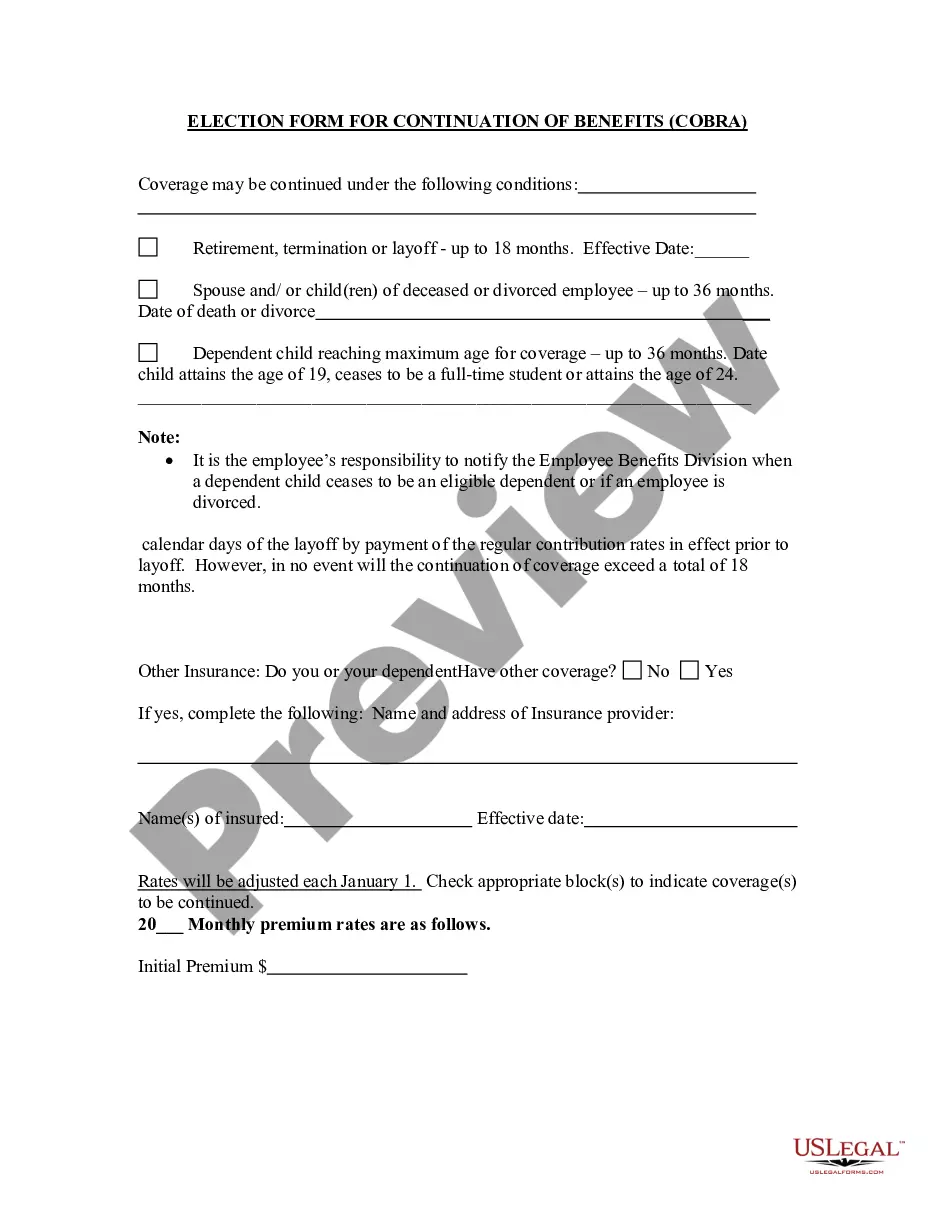
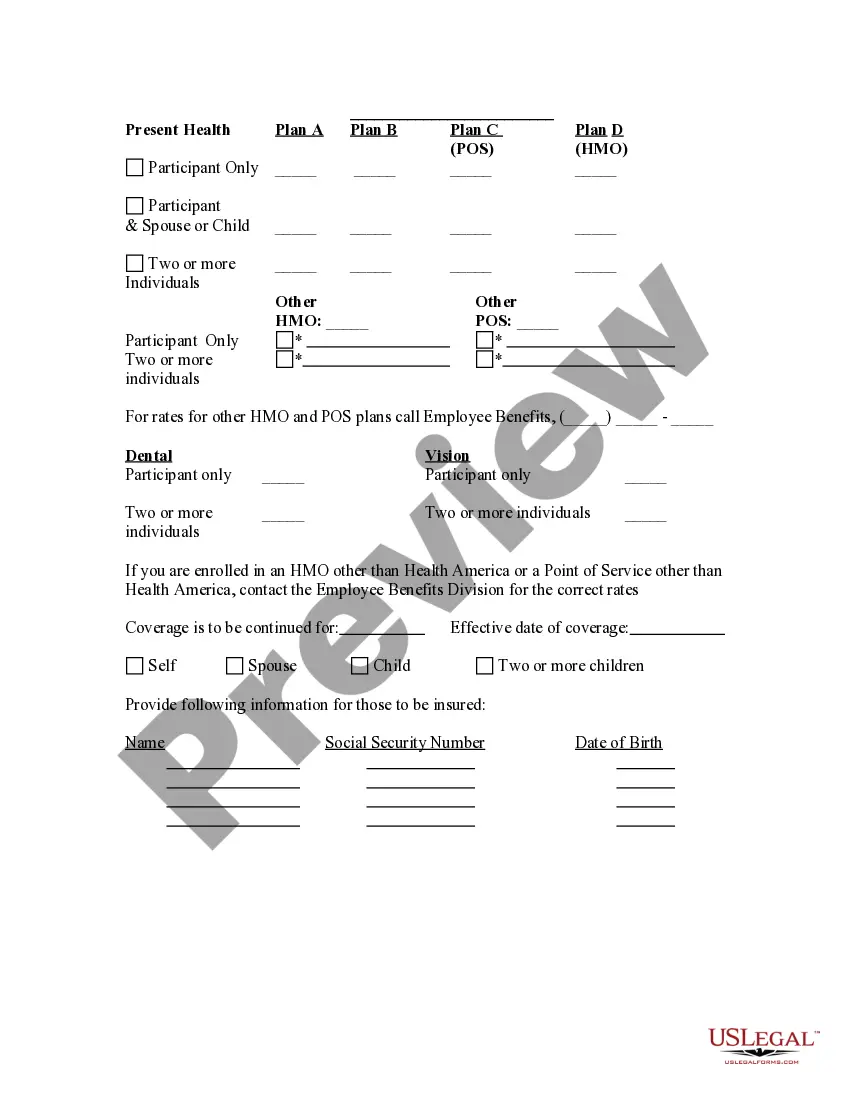
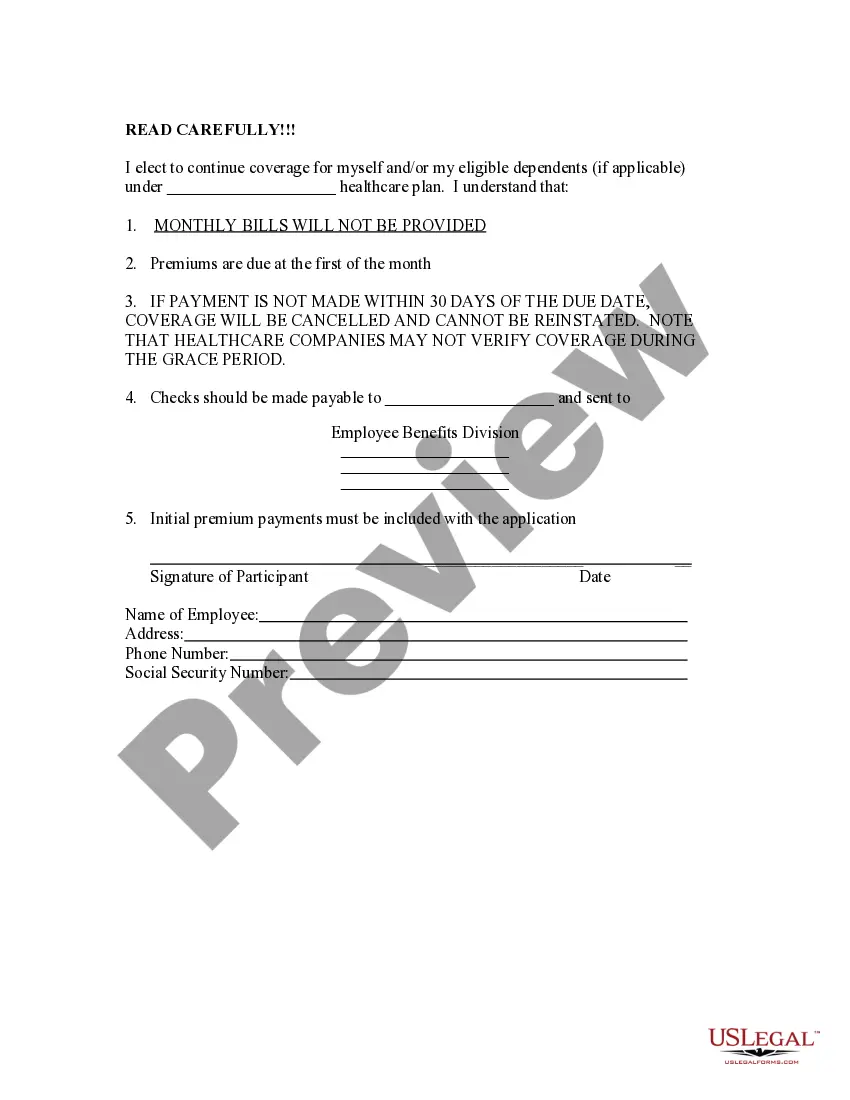
Illinois Election Form for Continuation of Benefits - COBRA
Description
How to fill out Election Form For Continuation Of Benefits - COBRA?
If you want to be thorough, obtain, or print official document templates, utilize US Legal Forms, the largest assortment of legal forms available online.
Use the site’s simple and user-friendly search feature to find the documents you need.
A variety of templates for business and personal purposes are organized by category and state, or keywords.
Step 4. Once you have located the form you need, click the Get now button. Select the pricing plan you desire and enter your details to register for an account.
Step 5. Complete the transaction. You can use your credit card or PayPal account to finalize the transaction. Step 6. Choose the format of the legal form and download it to your device. Step 7. Fill it out, modify, and print or sign the Illinois Election Form for Continuation of Benefits - COBRA. Each official document template you acquire is yours permanently. You will have access to every form you saved in your account. Click the My documents section and pick a form to print or download again. Stay efficient and download and print the Illinois Election Form for Continuation of Benefits - COBRA with US Legal Forms. There are millions of professional and state-specific forms available for your business or personal requirements.
