Indiana Summary of Rights and Obligations under COBRA
Description
How to fill out Summary Of Rights And Obligations Under COBRA?
Are you currently in a situation where you require documents for either professional or personal purposes almost all the time.
There are many legal document templates available online, but locating reliable ones is not easy.
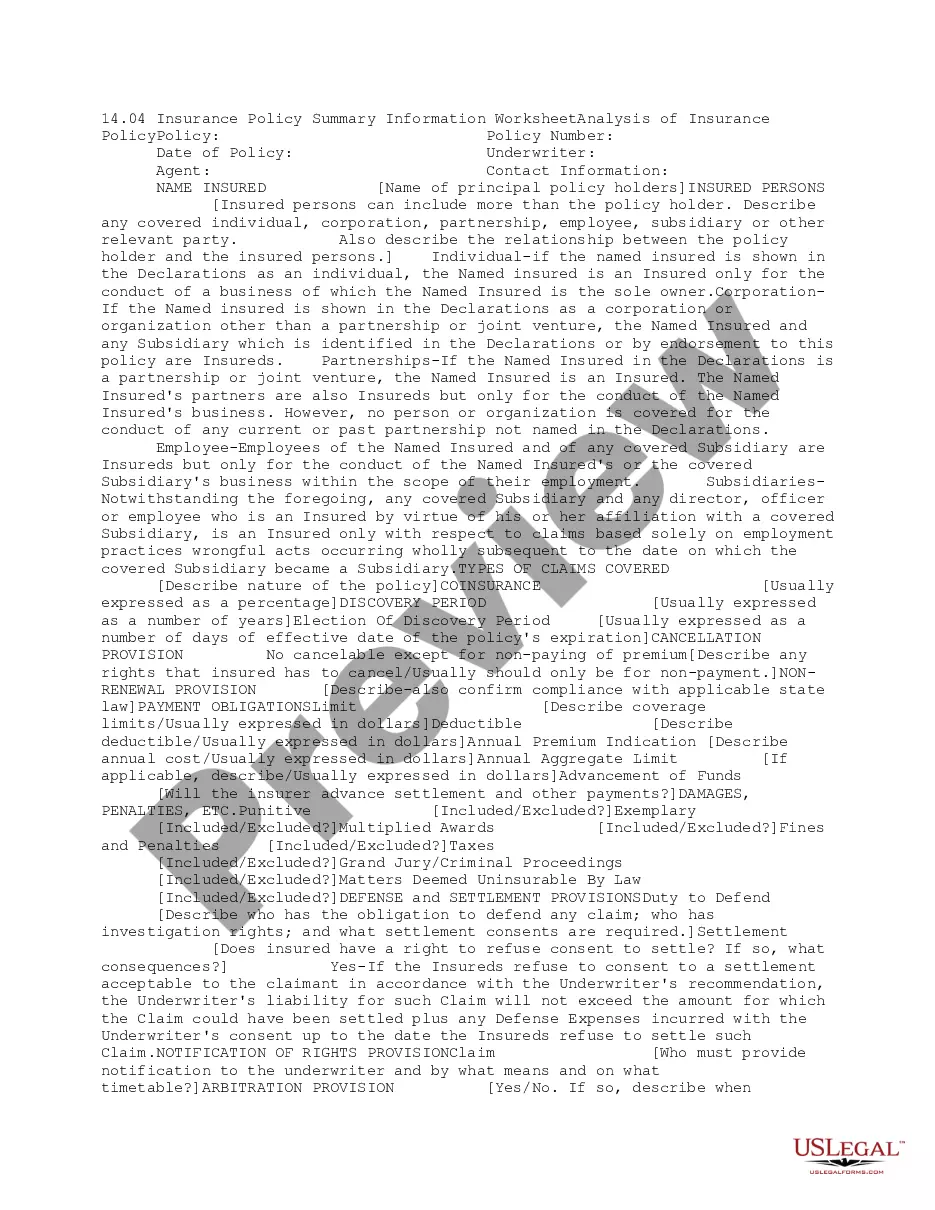
US Legal Forms offers a wide array of form templates, such as the Indiana Summary of Rights and Obligations under COBRA, which can be tailored to meet federal and state regulations.
Once you find the correct document, simply click Purchase now.
Select the payment plan you prefer, provide the necessary information to create your account, and complete your order using PayPal or a credit card.
