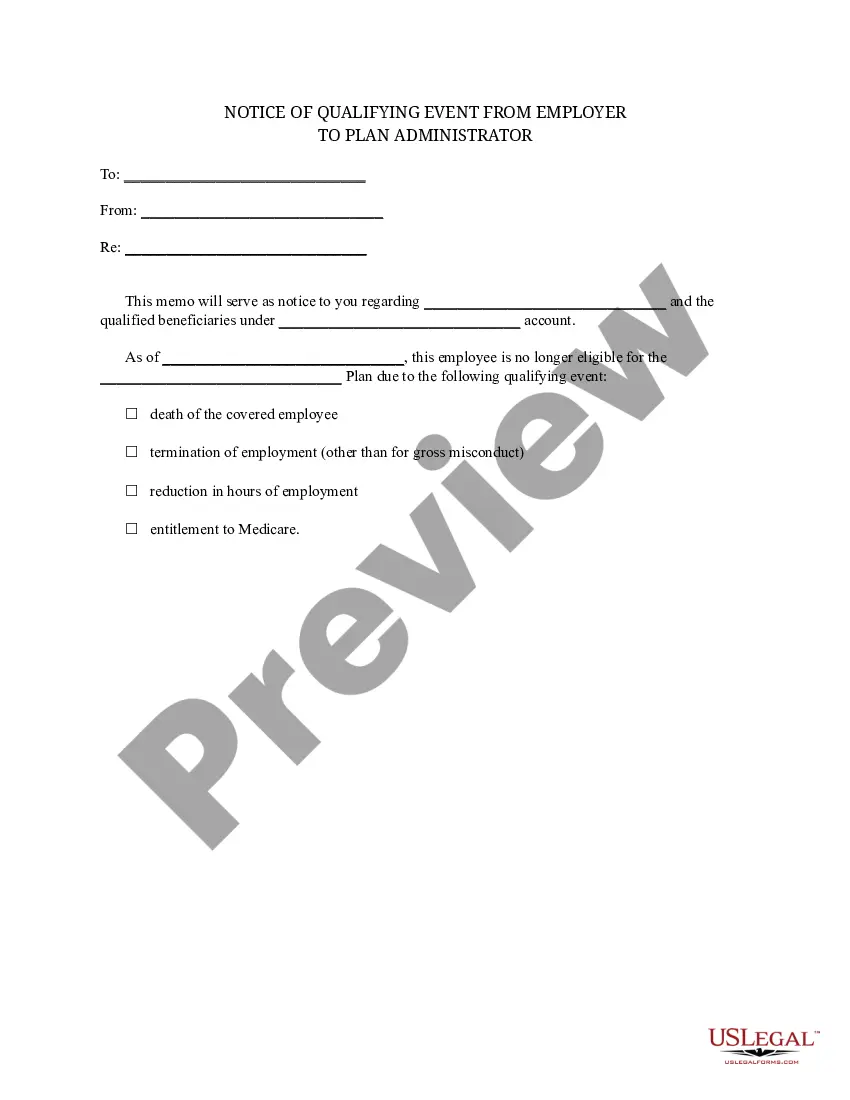
Massachusetts Notice of Qualifying Event from Employer to Plan Administrator
Description
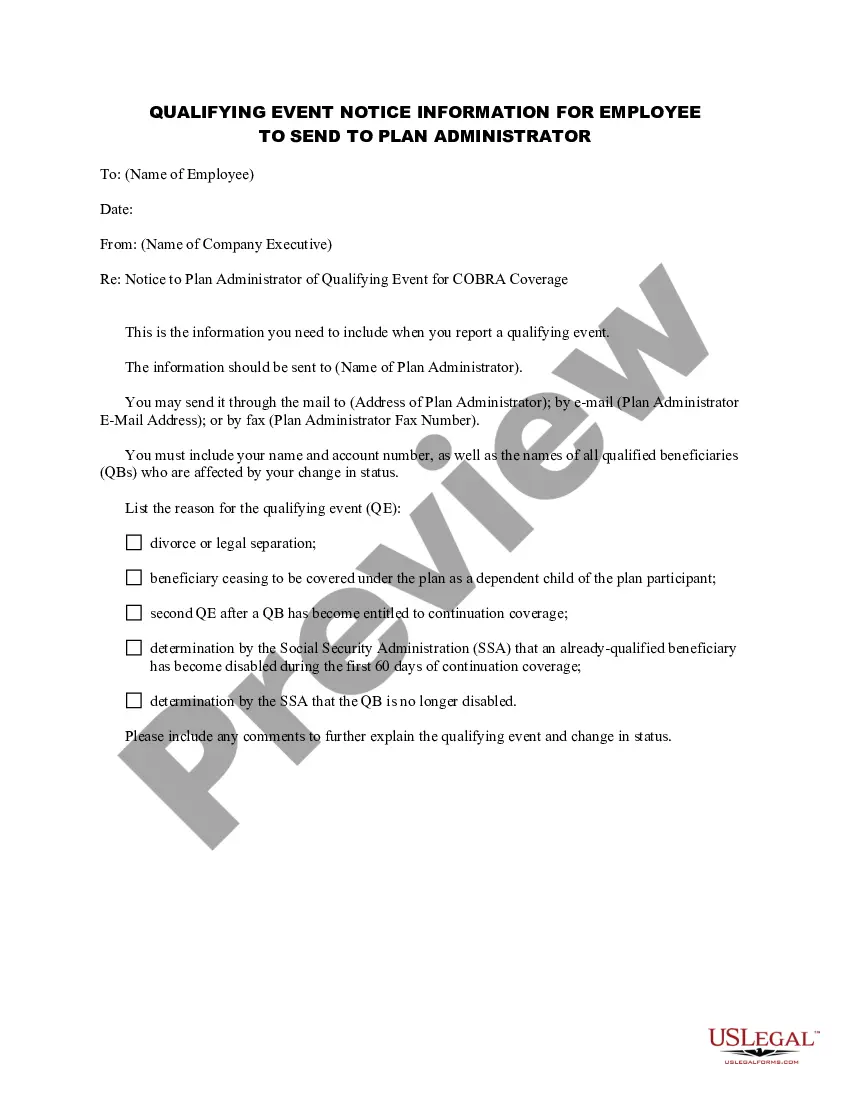
