Indiana Introductory COBRA Letter
Description
How to fill out Introductory COBRA Letter?
Are you in a scenario where you require documents for either business or personal reasons constantly.
There are numerous legal document templates available online, but finding reliable ones is not easy.
US Legal Forms offers thousands of template documents, including the Indiana Introductory COBRA Letter, designed to fulfill federal and state requirements.
Once you find the appropriate form, click Purchase now.
Choose the payment plan you want, provide the necessary information to create your account, and purchase your order using your PayPal or Visa or MasterCard.
- If you are already familiar with the US Legal Forms website and have an account, simply Log In.
- Then you can download the Indiana Introductory COBRA Letter template.
- If you do not have an account and wish to start using US Legal Forms, follow these steps.
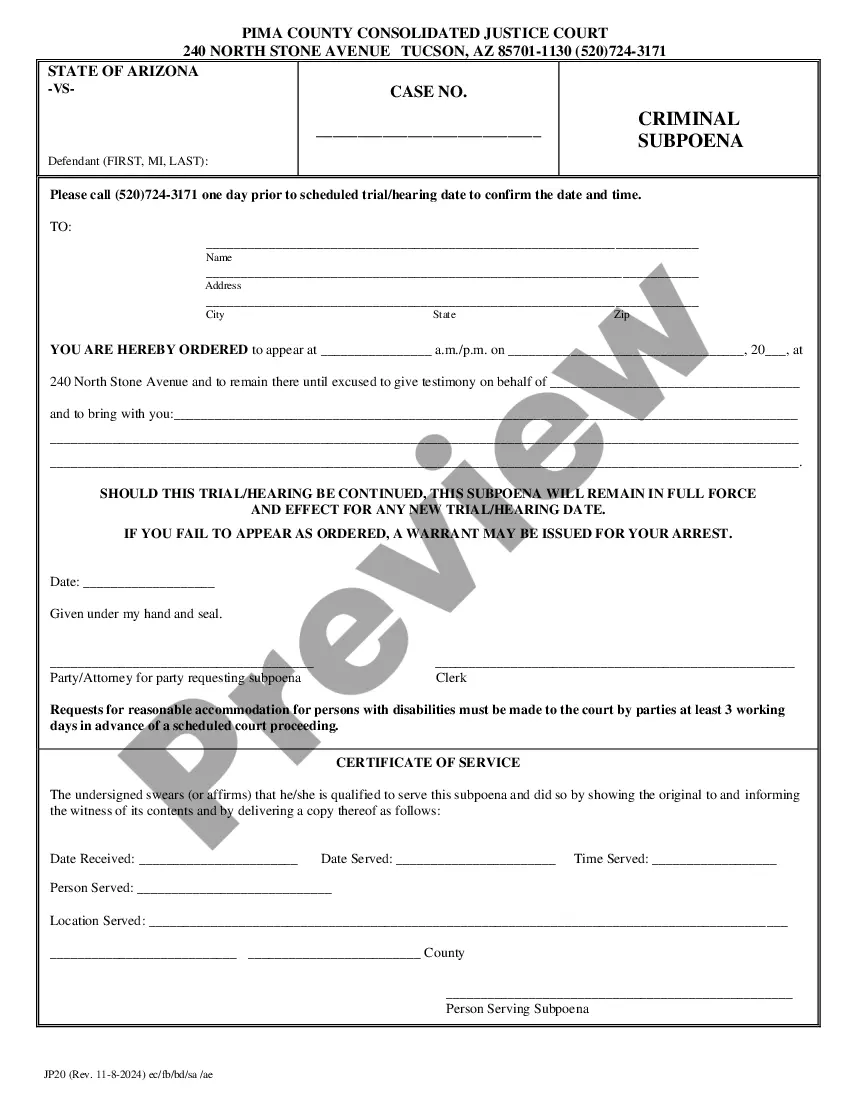
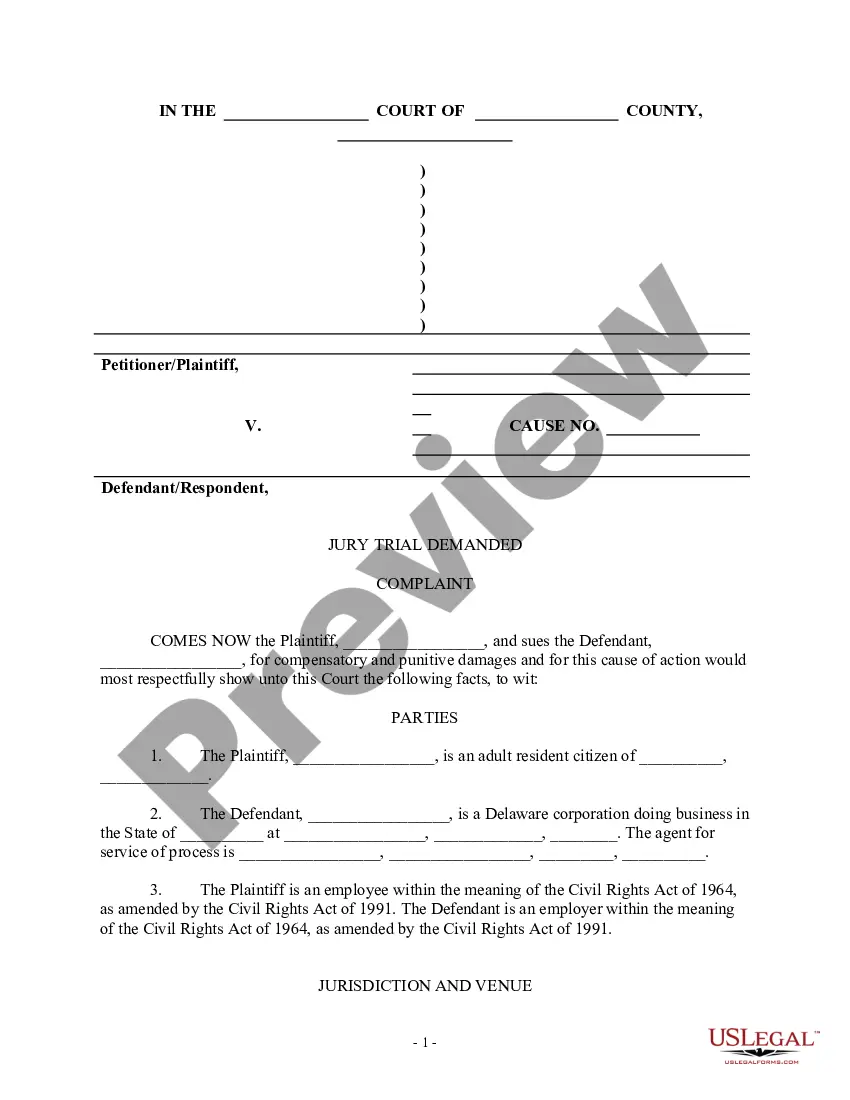
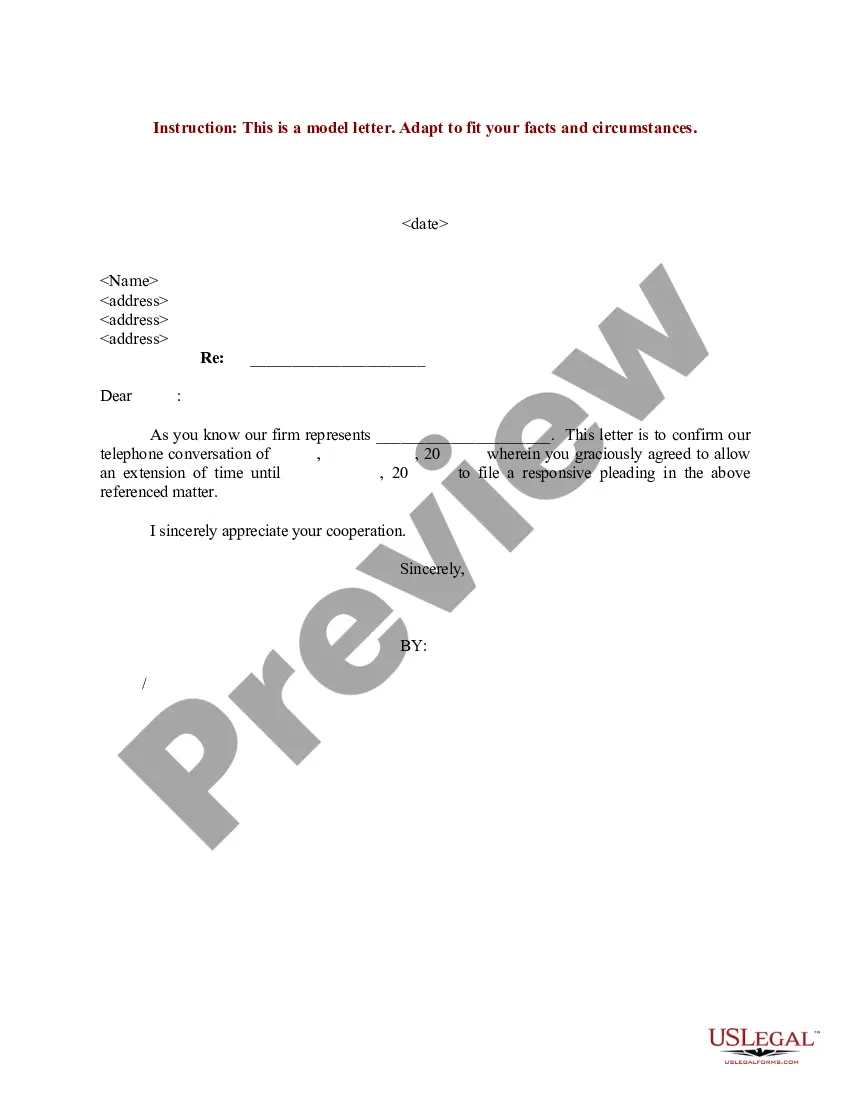
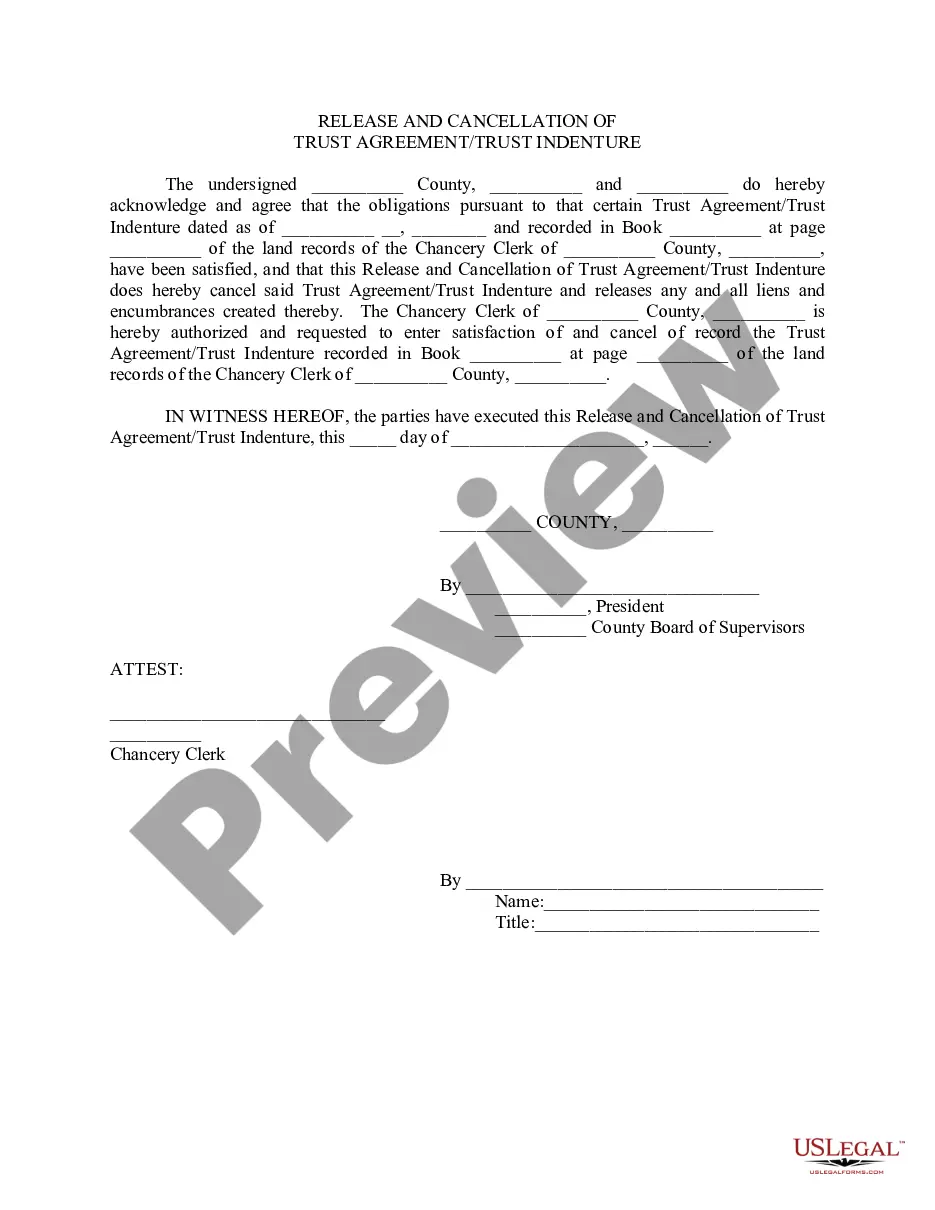
- Select the document you need and ensure it is for your correct location.
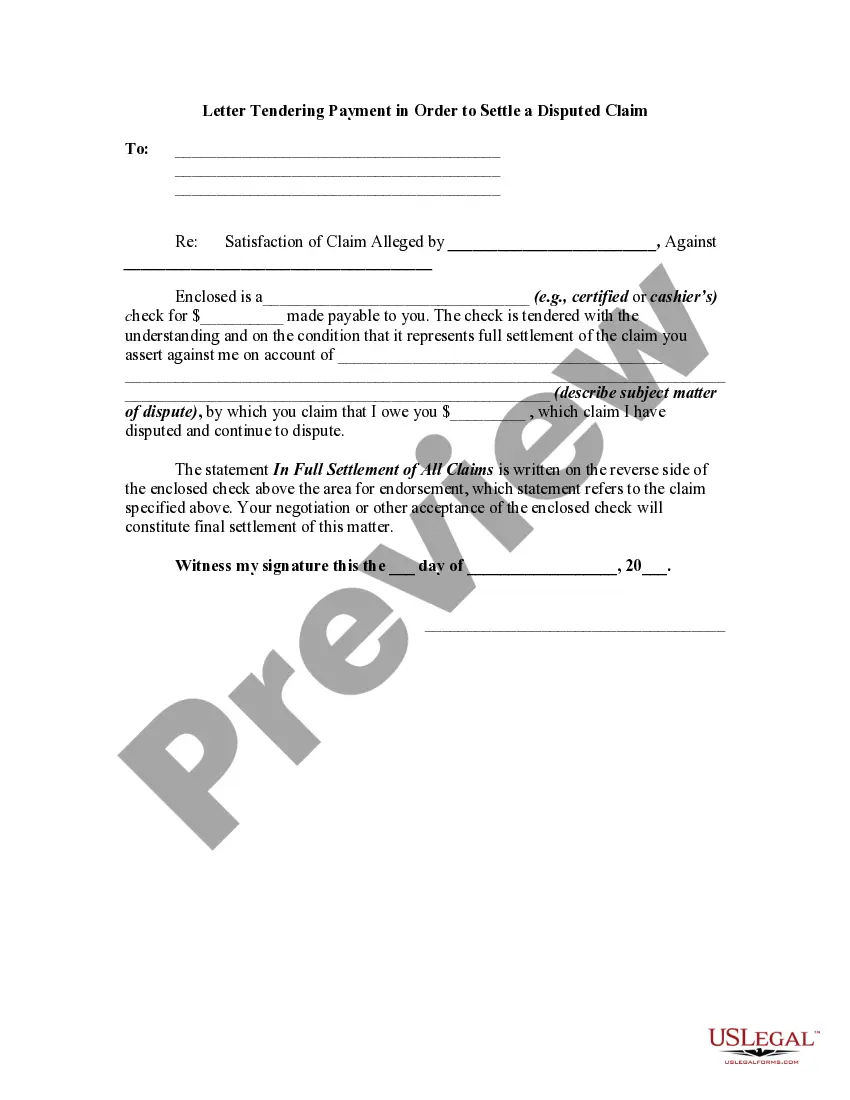
- Use the Preview button to review the form.
- Check the description to confirm you have chosen the right template.
- If the form is not what you are looking for, use the Search field to find a template that meets your needs.
Form popularity
FAQ
COBRA is a federal law about health insurance. If you lose or leave your job, COBRA lets you keep your existing employer-based coverage for at least the next 18 months. Your existing healthcare