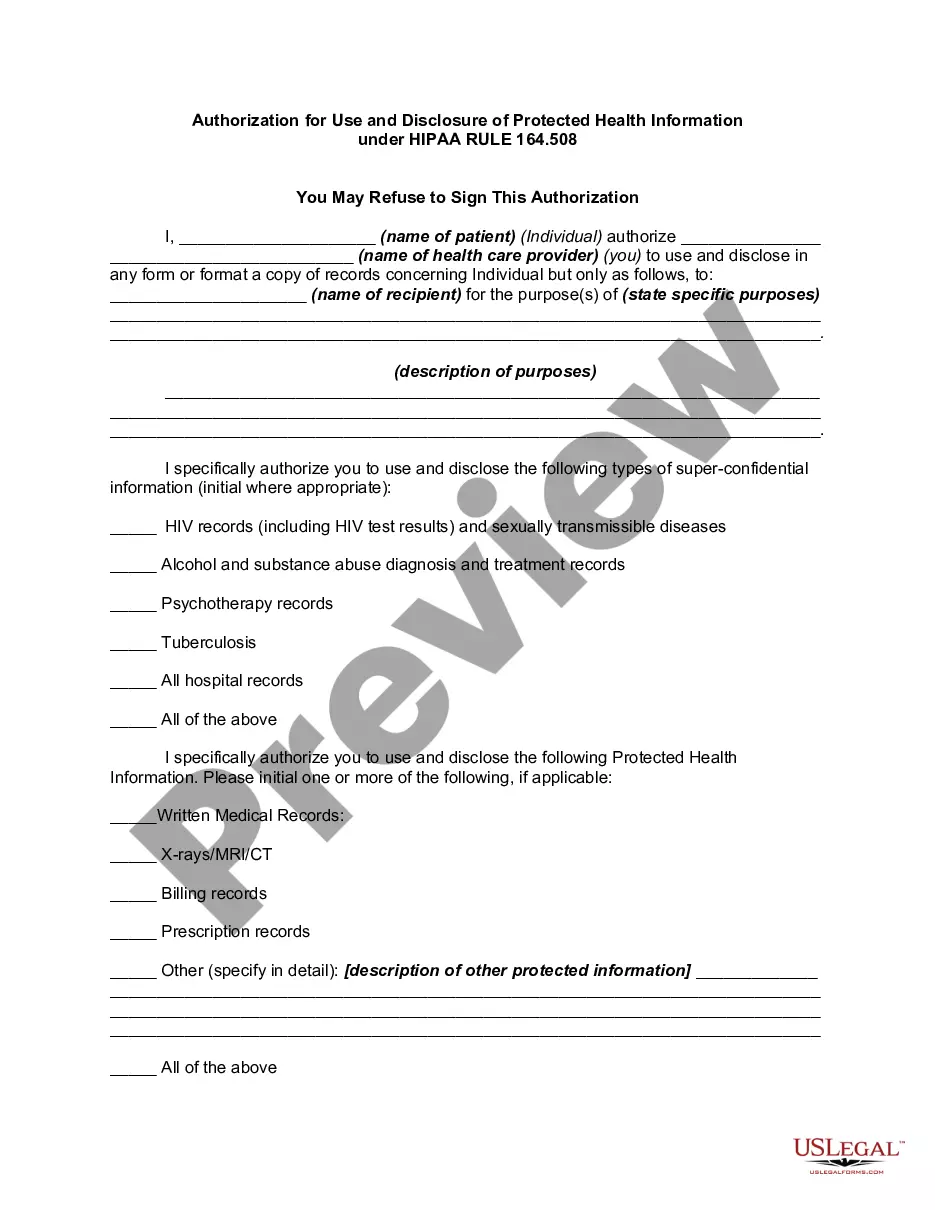
Under the Health Insurance Portability and Accountability Act of 1996 (HIPAA) and the Privacy Regulations written pursuant to the Act, the general rule is that covered entities may not use or disclose an individual's protected health information for purposes unrelated to treatment, payment, healthcare operations, or certain defined exceptions without first obtaining the individual's prior written authorization.
