Maryland Notice from Employer to Employee Regarding Early Termination of Continuation Coverage
Description
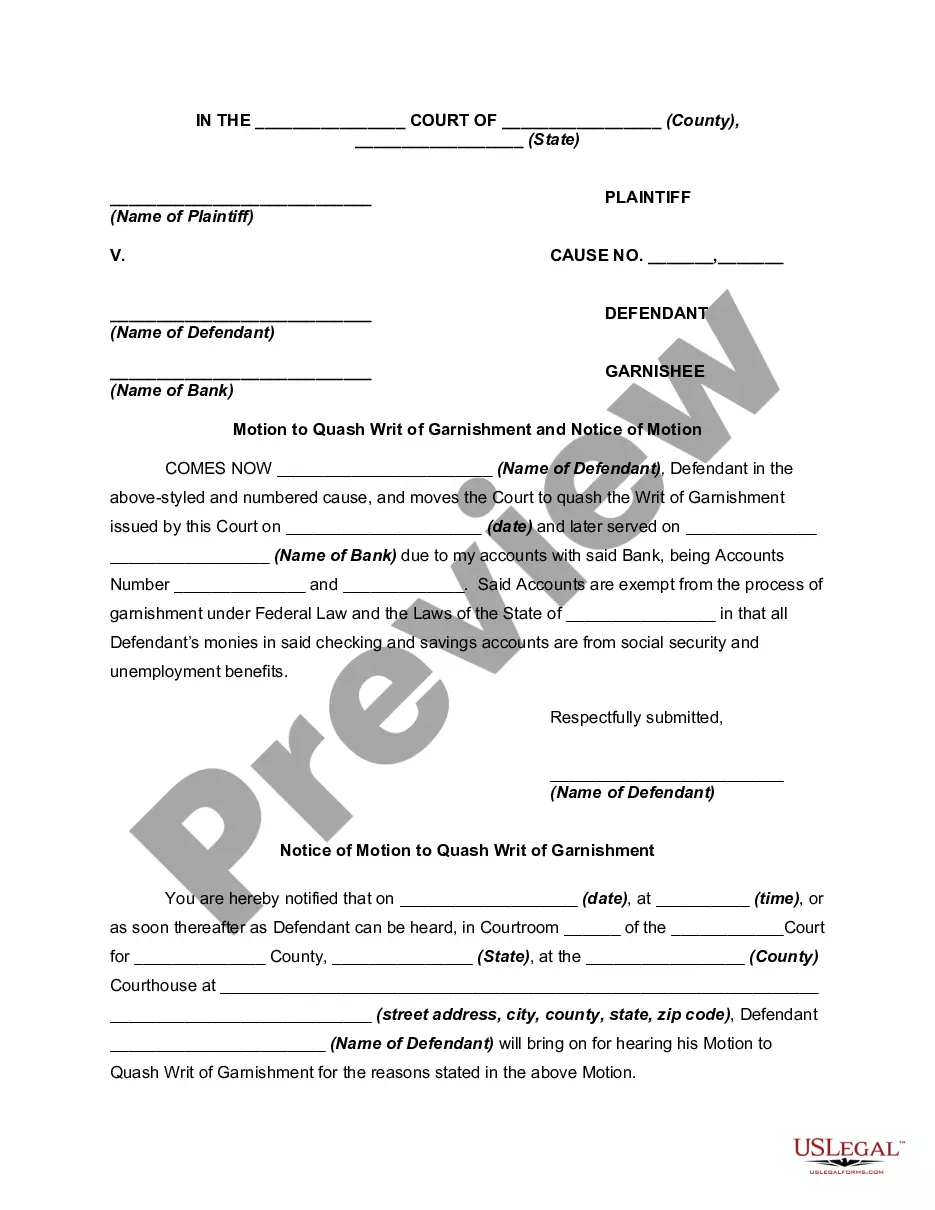
How to fill out Notice From Employer To Employee Regarding Early Termination Of Continuation Coverage?