- If you are currently familiar with the US Legal Forms website and have an account, simply Log In.
- Then, you can download the Indiana Summary of Rights and Obligations under COBRA template.
- If you do not have an account and wish to start using US Legal Forms, follow these steps.
- Find the document you need and ensure it is for the correct city or county.
- Utilize the Review button to look over the document.
- Check the information to confirm you have selected the right document.
- If the document is not what you're seeking, use the Research field to find the template that satisfies your needs and specifications.
Form popularity
FAQ
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
Q3: Which employers are required to offer COBRA coverage? COBRA generally applies to all private-sector group health plans maintained by employers that had at least 20 employees on more than 50 percent of its typical business days in the previous calendar year.
On Average, The Monthly COBRA Premium Cost Is $400 700 Per Person. Continuing on an employer's major medical health plan with COBRA is expensive.
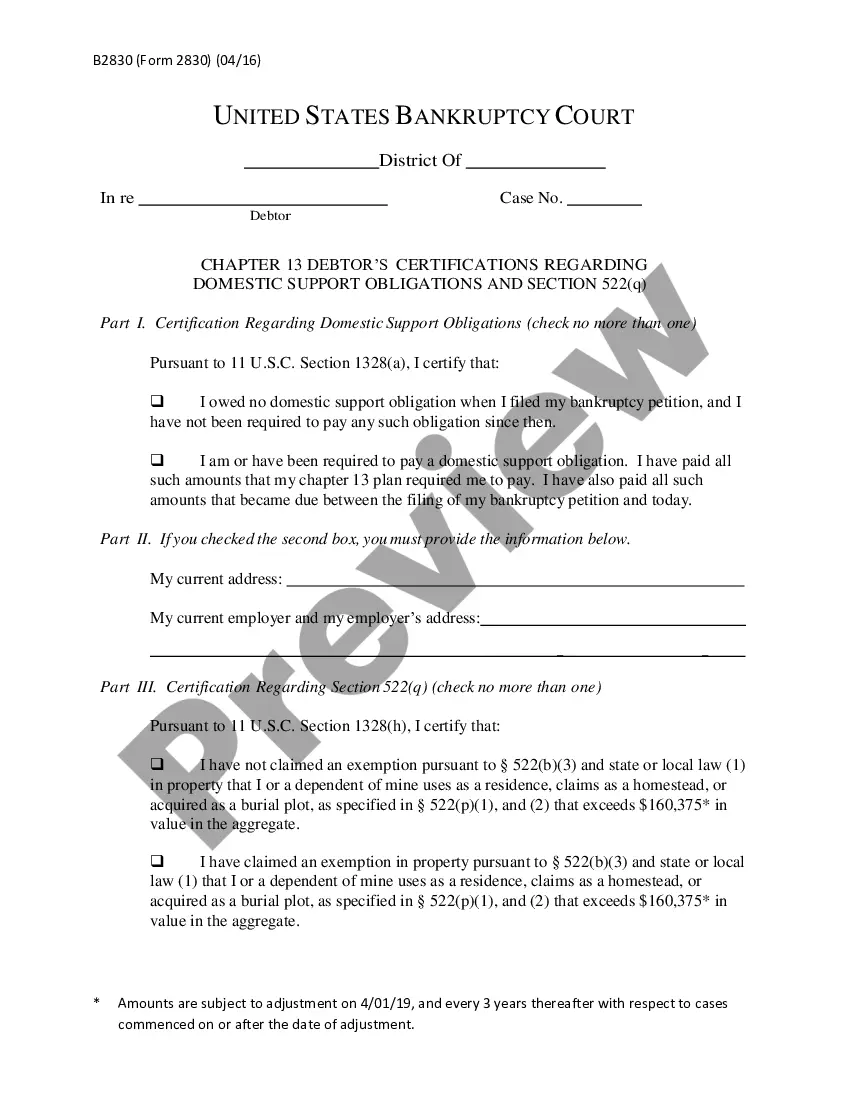
The Federal Consolidated Omnibus Budget Reconciliation Act (COBRA) requires the state of Indiana to offer covered employees and eligible family members the opportunity for a temporary extension of health coverage at group rates when coverage under the health plan would otherwise end.