Kentucky Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508
Description
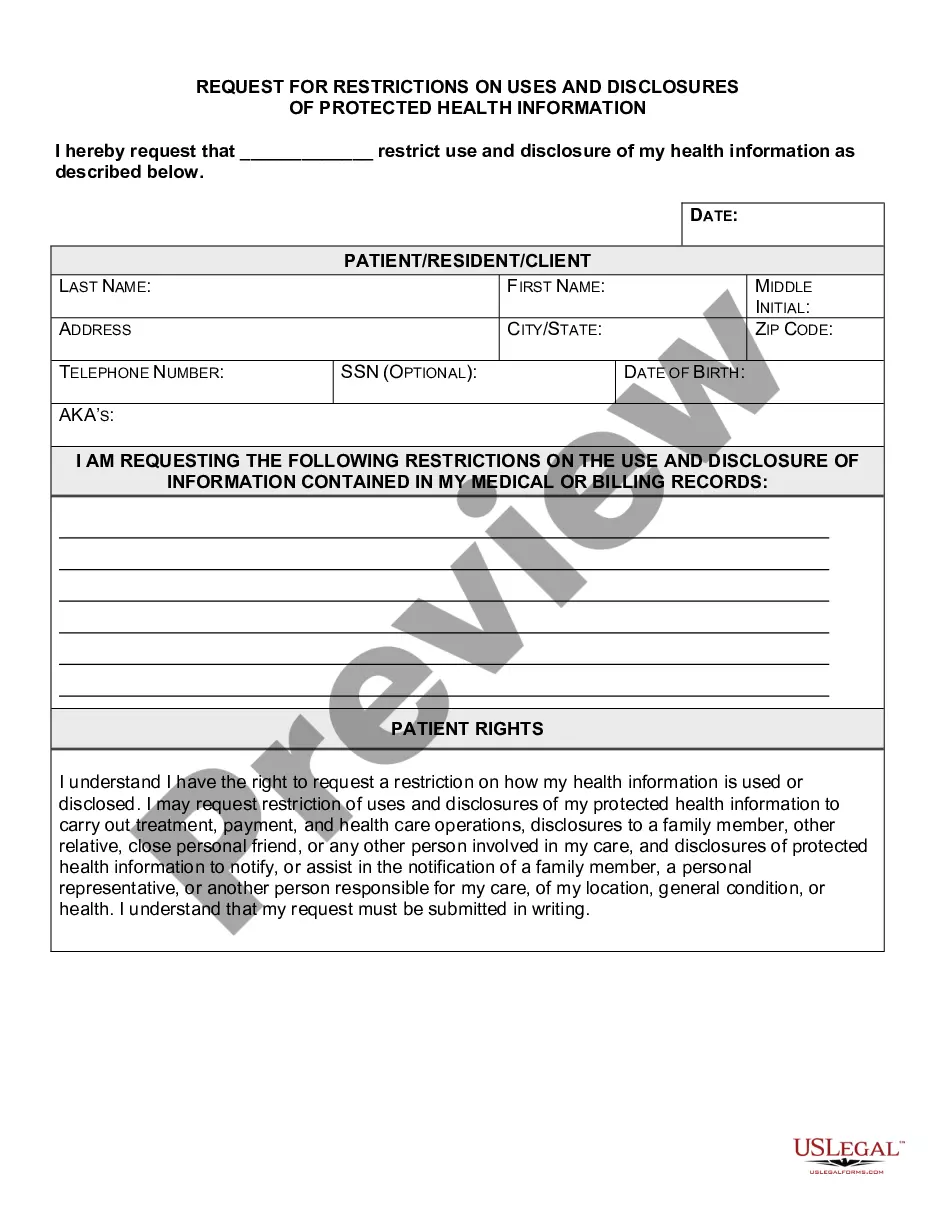
How to fill out Authorization For Use And Disclosure Of Protected Health Information Under HIPAA RULE 164.508?
US Legal Forms - one of the largest collections of legal documents in the United States - offers a range of legal form categories that you can download or print.
By using this website, you can access a vast array of forms for business and personal purposes, organized by categories, states, or keywords. You can find the latest versions of forms such as the Kentucky Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508 within seconds.
If you already have a monthly subscription, Log In to download the Kentucky Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508 from the US Legal Forms library. The Download button will appear on every form you view. You can access all previously downloaded forms in the My documents tab of your account.
Make modifications. Fill out, adjust, print, and sign the downloaded Kentucky Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508.