plan will now cost you more. Under COBRA, you pay the whole premium including the share your former employer used to pay.
If You Do Not Receive Your COBRA PaperworkReach out to the Human Resources Department and ask for the COBRA Administrator. They may use a third-party administrator to handle your enrollment. If the employer still does not comply you can call the Department of Labor at 1-866-487-2365.
The initial notice, also referred to as the general notice, communicates general COBRA rights and obligations to each covered employee (and his or her spouse) who becomes covered under the group health plan.
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
Your employer must mail you the COBRA information and forms within 14 days after receiving notification of the qualifying event. You are responsible for making sure your COBRA coverage goes into and stays in effect - if you do not ask for COBRA coverage before the deadline, you may lose your right to COBRA coverage.
Coverage with COBRA The COBRA plan offers health coverage to a terminated employee for a maximum of 18 months, sometimes less depending on how you qualify for the plan, and the family of an employee for up to 36 months, offering the same benefits as the initial group health care policy.
Coverage with COBRA The COBRA plan offers health coverage to a terminated employee for a maximum of 18 months, sometimes less depending on how you qualify for the plan, and the family of an employee for up to 36 months, offering the same benefits as the initial group health care policy.
The Federal Consolidated Omnibus Budget Reconciliation Act (COBRA) requires the state of Indiana to offer covered employees and eligible family members the opportunity for a temporary extension of health coverage at group rates when coverage under the health plan would otherwise end.
These state laws are the mini-COBRA laws. According to the National Conference of State Legislatures, 40 states and the District of Columbia have some sort of mini-COBRA law. (Alabama, Alaska, Arizona, Delaware, Idaho, Indiana, Michigan, Montana, Pennsylvania and Washington had no such laws as of May 2009.)
You should get a notice in the mail about your COBRA and Cal-COBRA rights. You have 60 days after being notified to sign up. If you are eligible for Federal COBRA and did not get a notice, contact your employer. If you are eligible for Cal-COBRA and did not get a notice, contact your health plan.