COBRA is a federal law about health insurance. If you lose or leave your job, COBRA lets you keep your existing employer-based coverage for at least the next 18 months. Your existing healthcare plan will now cost you more. Under COBRA, you pay the whole premium including the share your former employer used to pay.
Who pays for COBRA coverage? The employee generally pays the full cost of the insurance premiums. In fact, the law allows the employer to charge 102 percent of the premium, and to keep the 2 percent to cover your administrative costs.
How long does it take for COBRA to kick in? With all paperwork properly submitted, your COBRA coverage should begin on the first day of your qualifying event (for example, the first day you are no longer with your employer), ensuring no gaps in your coverage.
Coverage with COBRA The COBRA plan offers health coverage to a terminated employee for a maximum of 18 months, sometimes less depending on how you qualify for the plan, and the family of an employee for up to 36 months, offering the same benefits as the initial group health care policy.
Coverage with COBRA The COBRA plan offers health coverage to a terminated employee for a maximum of 18 months, sometimes less depending on how you qualify for the plan, and the family of an employee for up to 36 months, offering the same benefits as the initial group health care policy.
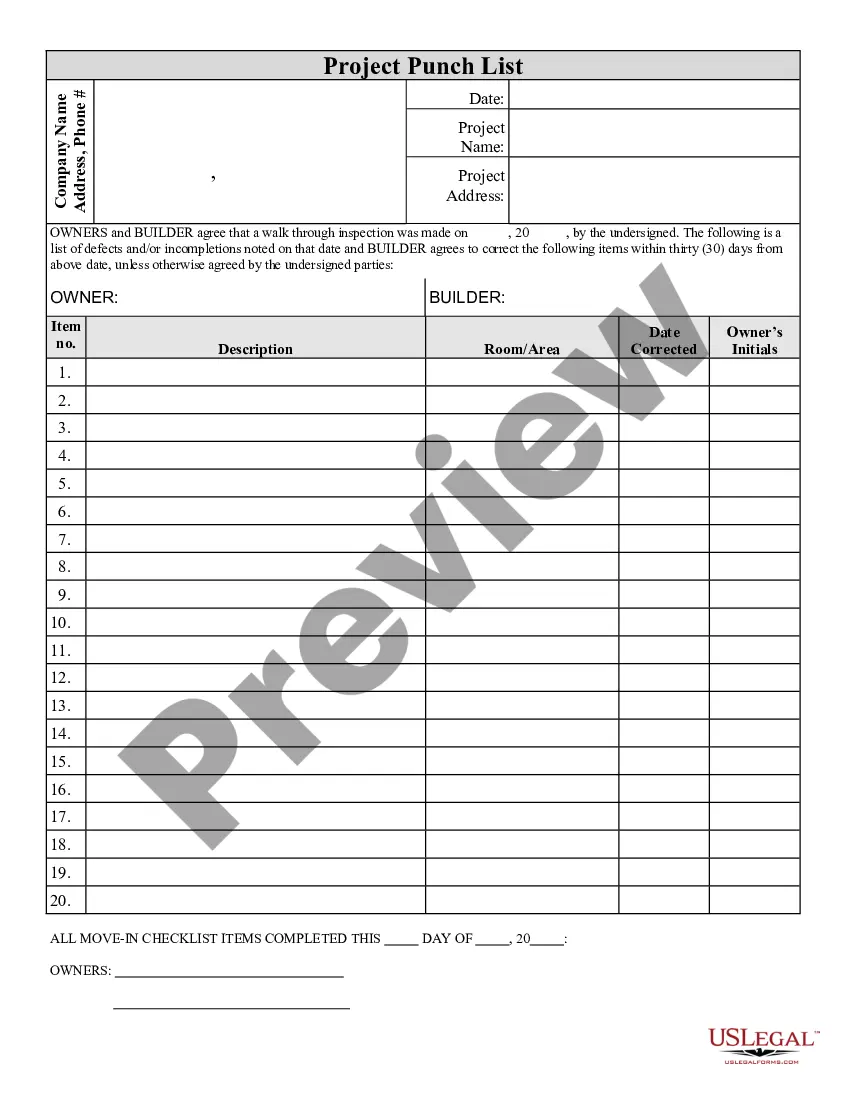
As an employer, you are responsible for notifying your former employee of the right to elect COBRA continuing health care coverage under your group plan. Most employers will include COBRA coverage information in the business employee handbook and as part of an employee's exit paperwork.