Each template you added to your account does not expire and is yours indefinitely. Therefore, if you wish to download or print another copy, simply navigate to the My documents section and click on the form you need. Access the Kentucky Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508 with US Legal Forms, the most extensive collection of legal document templates. Utilize numerous professional and state-specific templates that cater to your business or personal needs and requirements.
- If you would like to use US Legal Forms for the first time, follow these simple steps.
- Make sure you have selected the correct form for your city/state. Click the Review button to inspect the form's content. Check the form details to confirm you have chosen the appropriate form.
- If the form does not meet your requirements, utilize the Search box at the top of the screen to find one that does.
- If you are satisfied with the form, affirm your choice by clicking the Purchase now button. Then, select your preferred pricing plan and provide your credentials to register for an account.
- Complete the payment. Use a credit card or PayPal account to finalize the transaction.
- Select the format and download the form to your device.
Form popularity
FAQ
Individuals cannot receive HIPAA certification as it is not a formal credentialing process. However, you can take courses and training related to HIPAA compliance to better understand your responsibilities. While you cannot become 'HIPAA certified,' you can establish your knowledge and ensure that you handle the Kentucky Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508 accurately. The resources available on USLegalForms can guide you through this process.
HIPAA verification requires you to provide proof that your practices meet the HIPAA standards for privacy and security. This includes having a risk analysis, privacy policies, and employee training programs in place. For the Kentucky Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508, your organization must clearly document how it protects patient information. Using USLegalForms can simplify creating and maintaining the required documentation for your HIPAA verification.
To obtain HIPAA approval, you must ensure that your organization complies with the HIPAA regulations set forth by the U.S. Department of Health and Human Services. It is important to implement policies and procedures to protect patient information. Additionally, for the