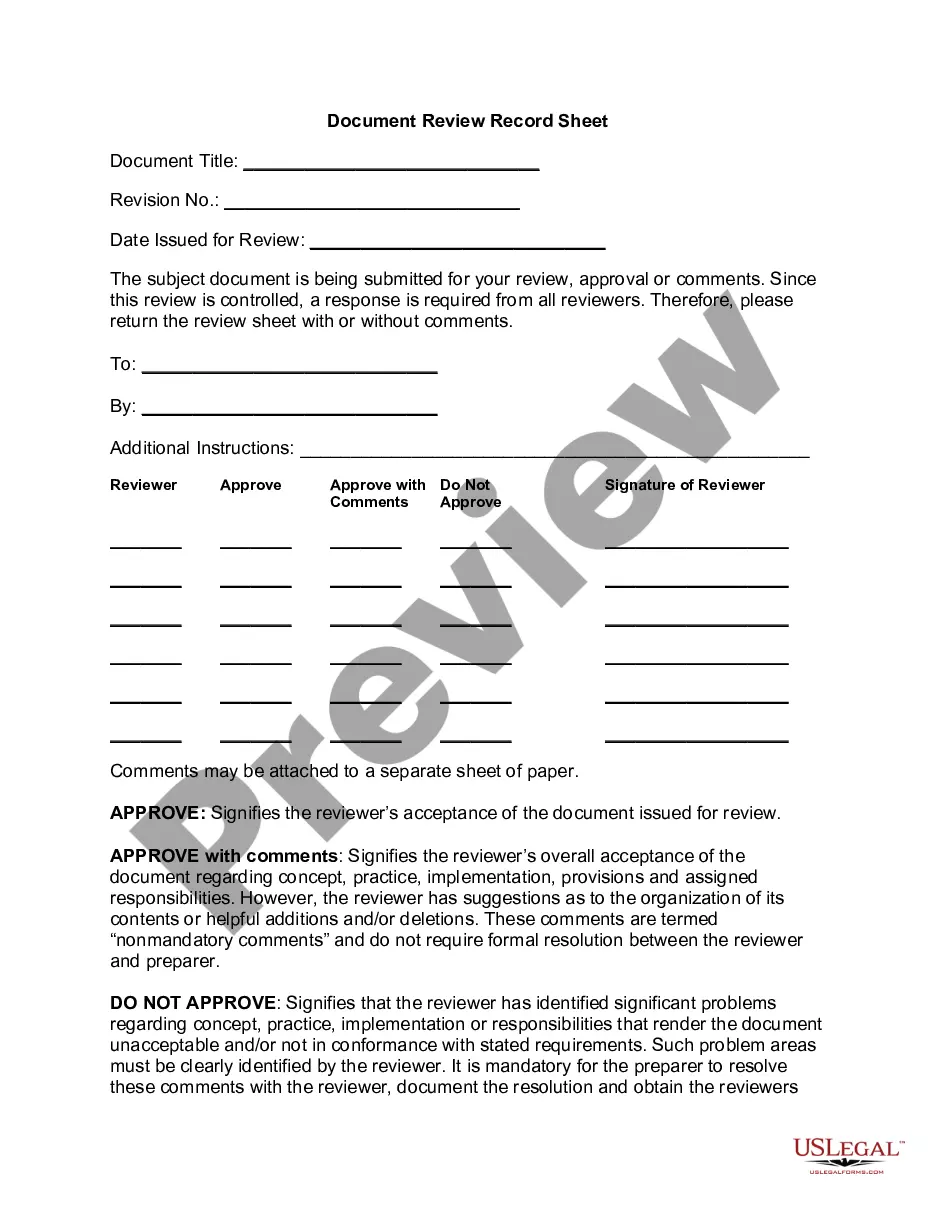
How to fill out Notice Of Qualifying Event From Employer To Plan Administrator?
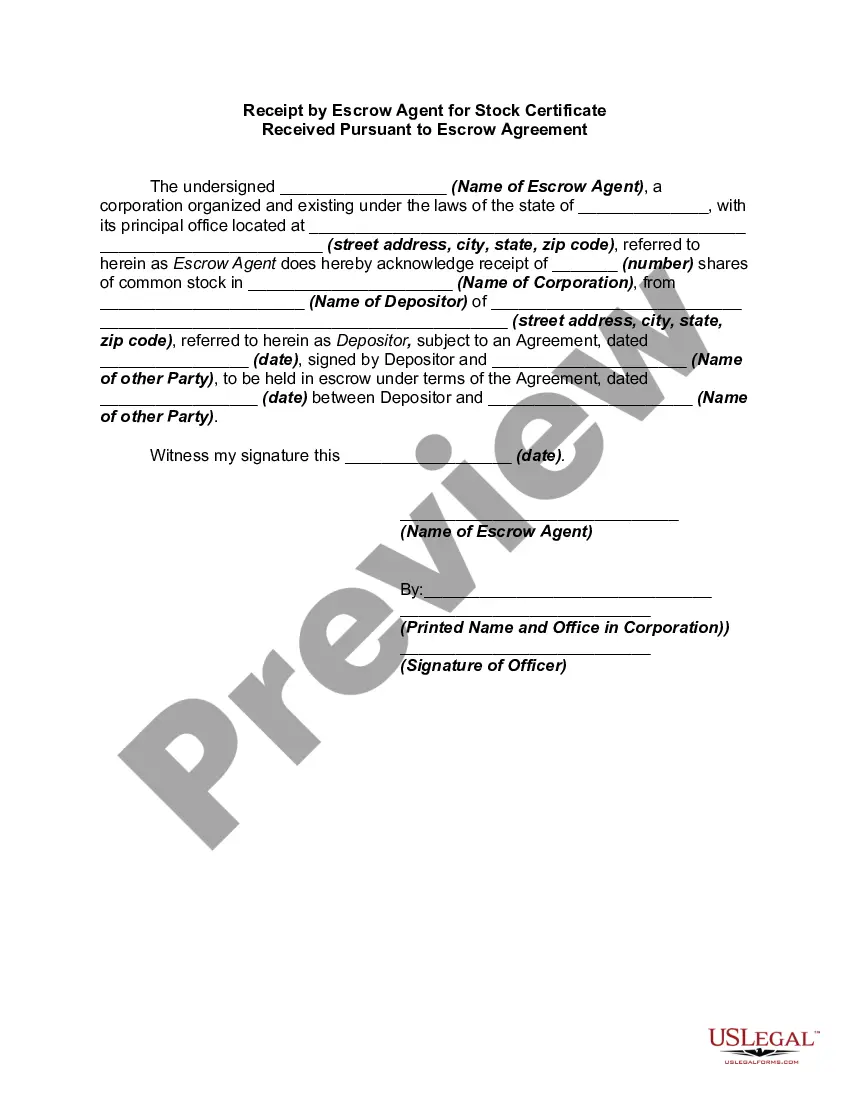
US Legal Forms - one of the largest collections of legal documents in the United States - offers a diverse selection of legal form templates available for download or printing.
