Kentucky Notice from Employer to Employee Regarding Early Termination of Continuation Coverage
Description
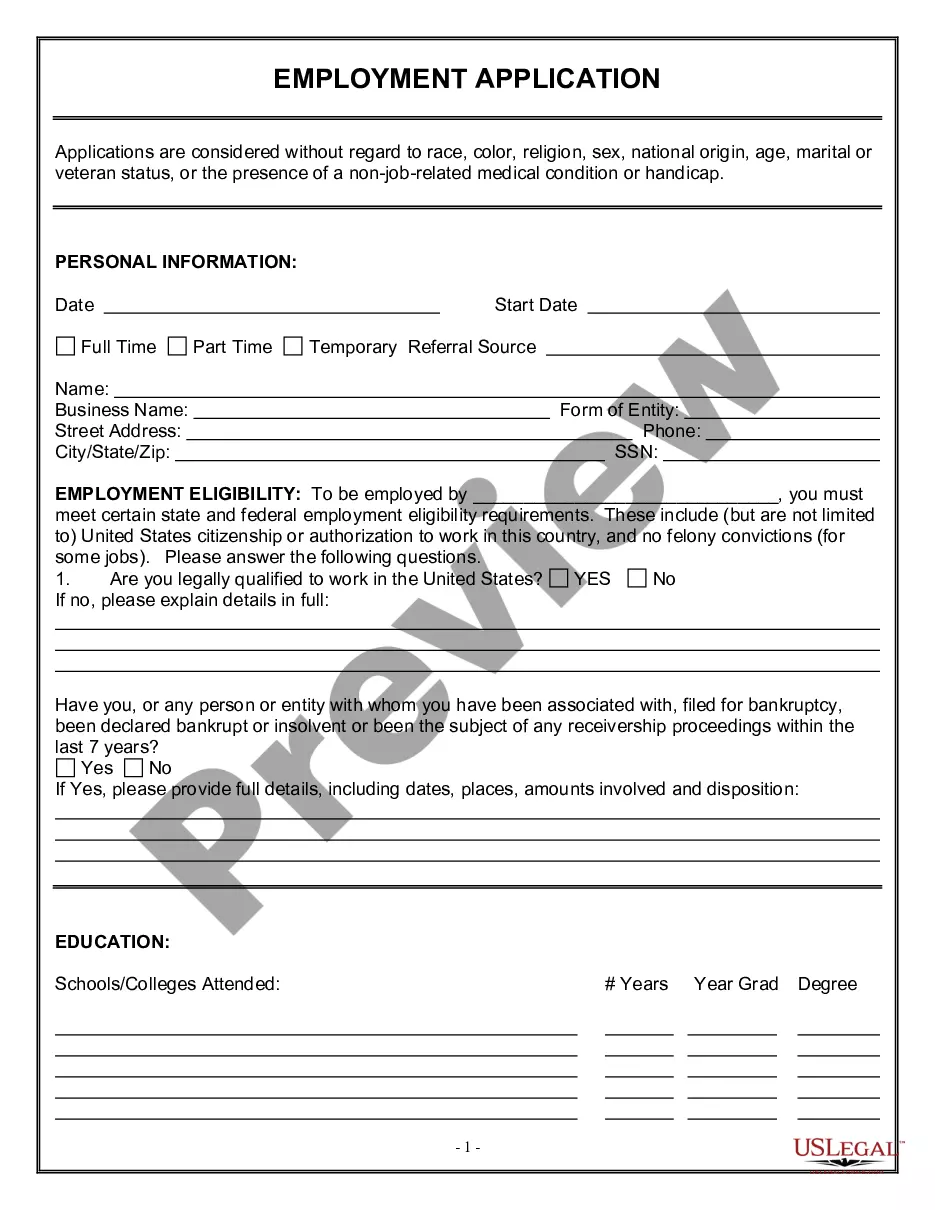
How to fill out Notice From Employer To Employee Regarding Early Termination Of Continuation Coverage?
US Legal Forms - one of the most significant libraries of authorized kinds in America - offers an array of authorized record layouts you can download or print out. While using internet site, you will get 1000s of kinds for organization and individual purposes, categorized by groups, suggests, or keywords and phrases.You will discover the most recent versions of kinds like the Kentucky Notice from Employer to Employee Regarding Early Termination of Continuation Coverage within minutes.
If you have a registration, log in and download Kentucky Notice from Employer to Employee Regarding Early Termination of Continuation Coverage from your US Legal Forms local library. The Download key will show up on each and every form you look at. You have access to all formerly delivered electronically kinds in the My Forms tab of your respective accounts.
If you would like use US Legal Forms initially, listed here are simple directions to help you get started out:
- Ensure you have chosen the correct form for your personal town/area. Click on the Preview key to examine the form`s content. Look at the form explanation to ensure that you have selected the appropriate form.
- If the form does not match your needs, use the Look for discipline towards the top of the screen to find the one that does.
- Should you be satisfied with the shape, validate your decision by visiting the Acquire now key. Then, pick the pricing program you want and give your accreditations to register for an accounts.
- Process the financial transaction. Make use of your charge card or PayPal accounts to finish the financial transaction.
- Select the format and download the shape in your gadget.
- Make modifications. Complete, change and print out and signal the delivered electronically Kentucky Notice from Employer to Employee Regarding Early Termination of Continuation Coverage.
Every design you put into your account does not have an expiry date and is also yours permanently. So, if you want to download or print out yet another duplicate, just check out the My Forms segment and click on around the form you require.
Obtain access to the Kentucky Notice from Employer to Employee Regarding Early Termination of Continuation Coverage with US Legal Forms, one of the most considerable local library of authorized record layouts. Use 1000s of expert and status-specific layouts that fulfill your business or individual needs and needs.
Form popularity
FAQ
COBRA (Consolidated Omnibus Budget Reconciliation Act of 1985) is a federal law that requires employers of 20 or more employees who offer health care benefits to offer the option of continuing this coverage to individuals who would otherwise lose their benefits due to termination of employment, reduction in hours or
COBRA (Consolidated Omnibus Budget Reconciliation Act of 1985) is a federal law that requires employers of 20 or more employees who offer health care benefits to offer the option of continuing this coverage to individuals who would otherwise lose their benefits due to termination of employment, reduction in hours or
In addition, employers can provide COBRA notices electronically (via email, text message, or through a website) during the Outbreak Period, if they reasonably believe that plan participants and beneficiaries have access to these electronic mediums.
The Consolidated Omnibus Budget Reconciliation Act, known as COBRA, is a federal law that allows employees to continue their employer-provided health insurance after they are laid off or fired, or they otherwise become ineligible for benefits (for example, because they quit or their hours are reduced below the
How Long Does COBRA Last After You Quit? You may remain on your former employer's COBRA insurance plan for up to 18 months. Depending on your circumstances you or your qualified dependents may be eligible for up to 36 months of continuing coverage.
Meet the Deadlines You should get a notice in the mail about your COBRA and Cal-COBRA rights. You have 60 days after being notified to sign up. If you are eligible for Federal COBRA and did not get a notice, contact your employer. If you are eligible for Cal-COBRA and did not get a notice, contact your health plan.
When the qualifying event is the covered employee's termination of employment or reduction in hours of employment, qualified beneficiaries are entitled to 18 months of continuation coverage.
COBRA Notice of Early Termination of Continuation Coverage Continuation coverage must generally be made available for a maximum period (18, 29, or 36 months).
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
Initial COBRA notices must generally be provided within 14 days of the employer notifying the third-party administrator (TPA) of a qualifying event.