- Utilize US Legal Forms to find the Illinois Election Form for Continuation of Benefits - COBRA in just a few clicks.
- If you are currently a US Legal Forms user, Log In to your account and click the Download button to obtain the Illinois Election Form for Continuation of Benefits - COBRA.
- You can also access forms you previously saved in the My documents section of your account.
- If you are using US Legal Forms for the first time, follow the steps below.
- Step 1. Make sure you have selected the form for your appropriate city/state.
- Step 2. Use the Preview option to review the form’s contents. Don’t forget to read the description.
- Step 3. If you are not satisfied with the form, use the Search field at the top of the screen to find alternative templates in the legal form directory.
Form popularity
FAQ
COBRA continuation coverage lets you stay on your employer's group health insurance plan after leaving your job. COBRA stands for the Consolidated Omnibus Budget Reconciliation Act. It's shorthand for the law change that required employers to extend temporary group health insurance to departing employees.
The general notice describes general COBRA rights and employee obligations. This notice must be provided to each covered employee and each covered spouse of an employee who becomes covered under the plan. The notice must be provided within the first 90 days of coverage under the group health plan.
Cal-COBRA is a California Law that lets you keep your group health plan when your job ends or your hours are cut. It may also be available to people who have exhausted their Federal COBRA.
COBRA the Consolidated Omnibus Budget Reconciliation Act -- requires group health plans to offer continuation coverage to covered employees, former employees, spouses, former spouses, and dependent children when group health coverage would otherwise be lost due to certain events.
Qualified beneficiaries must be given an election period of at least 60 days during which each qualified beneficiary may choose whether to elect COBRA coverage. This period is measured from the later of the date of the qualifying event or the date the COBRA election notice is provided.
Federal law requires that most group health plans (including this Plan) give employees and their families the opportunity to continue their health care coverage through COBRA continuation coverage when there's a qualifying event that would result in a loss of coverage under an employer's plan.
Illinois Continuation (mini-COBRA) must be offered to you and your eligible dependents who were continuously covered under the group policy for three months prior to termination of employment or reduction in hours below the minimum required by the group plan.
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.