Kentucky Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508, your documentation must reflect compliance with these standards. USLegalForms offers a streamlined process to help you create and manage necessary legal documents.
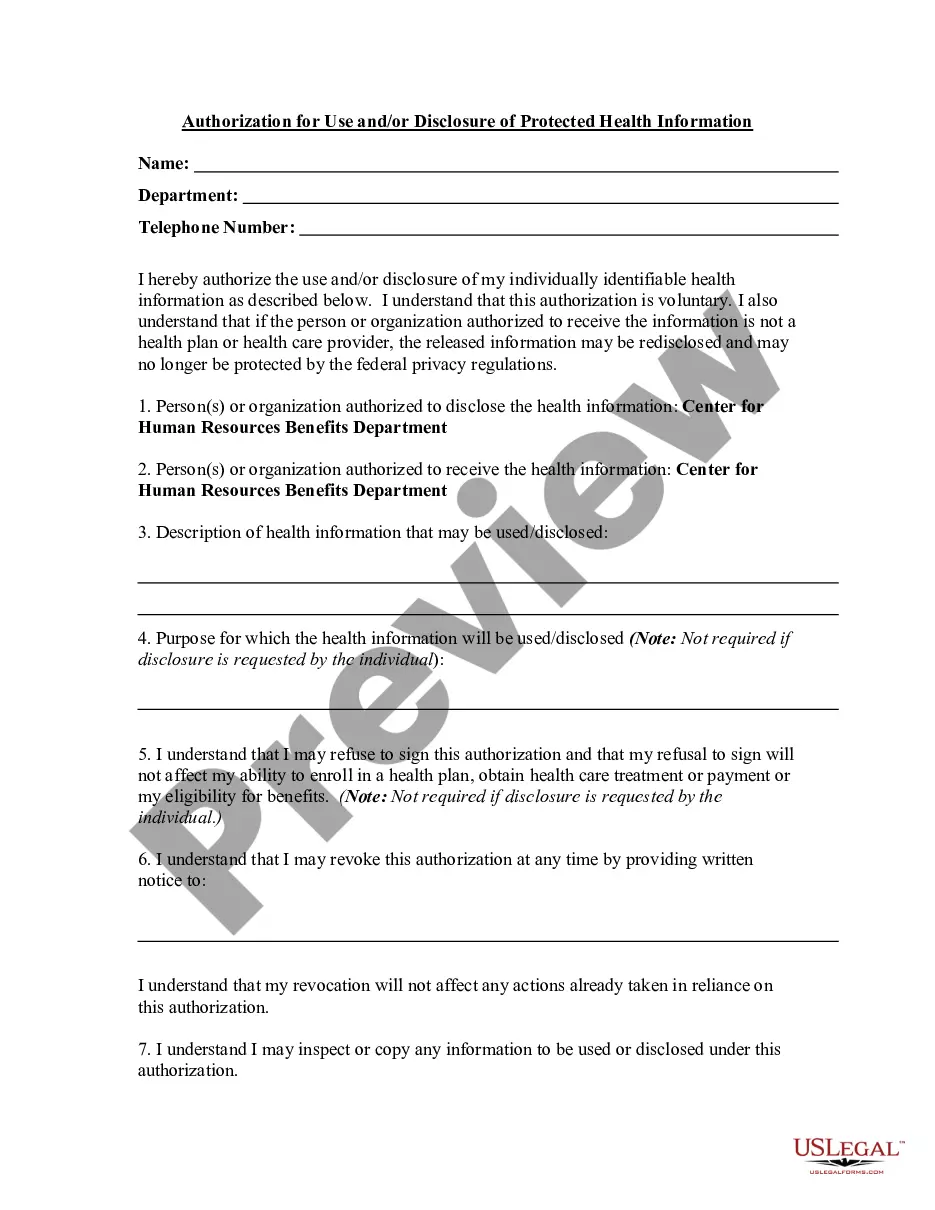
A HIPAA authorization is required to disclose protected health information when the disclosure is not related to treatment, payment, or healthcare operations. For example, if your healthcare provider wants to share your information for research or marketing purposes, they must obtain a Kentucky Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508. Utilizing services like uslegalforms can simplify this process for you by providing easy-to-use templates and guidance.
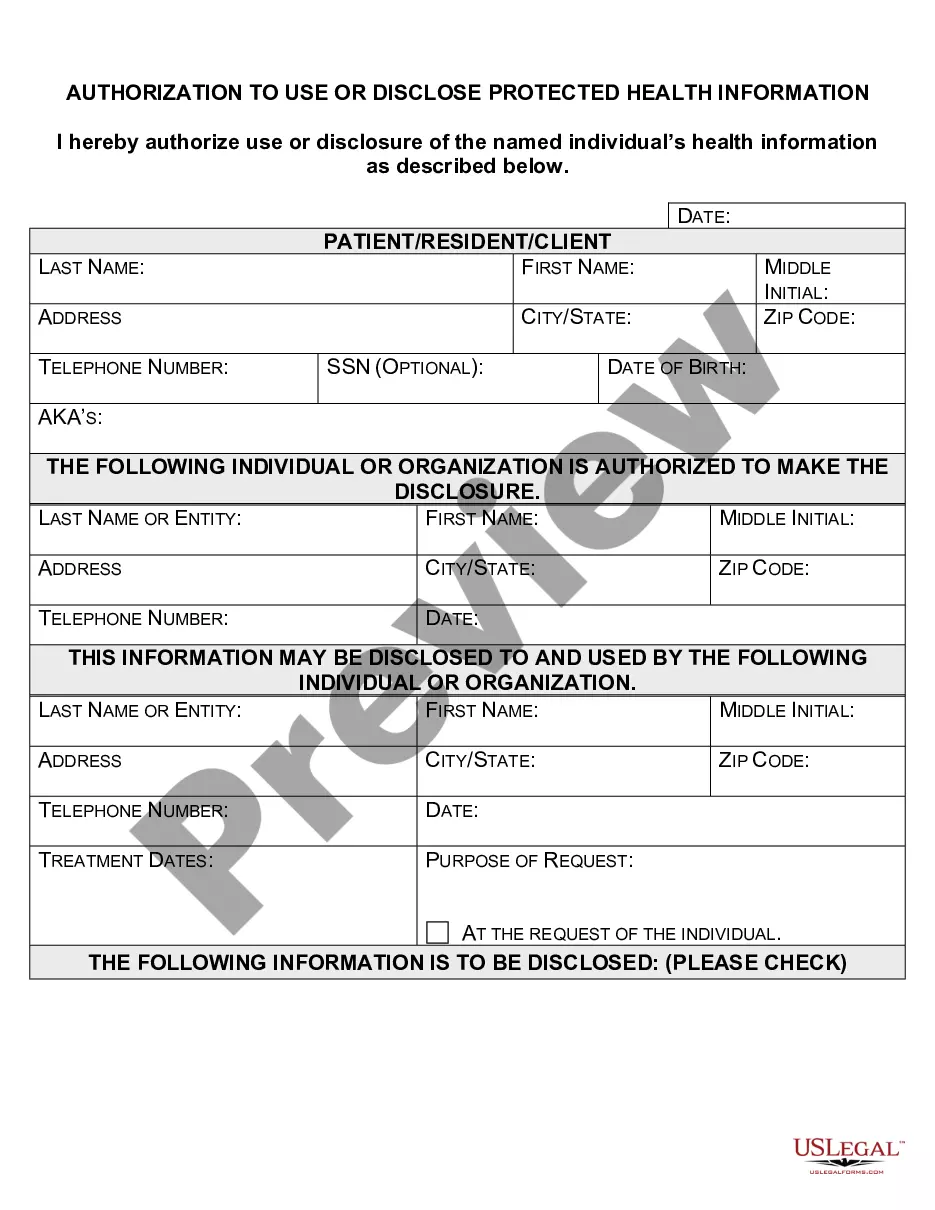
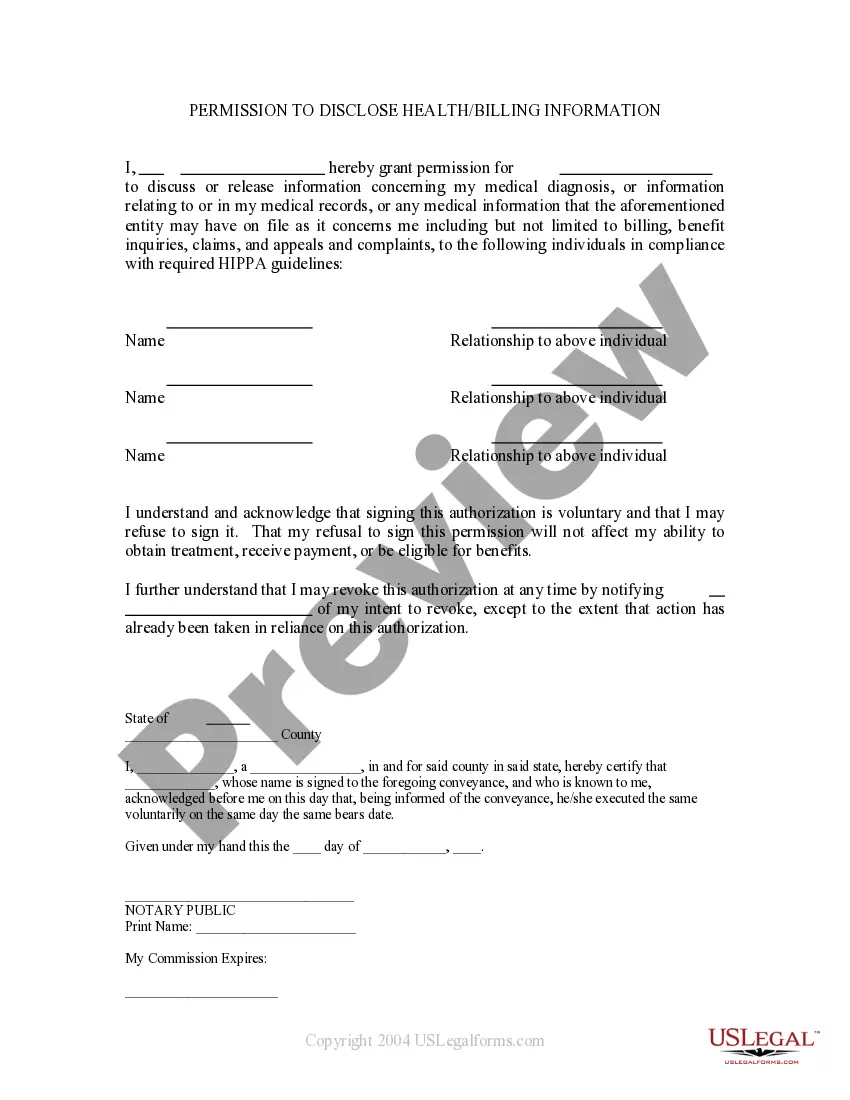
When HIPAA requires authorization to disclose information, the authorization must be written, and it should clearly identify the information being disclosed and the purpose of the disclosure. Additionally, it should specify who will receive the information. This process aligns with the Kentucky Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508, ensuring your rights are protected and your health information is handled responsibly.