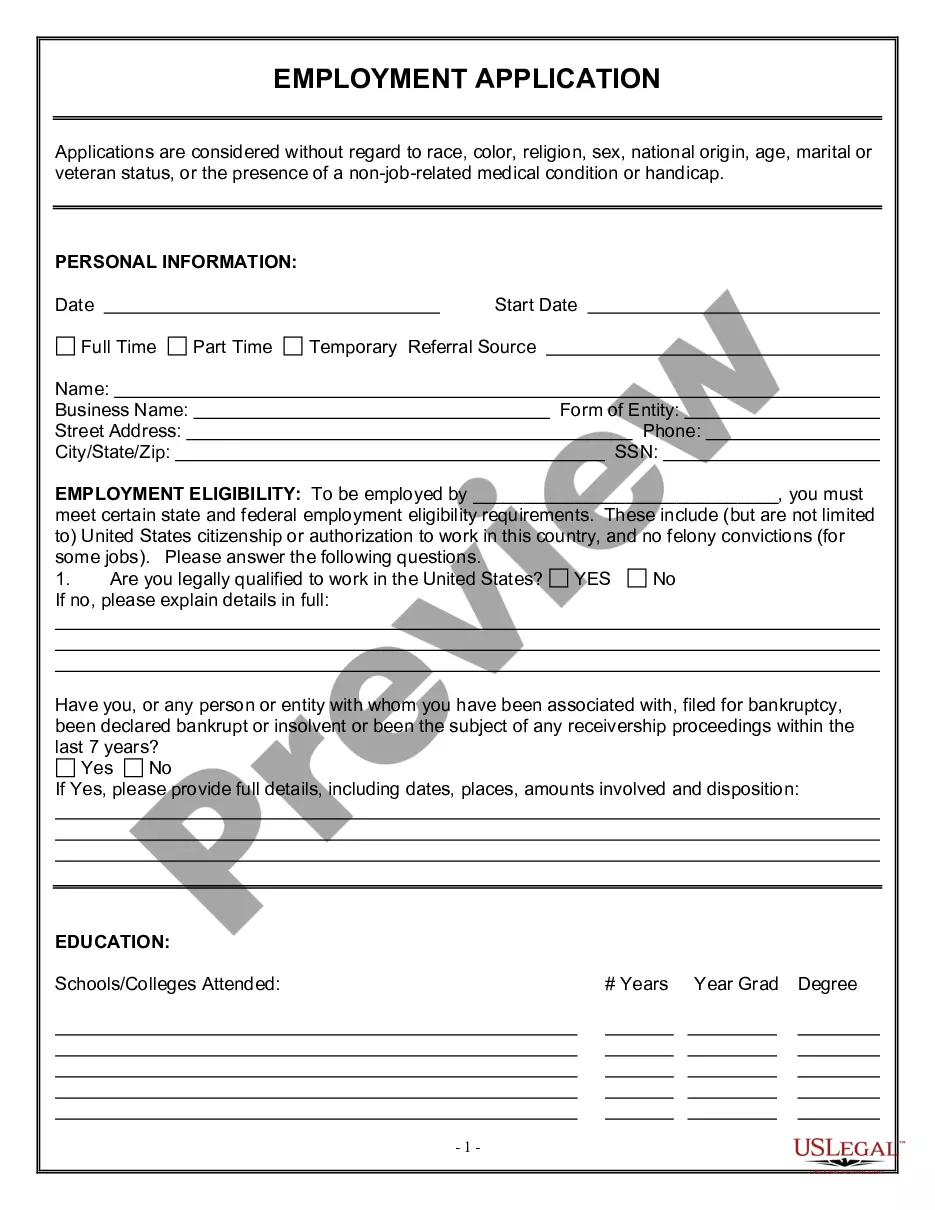
Are you currently in the location where you need to obtain documents for either business or personal reasons almost every day? There are numerous legal document templates available online, but finding ones that you can trust isn't easy.
