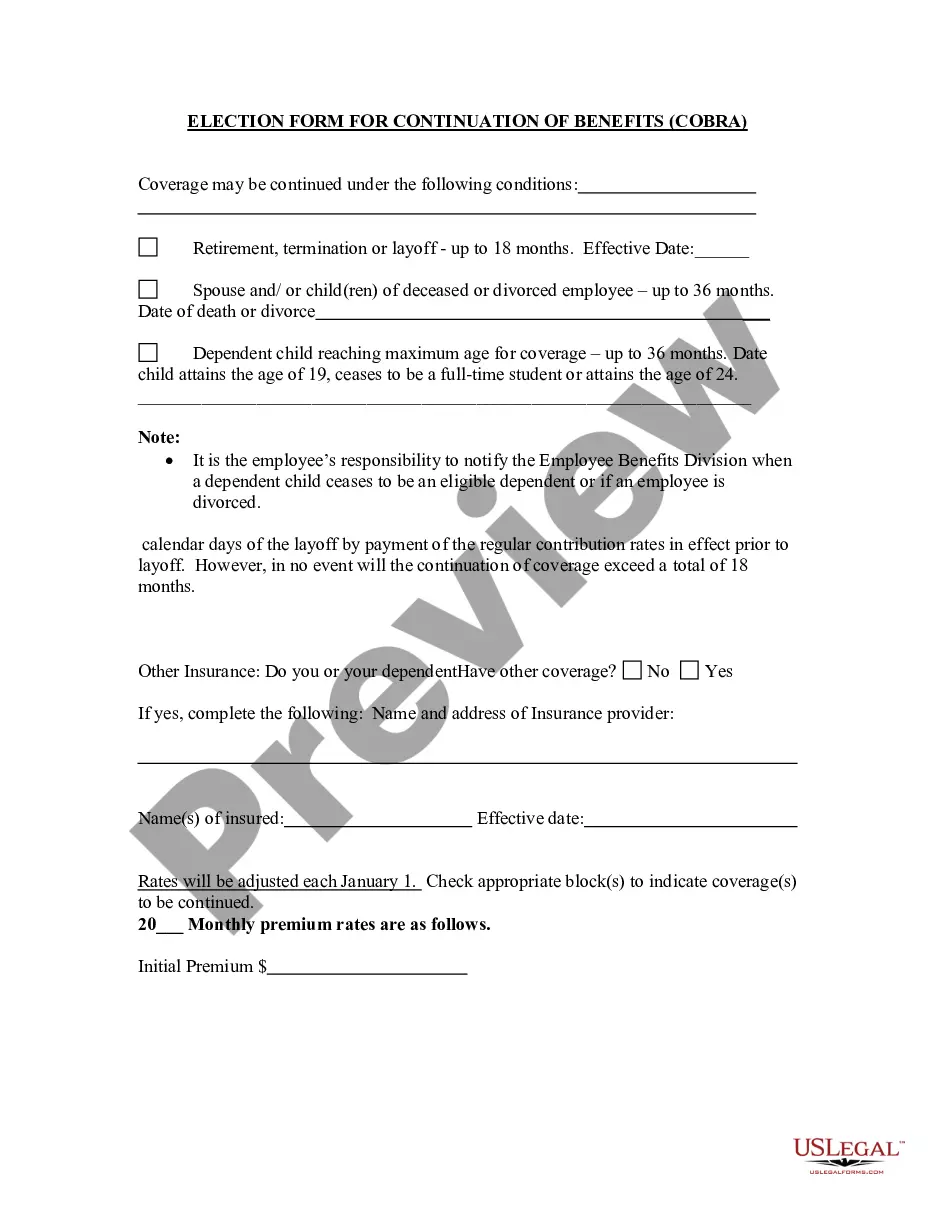
Minnesota Election Form for Continuation of Benefits - COBRA
Description
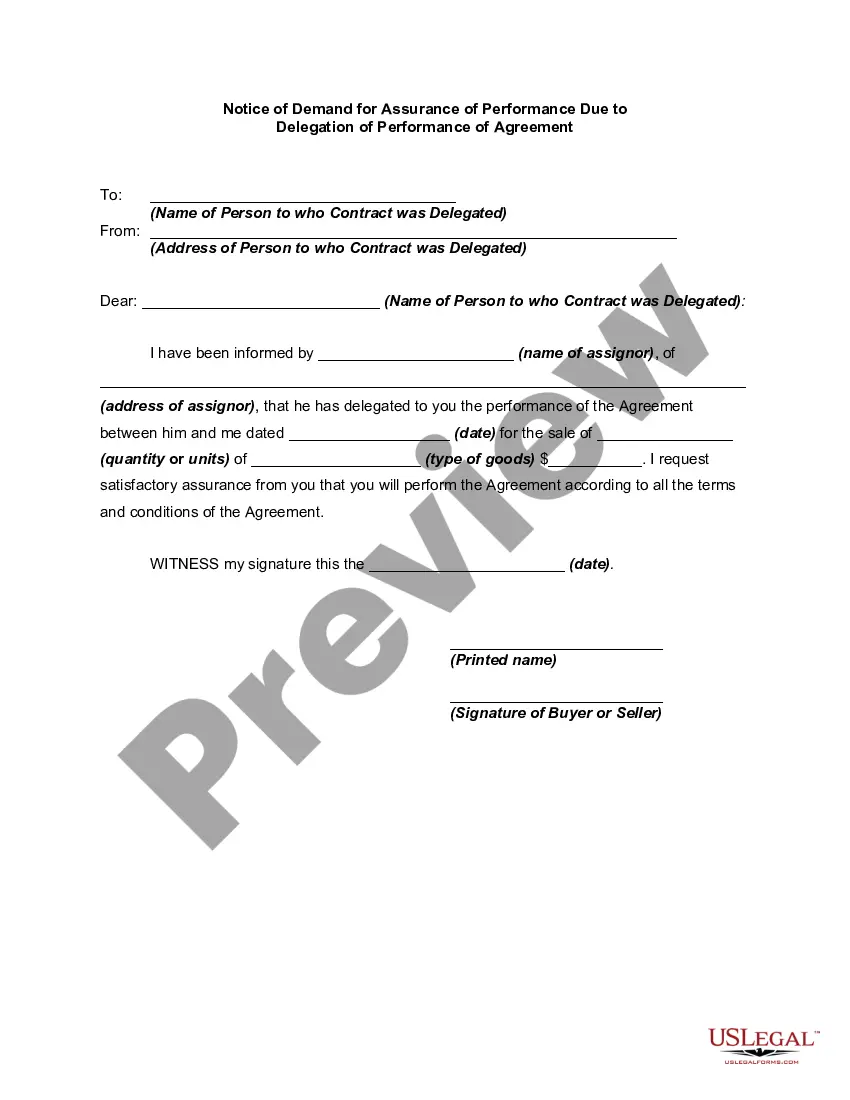
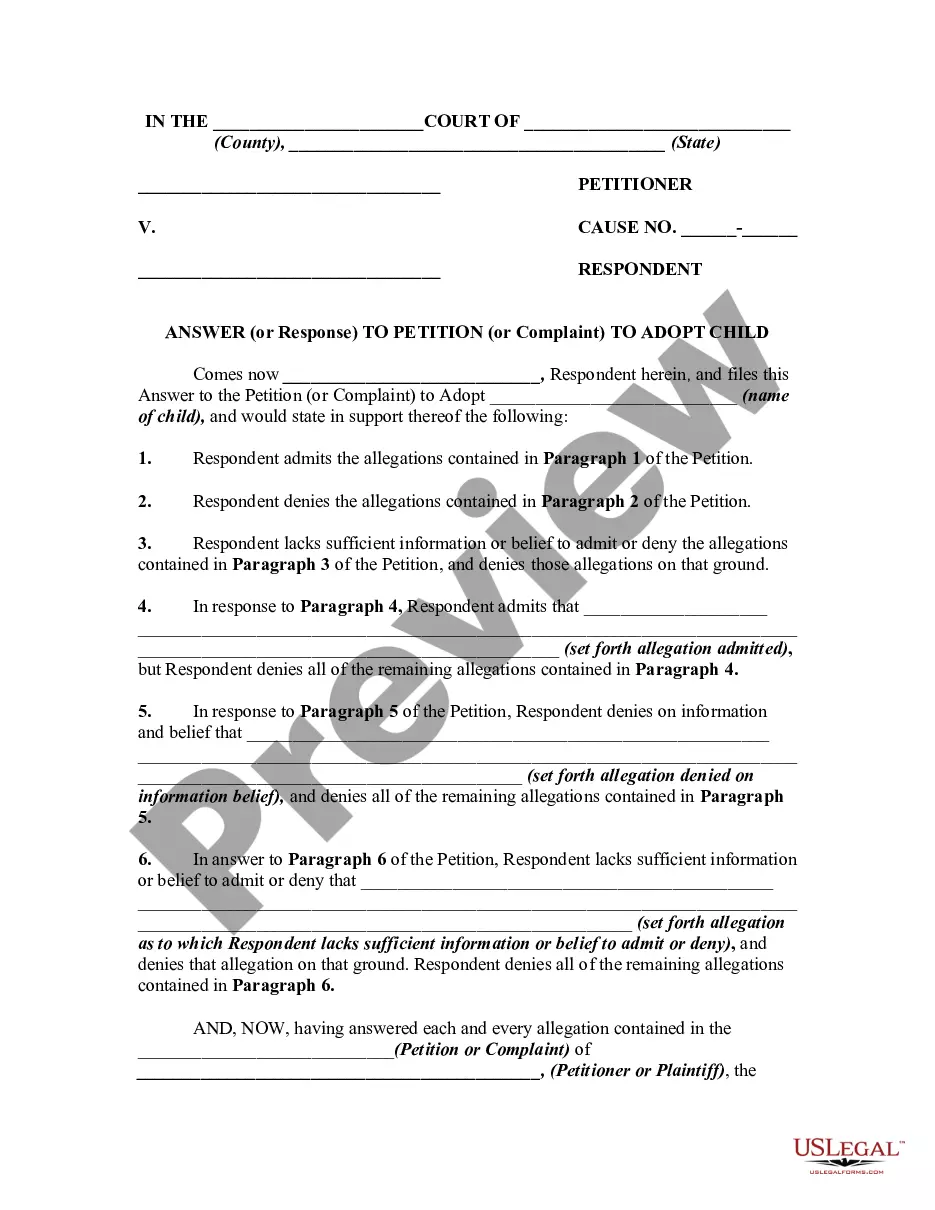
How to fill out Election Form For Continuation Of Benefits - COBRA?
Selecting the ideal legal document template may be a challenge.
Certainly, there are many templates accessible on the web, but how can you obtain the specific legal form you require.
Utilize the US Legal Forms website. The platform provides thousands of templates, including the Minnesota Election Form for Continuation of Benefits - COBRA, which you can employ for business and personal purposes.
You can preview the form using the Preview button and review the form description to confirm it suits your needs.
- All templates are vetted by experts and comply with state and federal guidelines.
- If you are already registered, Log In to your account and click the Download button to retrieve the Minnesota Election Form for Continuation of Benefits - COBRA.
- Utilize your account to search through the legal forms you have acquired previously.
- Visit the My documents tab of your account and obtain another copy of the document you need.
- If you are a new user of US Legal Forms, here are some simple instructions for you to follow.
- First, ensure you have selected the appropriate form for your specific city/state.
