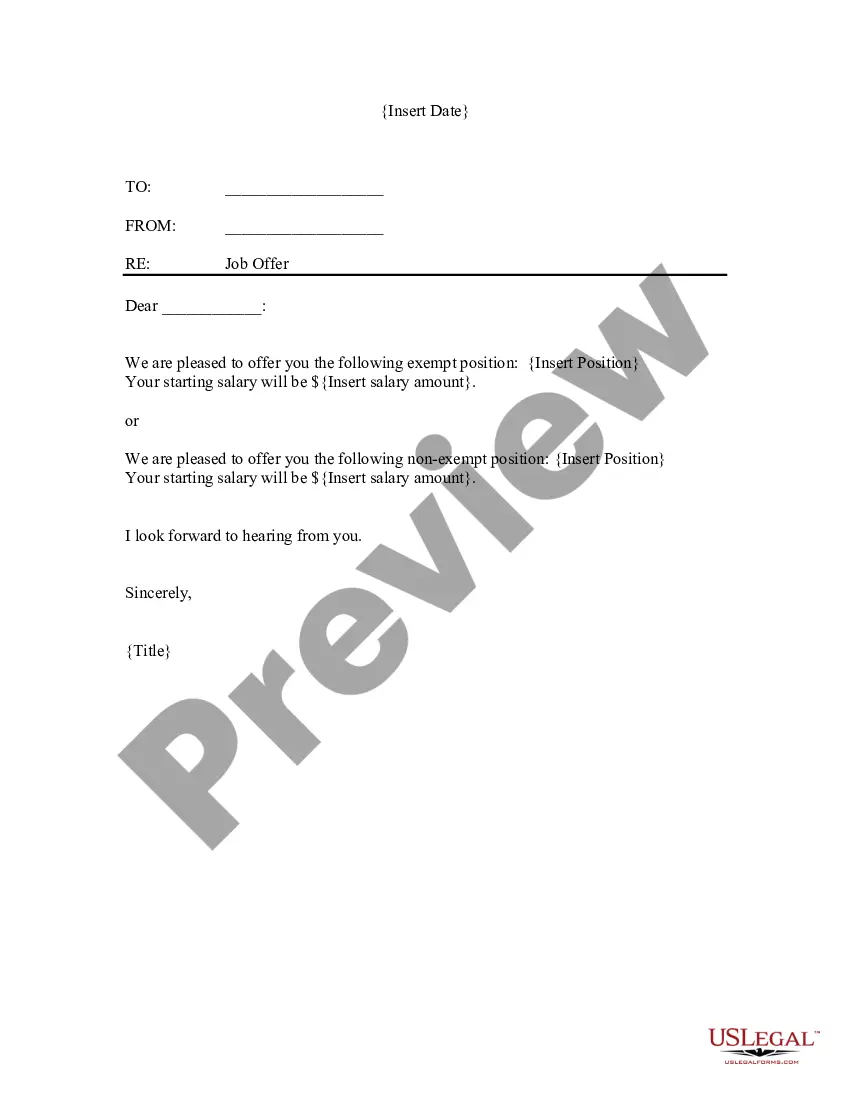
How to fill out Sample COBRA Enrollment And / Or Waiver Letter?