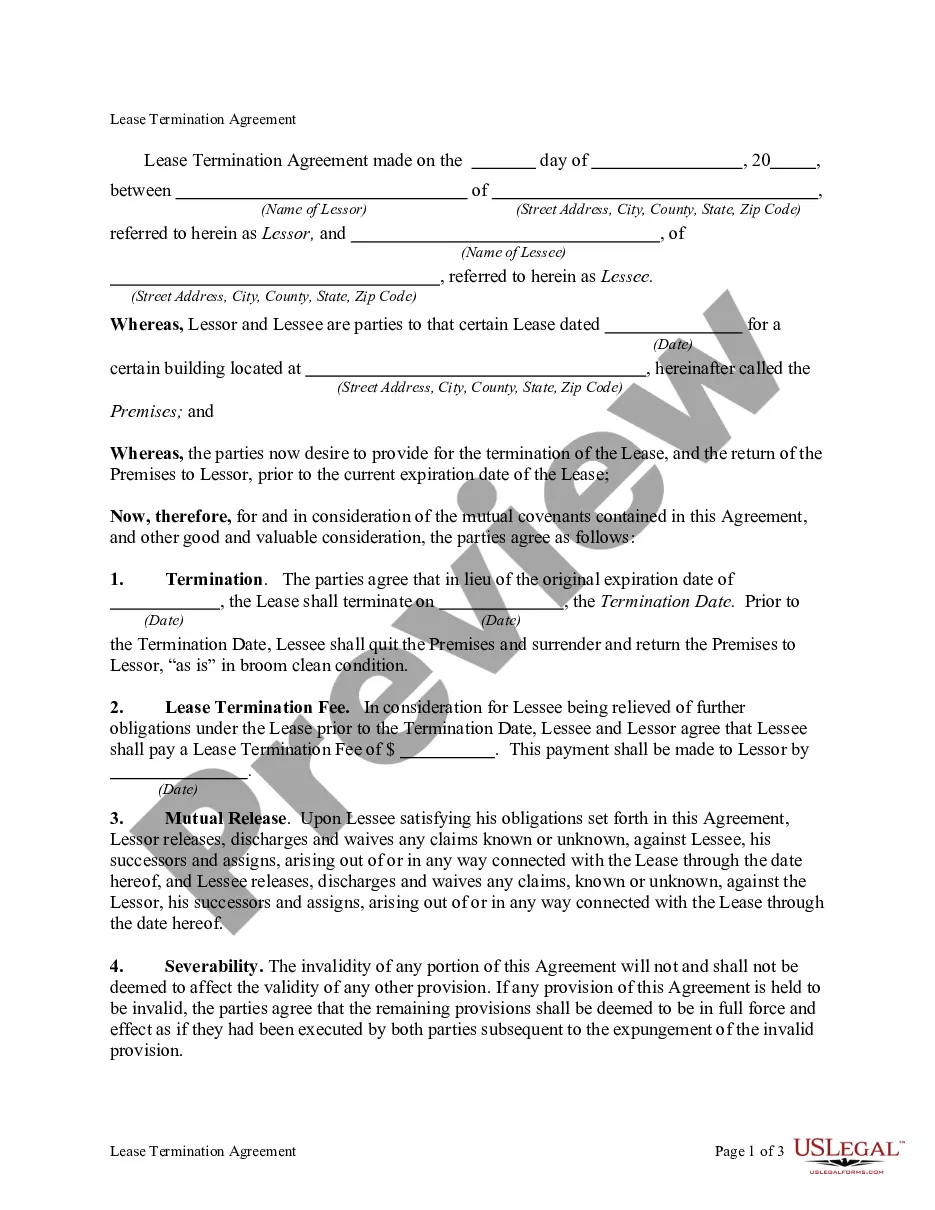
US Legal Forms provides thousands of template forms, such as the Maryland Notice from Employer to Employee Regarding Early Termination of Continuation Coverage, which are crafted to fulfill federal and state regulations.
If you are already familiar with the US Legal Forms website and possess an account, simply Log In. Then, you can download the Maryland Notice from Employer to Employee Regarding Early Termination of Continuation Coverage template.
- Obtain the form you need and ensure it is for the correct area/county.
- Use the Review button to inspect the document.
- Check the summary to ensure you have selected the right form.
- If the document isn't what you seek, use the Search field to find the form that satisfies your needs and requirements.
- Once you locate the correct template, click Acquire now.
- Select the pricing plan you desire, fill in the required information to create your account, and complete the payment using your PayPal or credit card.
- Choose a suitable document format and download your copy.
Form popularity
FAQ
Federal COBRA is a federal law that lets you keep your group health plan when your job ends or your hours are cut. Federal COBRA requires continuation coverage be offered to covered employees, their spouses, former spouses, and dependent children.
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
When the qualifying event is the covered employee's termination of employment or reduction in hours of employment, qualified beneficiaries are entitled to 18 months of continuation coverage.