Form popularity
FAQ
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
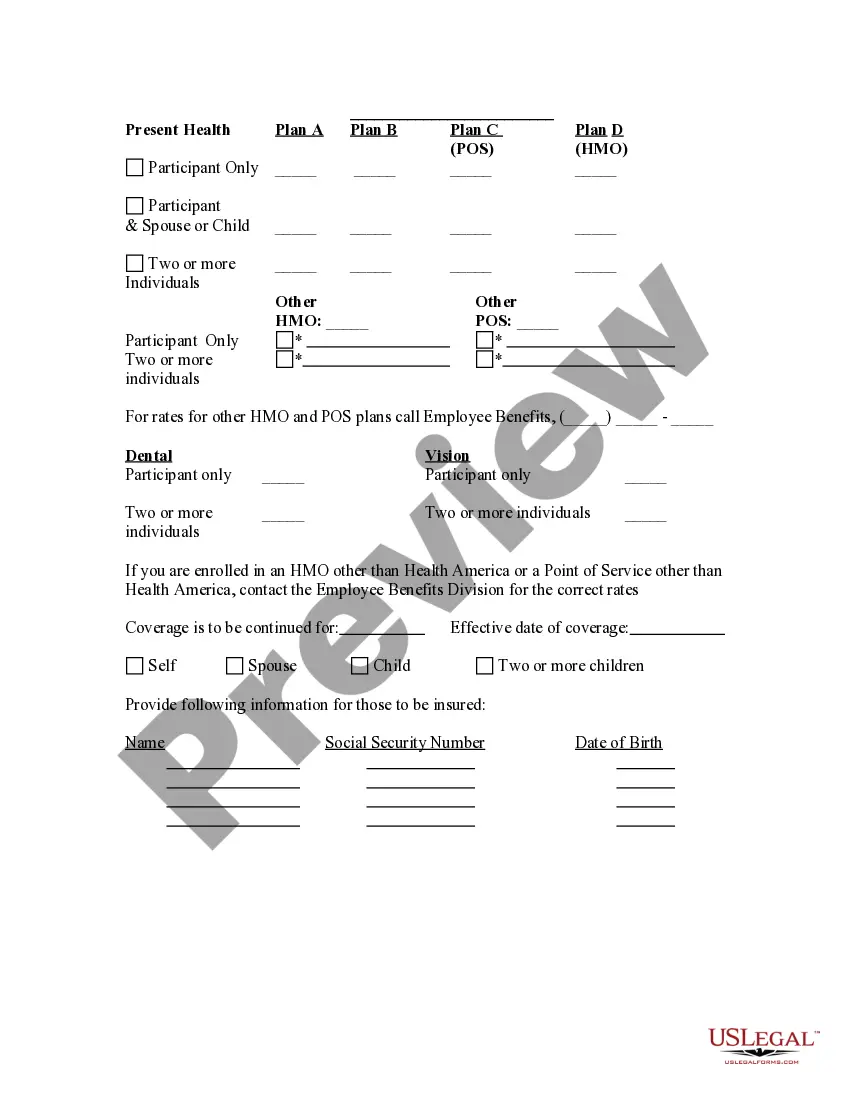
The length of continuation depends on the qualifying event. Legal separation or divorce - dependent children can continue up to 36 months under federal law. Under Minnesota law, they can continue until they become covered under another group plan, or until they no longer qualify as dependents under state law.
