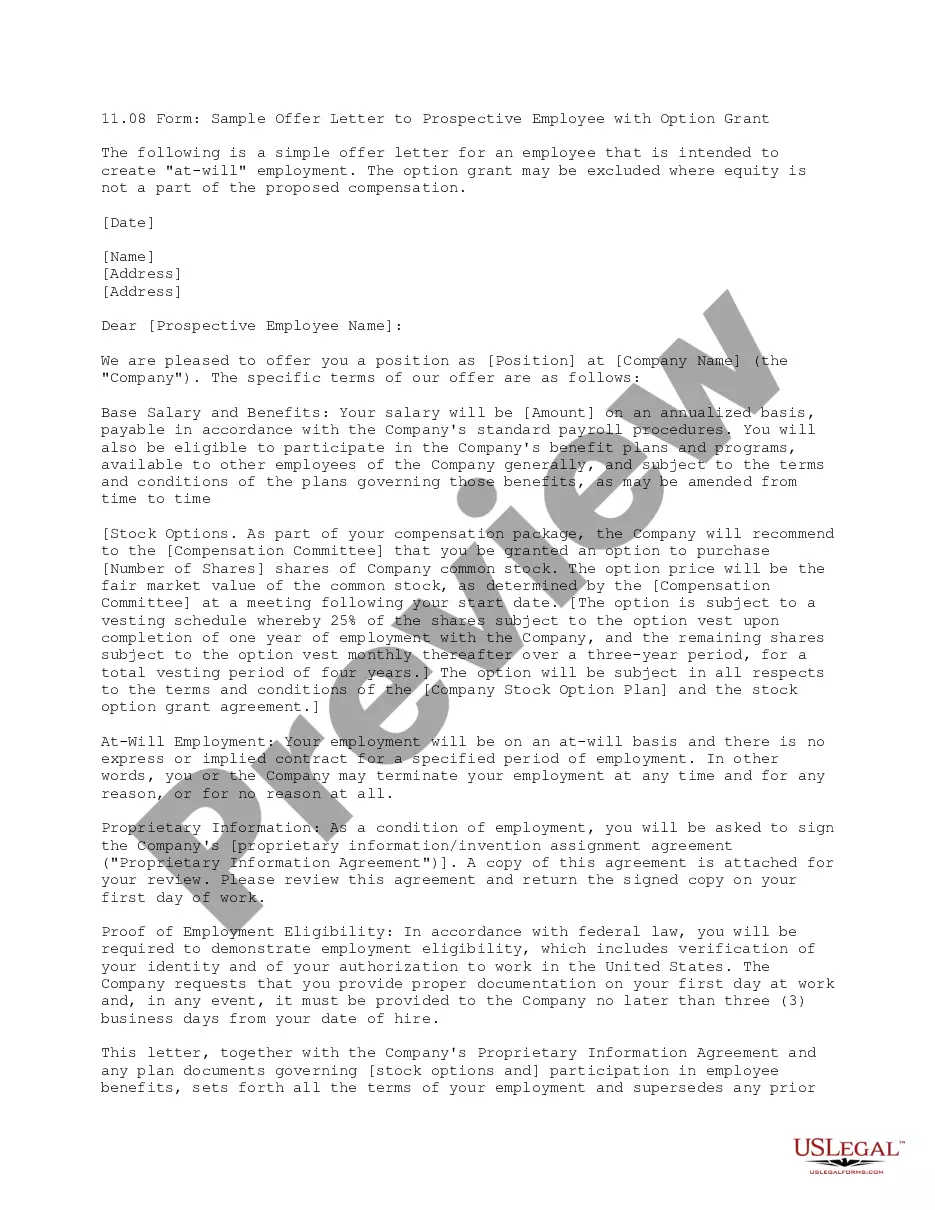
Mississippi Introductory COBRA Letter
Description
How to fill out Introductory COBRA Letter?
Finding the appropriate legal document template can be a challenge.
Without a doubt, there are countless templates available online, but how will you find the legal form you need.
Utilize the US Legal Forms website. The platform provides thousands of templates, including the Mississippi Introductory COBRA Letter, which you can use for both business and personal purposes.
If the form does not meet your needs, utilize the Search field to locate the correct form. Once you are certain that the form is accurate, click the Buy now button to obtain the form. Choose the payment plan you prefer and input the required information. Create your account and complete the purchase using your PayPal account or credit card. Select the file format and download the legal document template to your device. Fill out, modify, and print the received Mississippi Introductory COBRA Letter. US Legal Forms is the largest repository of legal forms where you can find numerous document templates. Use the service to acquire properly-created documentation that adheres to state regulations.
- All of the forms are reviewed by experts and comply with state and federal regulations.
- If you are already registered, Log In to your account and click the Download button to access the Mississippi Introductory COBRA Letter.
- Use your account to browse the legal forms you have previously obtained.
- Head to the My documents section of your account and secure another copy of the document you need.