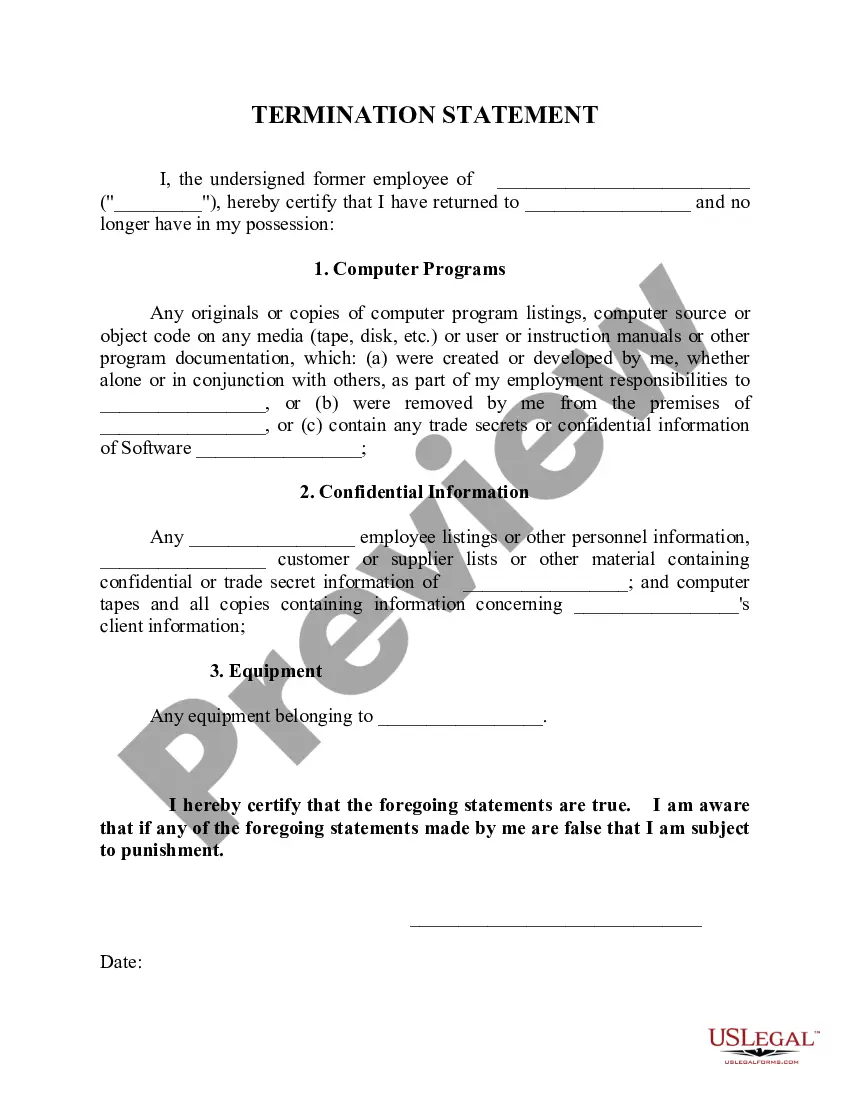
You May Cancel COBRA At Any Time To cancel your your COBRA coverage you will need to notify your previous employer or the plan administrator in writing. After you stop your COBRA insurance, your former employer should send you a letter affirming termination of that health insurance.
The Consolidated Omnibus Budget Reconciliation Act of 1986 (COBRA) amended the Public Health Service Act, the Internal Revenue Code and the Employee Retirement Income Security Act (ERISA) to require employers with 20 or more employees to provide temporary continuation of group health coverage in certain situations
Federal law requires that most group health plans (including this Plan) give employees and their families the opportunity to continue their health care coverage through COBRA continuation coverage when there's a qualifying event that would result in a loss of coverage under an employer's plan.
The general notice describes general COBRA rights and employee obligations. This notice must be provided to each covered employee and each covered spouse of an employee who becomes covered under the plan. The notice must be provided within the first 90 days of coverage under the group health plan.
If you are entitled to elect COBRA continuation coverage, you must be given an election period of at least 60 days (starting on the later of the date you are furnished the election notice or the date you would lose coverage) to choose whether or not to elect continuation coverage.
State continuation coverage refers to state laws that enable employees to extend their employer-sponsored group health insurance even if they are not eligible for an extension through COBRA. While COBRA law applies throughout the U.S., it is only applicable to employers with 20 or more employees.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,