A written authorization from a patient is essential when a healthcare provider needs to disclose the patient's Protected Health Information (PHI) for purposes other than treatment, payment, or healthcare operations. For instance, if you want to share your medical records with a third party for legal reasons or marketing, a Kentucky Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508 is necessary. This ensures that you maintain control over your sensitive information while complying with HIPAA regulations.
When HIPAA requires authorization to disclose information, the authorization must meet specific criteria outlined in the Kentucky Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508. This includes being written, signed by the individual, and describing the information that will be disclosed, the recipient, and the purpose of the disclosure. Compliance with these guidelines is essential for proper authorization.
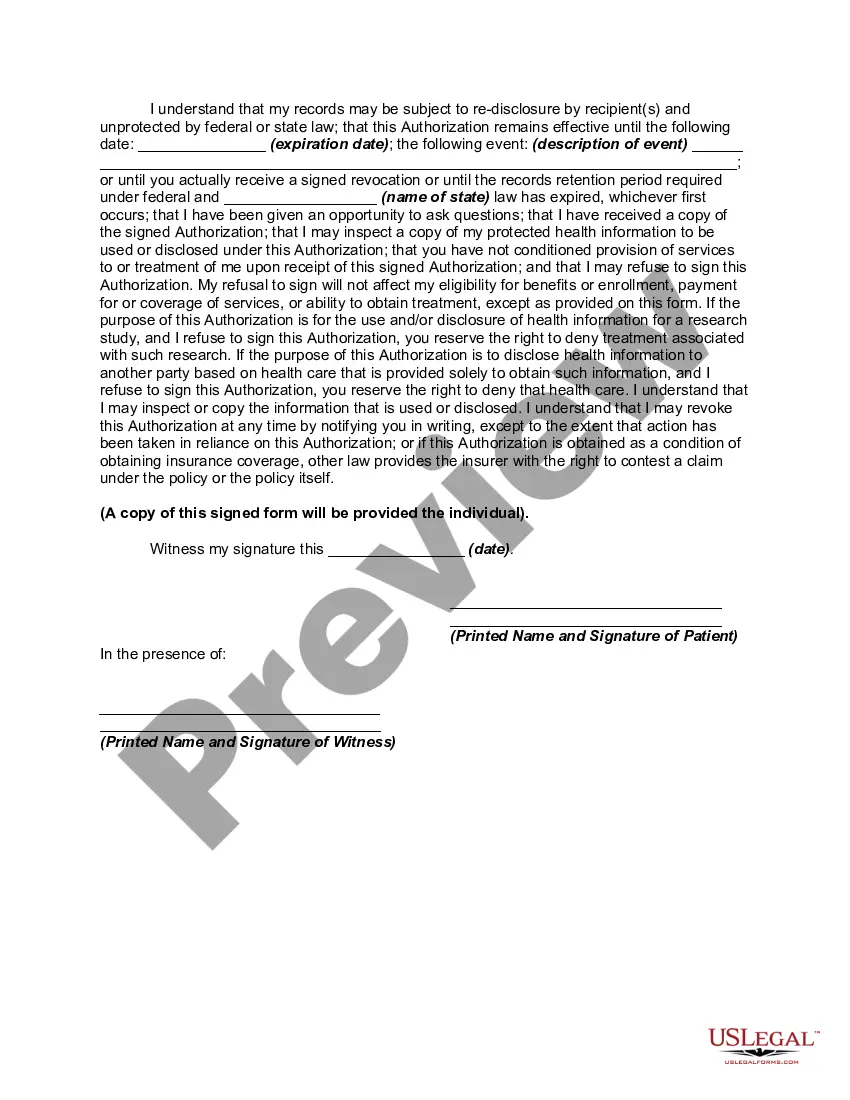
If you decline HIPAA authorization, the organization or individual requesting it cannot access your protected health information. This decision protects your privacy but may impact your ability to receive certain services or consultations. Understanding the implications of declining the Kentucky Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508 can help you manage your healthcare relationships.
HIPAA is generally considered beneficial as it sets standards for protecting patient information and promoting trust in healthcare systems. While it may create some barriers to information flow, these safeguards ensure that personal health data remains confidential. The Kentucky Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508 exemplifies how HIPAA supports patient rights.
Agreeing to HIPAA authorization is a personal choice that should consider the context of the request. If you trust the recipient and understand the purpose behind the authorization, it may be beneficial. Reviewing the Kentucky Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508 can help you feel more secure in your decision.