- If you are a new user of US Legal Forms, here are simple steps for you to follow.
- First, ensure you have selected the right form for your city/county. You can preview the form using the Preview option and review the form description to confirm it is suitable for you.
Form popularity
FAQ
How to Administer Cal-COBRANotifying all eligible group health care participants of their Cal-COBRA rights.Providing timely notice of Cal-COBRA eligibility, enrollment forms, and notice of the duration of coverage and terms of payment after a qualifying event has occurred.More items...
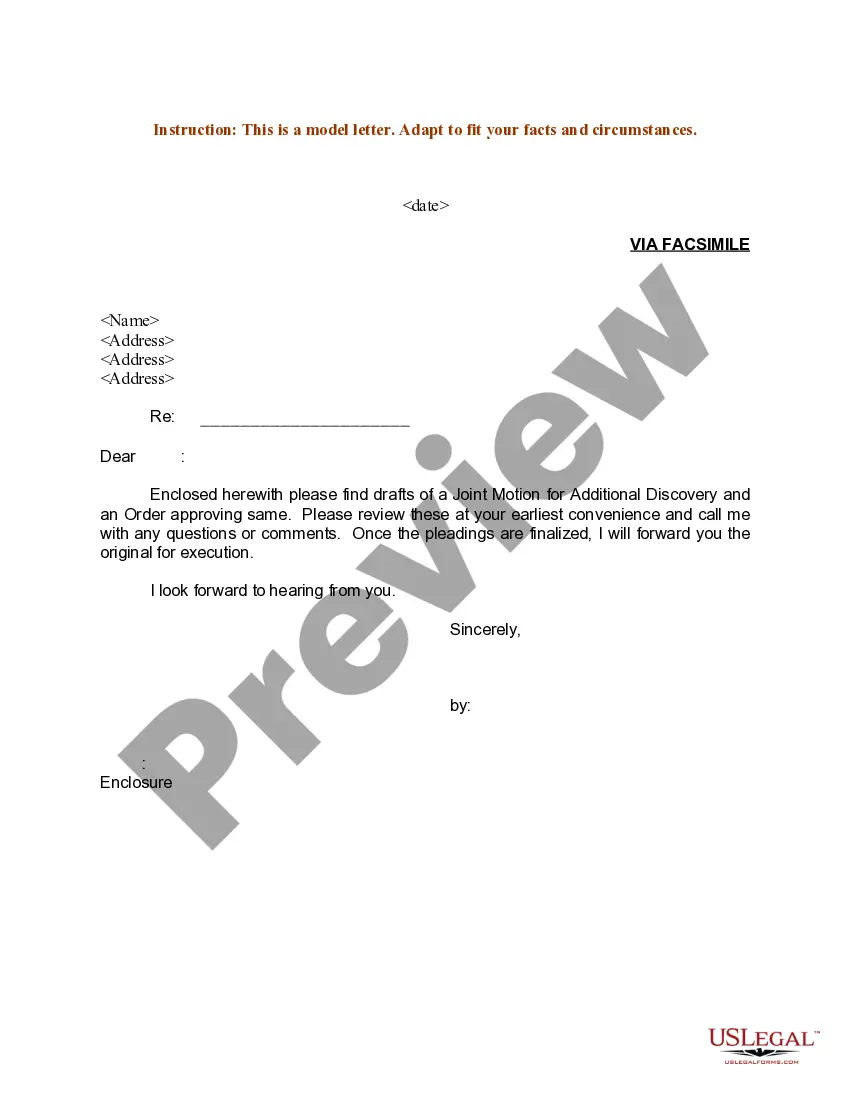
The Consolidated Omnibus Budget Reconciliation Act (COBRA) permits employees and their dependents to extend health coverage under an employer's group health plan when coverage would otherwise be lost due to termination of employment or other qualifying events. Under COBRA, employees must receive specific notices
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
The initial notice, also referred to as the general notice, communicates general COBRA rights and obligations to each covered employee (and his or her spouse) who becomes covered under the group health plan.
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
Your employer must mail you the COBRA information and forms within 14 days after receiving notification of the qualifying event. You are responsible for making sure your COBRA coverage goes into and stays in effect - if you do not ask for COBRA coverage before the deadline, you may lose your right to COBRA coverage.
If You Do Not Receive Your COBRA PaperworkReach out to the Human Resources Department and ask for the COBRA Administrator. They may use a third-party administrator to handle your enrollment. If the employer still does not comply you can call the Department of Labor at 1-866-487-2365.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
Employers should send notices by first-class mail, obtain a certificate of mailing from the post office, and keep a log of letters sent. Certified mailing should be avoided, as a returned receipt with no delivery acceptance signature proves the participant did not receive the required notice.
With all paperwork properly submitted, your COBRA coverage should begin on the first day of your qualifying event (for example, the first day you are no longer with your employer), ensuring no gaps in your coverage.