By utilizing the website, you can obtain numerous forms for business and personal purposes, organized by categories, states, or keywords.
You can access the latest versions of forms such as the Massachusetts Notice of Qualifying Event from Employer to Plan Administrator in just a few minutes.
Click the Review button to examine the contents of the form. Check the form description to confirm you have selected the appropriate form.
If the form does not meet your needs, use the Search field at the top of the screen to find the one that does.
- If you already have an account, Log In to download the Massachusetts Notice of Qualifying Event from Employer to Plan Administrator from the US Legal Forms library.
- The Download button appears on every form you view.
- You have access to all previously downloaded forms in the My documents section of your profile.
- If you are using US Legal Forms for the first time, here are some simple steps to get you started.
- Ensure you have selected the correct form for your city/state.
Form popularity
FAQ
Your employer may have just begun offering a health insurance plan. Your employer may have recently hired several new employees, and the increase in the number of employees may force your employer to follow these regulations for the first time.
If You Do Not Receive Your COBRA PaperworkReach out to the Human Resources Department and ask for the COBRA Administrator. They may use a third-party administrator to handle your enrollment. If the employer still does not comply you can call the Department of Labor at 1-866-487-2365.
DOL ERISA Penalties An employer is liable up to an additional $110 per day per participant if they fail to provide initial COBRA notices. ERISA can also hold any fiduciary personally liable for non-compliance.
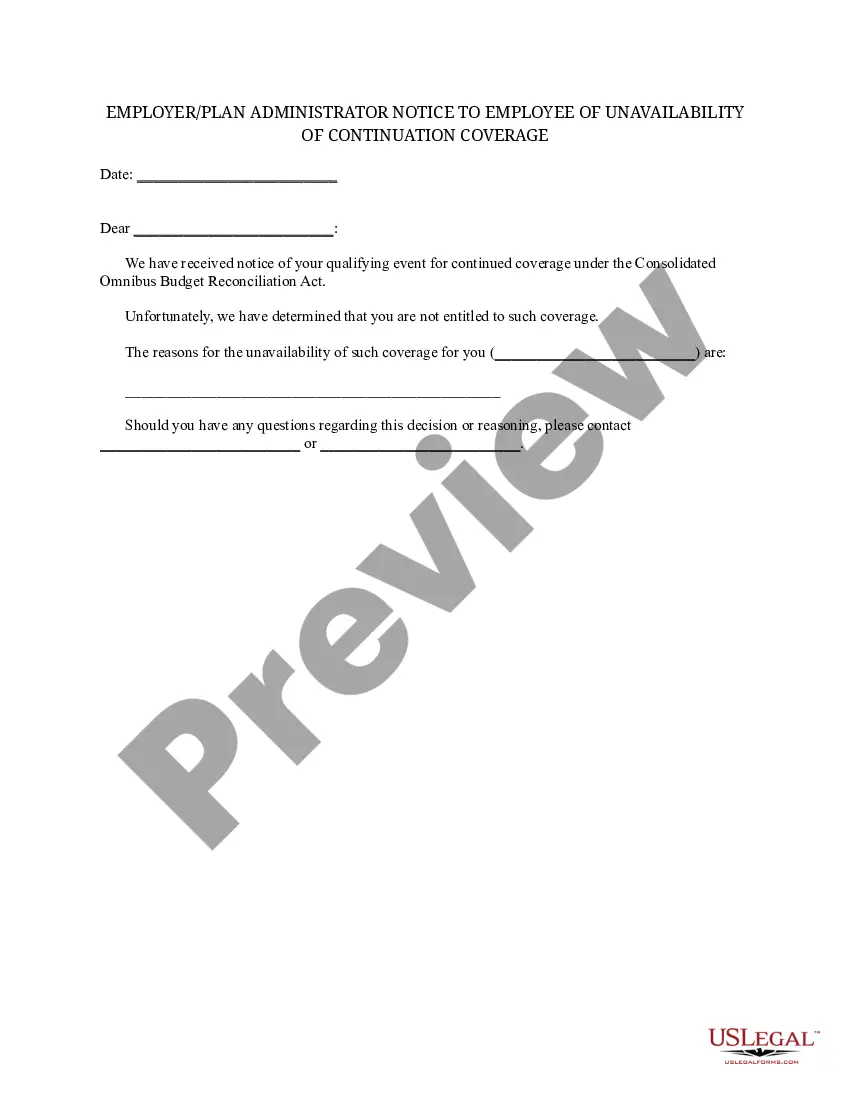
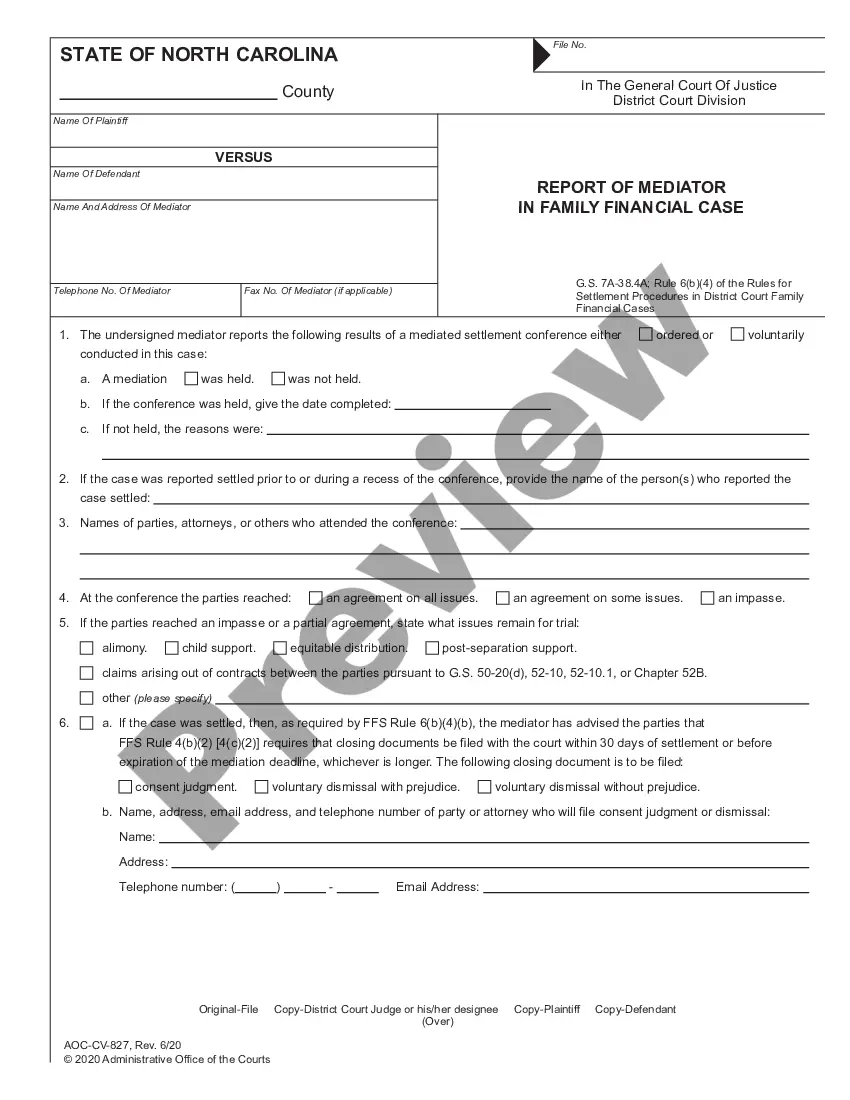
Second qualifying events may include the death of the covered employee, divorce or legal separation from the covered employee, the covered employee becoming entitled to Medicare benefits (under Part A, Part B or both), or a dependent child ceasing to be eligible for coverage as a dependent under the group health plan.
