Louisiana Summary of Rights and Obligations under COBRA
Description
How to fill out Summary Of Rights And Obligations Under COBRA?
Finding the appropriate legally authorized file template can be challenging. Naturally, there are numerous layouts accessible on the web, but how can you locate the authorized type you need? Utilize the US Legal Forms platform. The service offers a vast array of templates, such as the Louisiana Summary of Rights and Obligations under COBRA, which you can employ for both business and personal purposes. All documents are reviewed by professionals and comply with federal and state regulations.
If you are already a member, Log In to your account and click on the Acquire button to obtain the Louisiana Summary of Rights and Obligations under COBRA. Use your account to check the legal forms you may have previously obtained. Navigate to the My documents section of your account to download another copy of the document you require.
If you are a new customer of US Legal Forms, here are simple instructions that you should follow: First, ensure that you have chosen the correct form for your city/region. You can view the document using the Preview button and read the form description to confirm that it meets your needs. If the form does not fulfill your requirements, utilize the Search field to find the appropriate kind. Once you are confident that the document is suitable, click the Acquire now button to purchase the form. Select the pricing plan you prefer and fill in the necessary information. Create your account and complete the payment using your PayPal account or credit card. Choose the file format and download the legal file template to your device. Finally, complete, edit, and print as well as sign the obtained Louisiana Summary of Rights and Obligations under COBRA.
- US Legal Forms is the largest database of legal documents where you can find various form layouts.
- Utilize the service to download professionally crafted documents that comply with state regulations.
Form popularity
FAQ
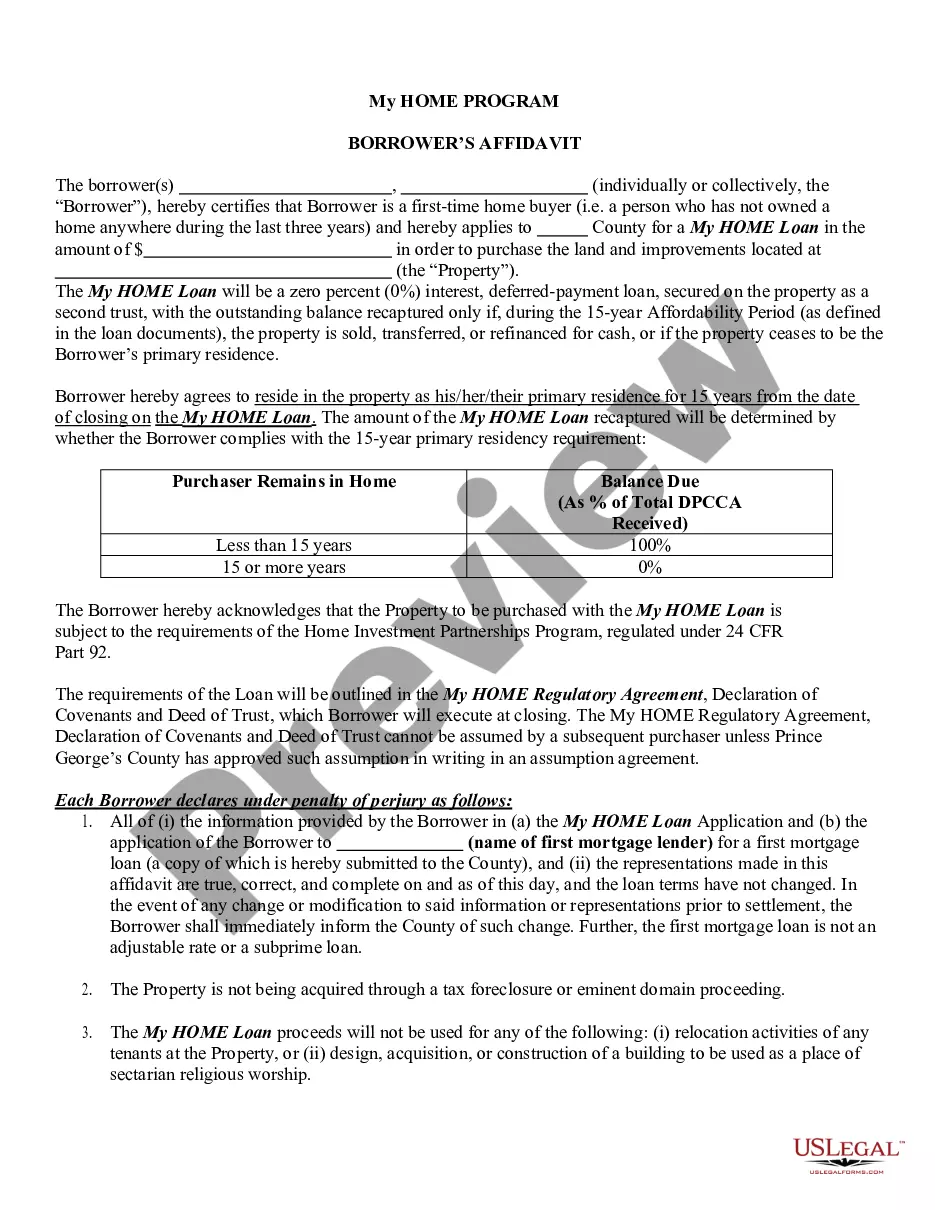
The Federal COBRA Act is in place for companies with 20 or more employees. The law requires employers to provide a notice of continuation within 45 days of qualifying event that would have stopped that workers insurance. Qualified beneficiaries may remain on COBRA insurance for up to 18 months.