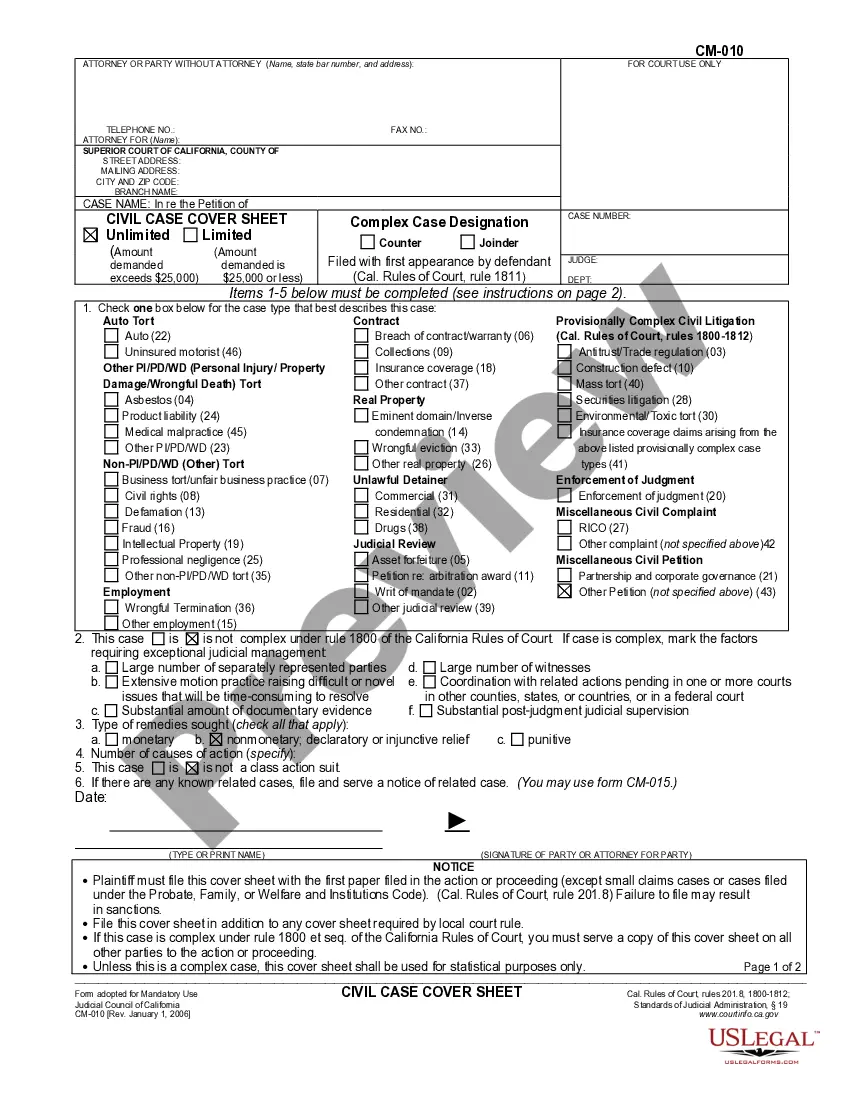
It is feasible to dedicate hours online looking for the legal document template that satisfies the state and federal requirements you require.
US Legal Forms provides a vast collection of legal forms that are reviewed by experts.
You can easily download or print the Mississippi Sample COBRA Enrollment and/or Waiver Letter from their service.
To find another version of the form, use the Search field to locate the template that suits your needs and requirements.
- If you have a US Legal Forms account, you can sign in and click on the Download button.
- Then, you can complete, modify, print, or sign the Mississippi Sample COBRA Enrollment and/or Waiver Letter.
- Each legal document template you download is yours indefinitely.
- To obtain another copy of a purchased form, visit the My documents section and click on the relevant button.
- If you are using the US Legal Forms website for the first time, follow the simple instructions listed below.
- First, ensure you have selected the correct document template for your state/city of choice.
- Review the form description to confirm you have chosen the right version.
- If available, utilize the Preview button to view the document template as well.