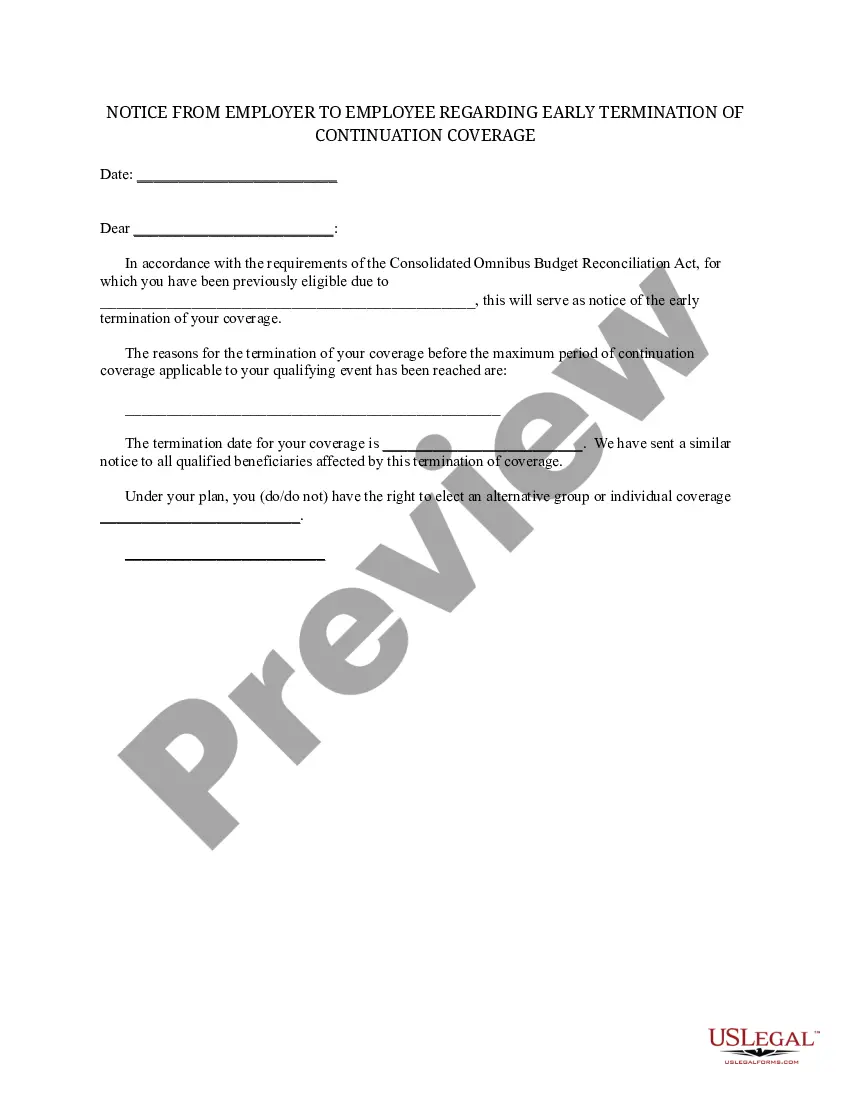
Losing COBRA Benefits Here's the good news: Rolling off of COBRA coverage is a qualifying event that opens a special enrollment period for you to purchase your own health coverage. And you'll have more options, flexibility and control of your health plan outside of COBRA with an individual health insurance plan.
The following are qualifying events: the death of the covered employee; a covered employee's termination of employment or reduction of the hours of employment; the covered employee becoming entitled to Medicare; divorce or legal separation from the covered employee; or a dependent child ceasing to be a dependent under
When the qualifying event is the covered employee's termination of employment or reduction in hours of employment, qualified beneficiaries are entitled to 18 months of continuation coverage.
COBRA Qualifying Event Notice The employer must notify the plan if the qualifying event is: Termination or reduction in hours of employment of the covered employee, 2022 Death of the covered employee, 2022 Covered employee becoming entitled to Medicare, or 2022 Employer bankruptcy.
Employers do not have to offer COBRA coverage to: Employees who are not yet eligible for a group health plan. Eligible employees who declined to participate in a group health plan. Individuals who are enrolled for benefits under Medicare.
COBRA is a federal law and is not enforced by the Division of Insurance. Mini-COBRA is a state law and is enforced by the Division of Insurance. COBRA generally applies to group health plans offered by employers with 20 or more employees.