On Average, The Monthly COBRA Premium Cost Is $400 700 Per Person. Continuing on an employer's major medical health plan with COBRA is expensive.
Q3: Which employers are required to offer COBRA coverage? COBRA generally applies to all private-sector group health plans maintained by employers that had at least 20 employees on more than 50 percent of its typical business days in the previous calendar year.
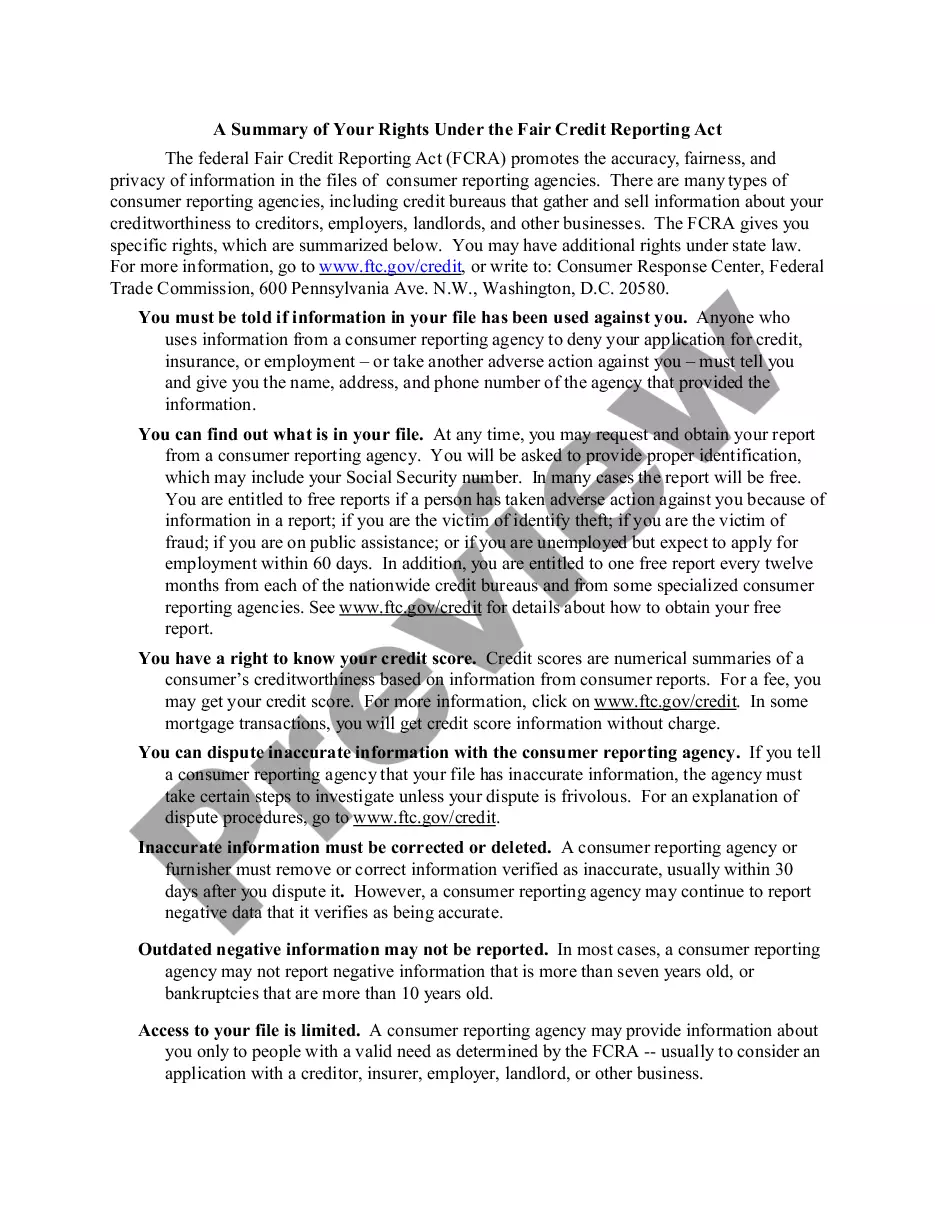
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
COBRA is a federal law about health insurance. If you lose or leave your job, COBRA lets you keep your existing employer-based coverage for at least the next 18 months. Your existing healthcare plan will now cost you more. Under COBRA, you pay the whole premium including the share your former employer used to pay.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) is a federal law passed in 1986 that lets certain employees, their spouses, and their dependents keep group health plan (GHP) coverage for 18 to 36 months after they leave their job or lose coverage for certain other reasons, as long as they pay the full cost
The Consolidated Omnibus Budget Reconciliation Act (COBRA) Passed in 1985, COBRA is a federal law that allows employees of certain companies to continue their health insurance with the same benefits even after they stop working for their employer.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
The following are qualifying events: the death of the covered employee; a covered employee's termination of employment or reduction of the hours of employment; the covered employee becoming entitled to Medicare; divorce or legal separation from the covered employee; or a dependent child ceasing to be a dependent under