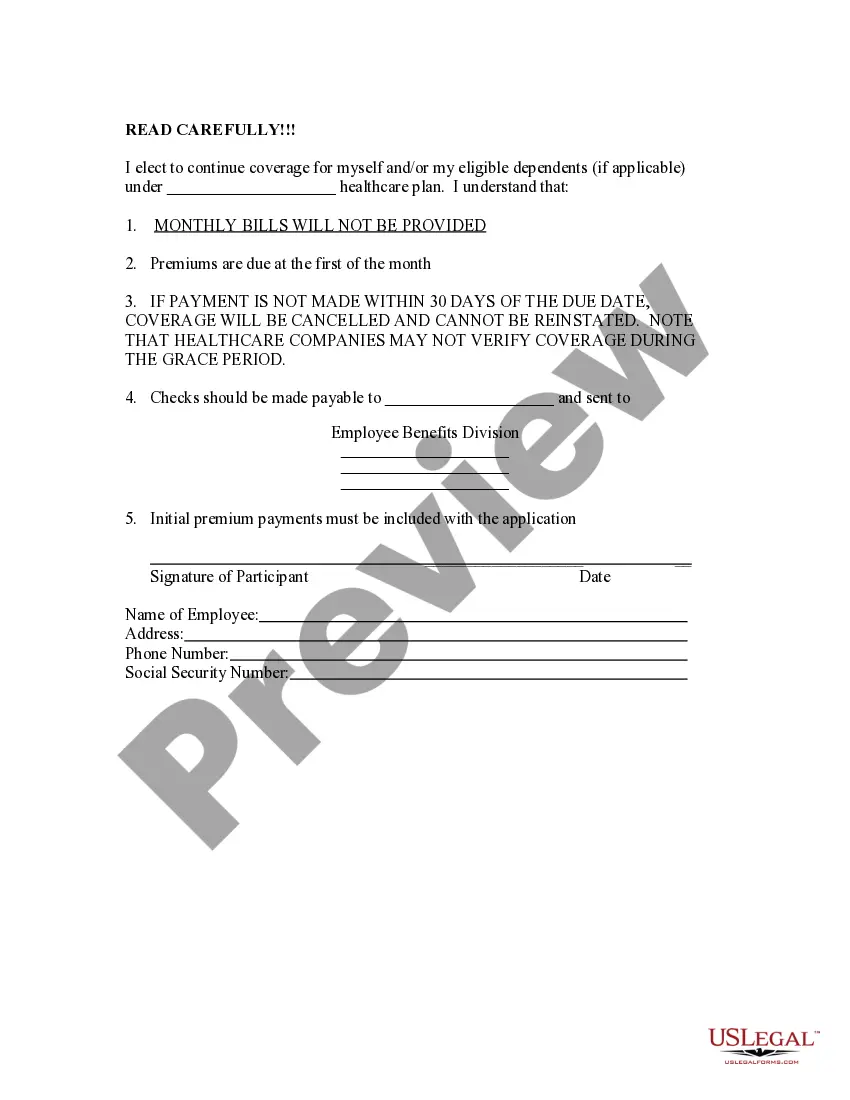
The general notice describes general COBRA rights and employee obligations. This notice must be provided to each covered employee and each covered spouse of an employee who becomes covered under the plan. The notice must be provided within the first 90 days of coverage under the group health plan.
COBRA continuation coverage lets you stay on your employer's group health insurance plan after leaving your job. COBRA stands for the Consolidated Omnibus Budget Reconciliation Act. It's shorthand for the law change that required employers to extend temporary group health insurance to departing employees.
COBRA the Consolidated Omnibus Budget Reconciliation Act -- requires group health plans to offer continuation coverage to covered employees, former employees, spouses, former spouses, and dependent children when group health coverage would otherwise be lost due to certain events.
Cal-COBRA is a California Law that lets you keep your group health plan when your job ends or your hours are cut. It may also be available to people who have exhausted their Federal COBRA.
Federal law requires that most group health plans (including this Plan) give employees and their families the opportunity to continue their health care coverage through COBRA continuation coverage when there's a qualifying event that would result in a loss of coverage under an employer's plan.
If you are enrolled on your parent's coverage and turn 26, you are eligible to continue Medical and Dental benefits on COBRA for 36 months. Your first day of COBRA coverage will be the first of the month following the date you turn 26.