Form popularity
FAQ
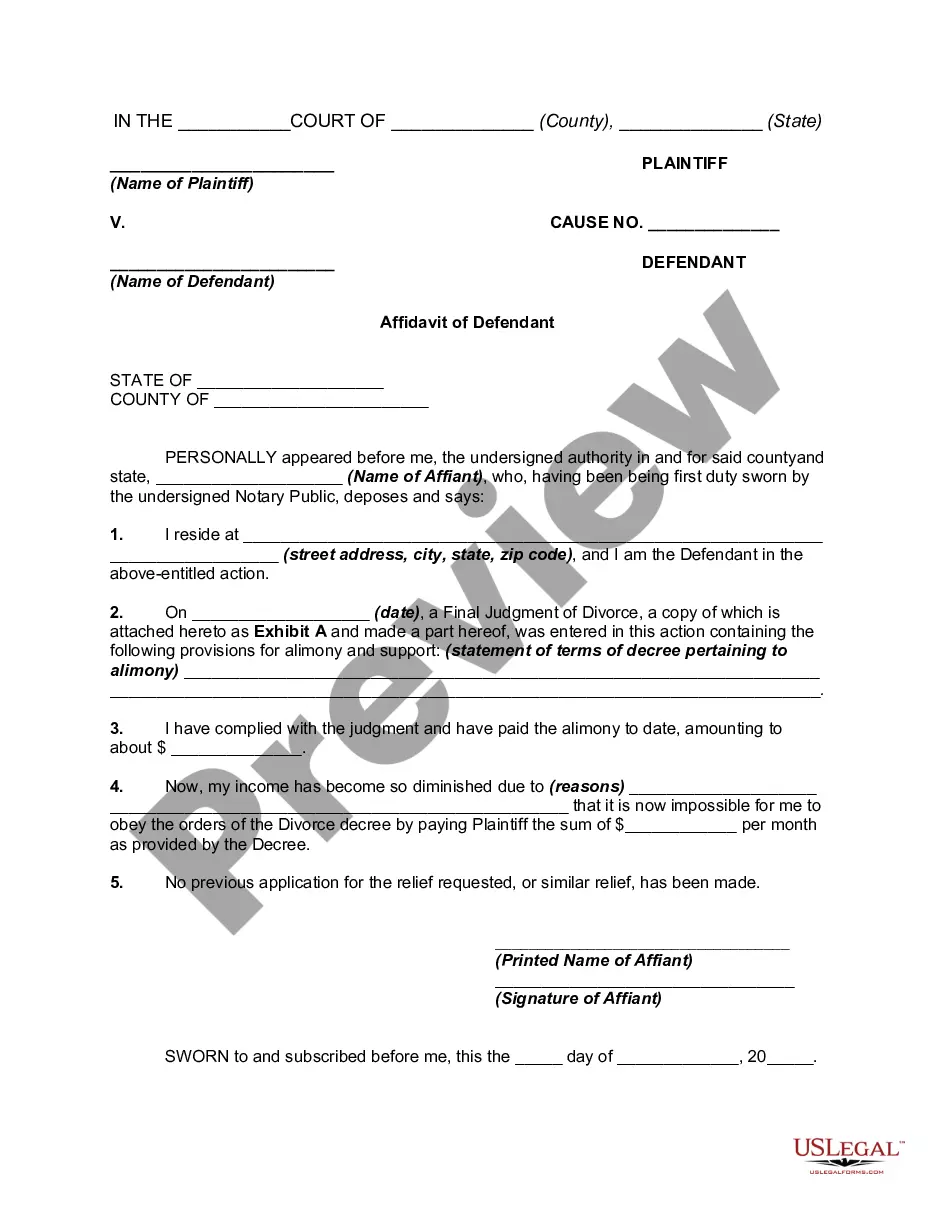
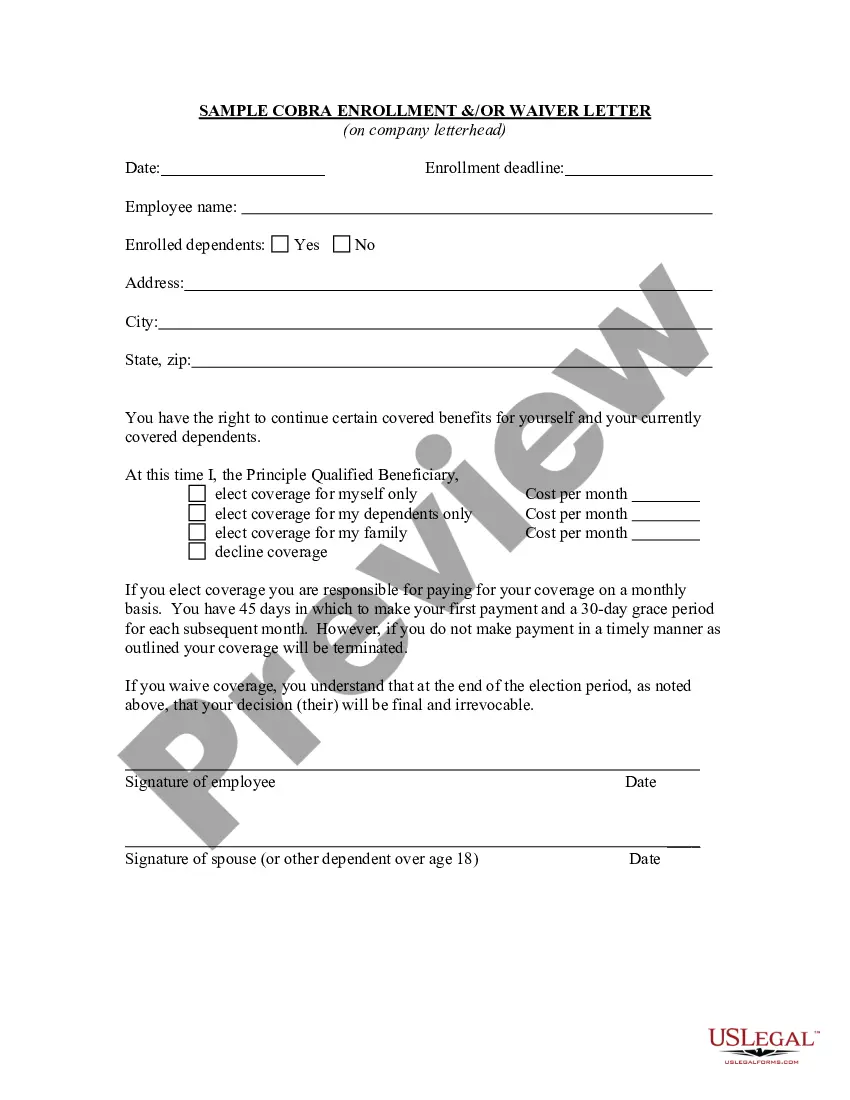
The initial notice, also referred to as the general notice, communicates general COBRA rights and obligations to each covered employee (and his or her spouse) who becomes covered under the group health plan.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) is a landmark federal law, passed in 1985, that provides for continuing group health insurance coverage for some employees and their families after a job loss or other qualifying event.
COBRA is a federal law about health insurance. If you lose or leave your job, COBRA lets you keep your existing employer-based coverage for at least the next 18 months. Your existing healthcare plan will now cost you more. Under COBRA, you pay the whole premium including the share your former employer used to pay.
In addition, employers can provide COBRA notices electronically (via email, text message, or through a website) during the Outbreak Period, if they reasonably believe that plan participants and beneficiaries have access to these electronic mediums.
The purpose of this letter is to inform you of your rights and responsibilities as a plan participant. Qualifying Event: At the end of your employment or because of reduction of hours (not maintain full-time status) you will receive this letter.
The initial notice, also referred to as the general notice, communicates general COBRA rights and obligations to each covered employee (and his or her spouse) who becomes covered under the group health plan.
The COBRA Notice informs the qualified beneficiary of their rights under COBRA law, and the form allows the qualified beneficiary to elect COBRA coverage to continue enrollment in benefits.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
Failure to pay premiums. When a participant fails to make a timely payment of any required COBRA premium, the employer may terminate COBRA coverage. Employers must provide participants with at least a 30-day grace period for payment of any late premiums.
COBRA continuation coverage notices are documents that explain employees' rights under the Consolidated Omnibus Budget Reconciliation Act of 1985. These documents generally contain a variety of information, including the following: The name of the health insurance plan.