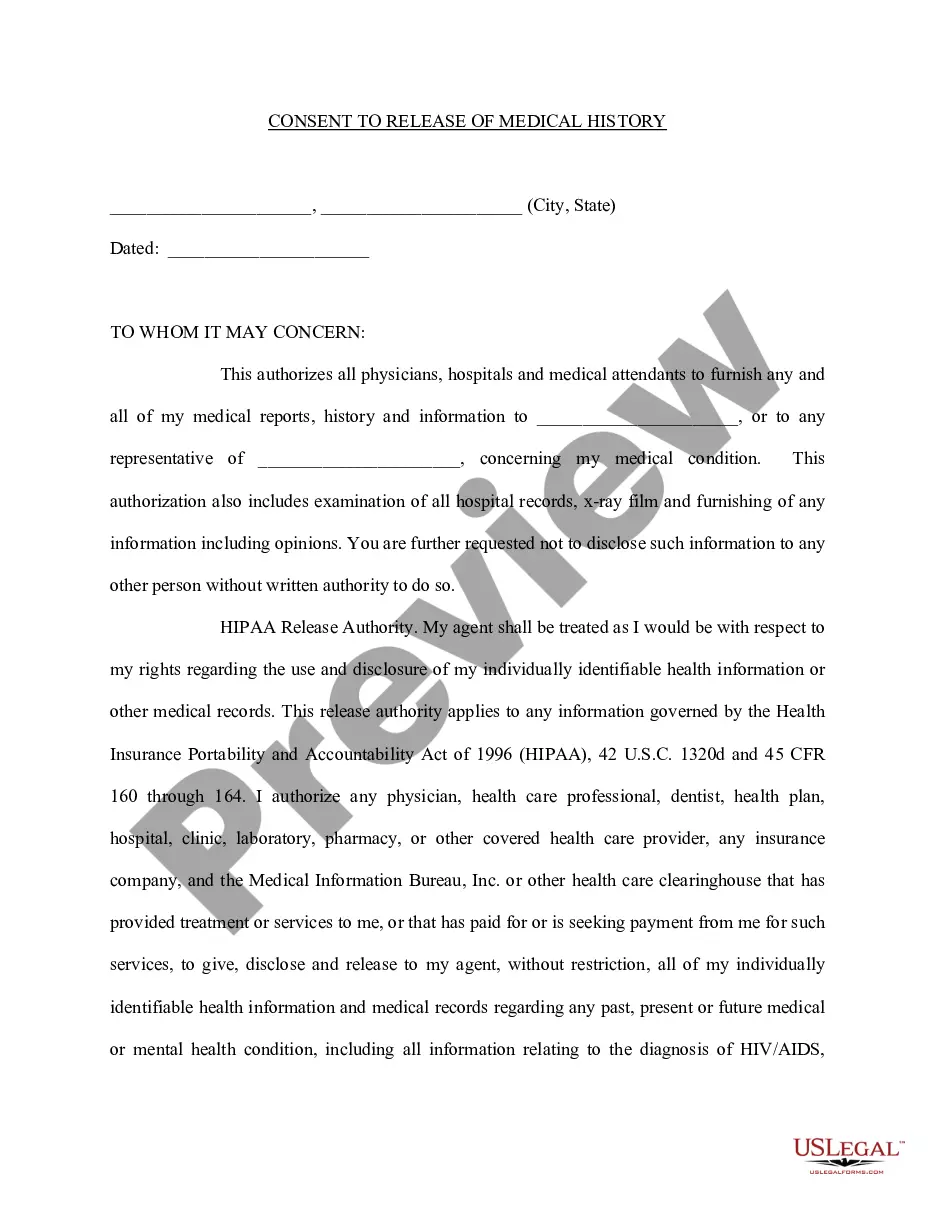
Hawaii Permission To Disclose Health Billing Information
Description
How to fill out Permission To Disclose Health Billing Information?
You are able to spend several hours on-line searching for the lawful papers format that fits the state and federal demands you require. US Legal Forms provides thousands of lawful varieties that happen to be reviewed by pros. It is possible to down load or produce the Hawaii Permission To Disclose Health Billing Information from our service.
If you currently have a US Legal Forms accounts, you can log in and click on the Download key. After that, you can complete, change, produce, or indication the Hawaii Permission To Disclose Health Billing Information. Every lawful papers format you acquire is your own property forever. To get an additional copy of any purchased kind, check out the My Forms tab and click on the related key.
If you are using the US Legal Forms internet site the very first time, adhere to the straightforward recommendations listed below:
- Initially, make certain you have selected the best papers format for the region/town that you pick. Look at the kind explanation to make sure you have chosen the appropriate kind. If accessible, make use of the Preview key to search with the papers format as well.
- If you want to discover an additional version in the kind, make use of the Search field to discover the format that meets your requirements and demands.
- When you have identified the format you would like, just click Get now to move forward.
- Find the pricing plan you would like, key in your qualifications, and sign up for an account on US Legal Forms.
- Total the deal. You may use your Visa or Mastercard or PayPal accounts to cover the lawful kind.
- Find the format in the papers and down load it to your system.
- Make changes to your papers if required. You are able to complete, change and indication and produce Hawaii Permission To Disclose Health Billing Information.
Download and produce thousands of papers themes using the US Legal Forms website, which provides the most important variety of lawful varieties. Use specialist and condition-particular themes to tackle your company or specific requirements.
Form popularity
FAQ
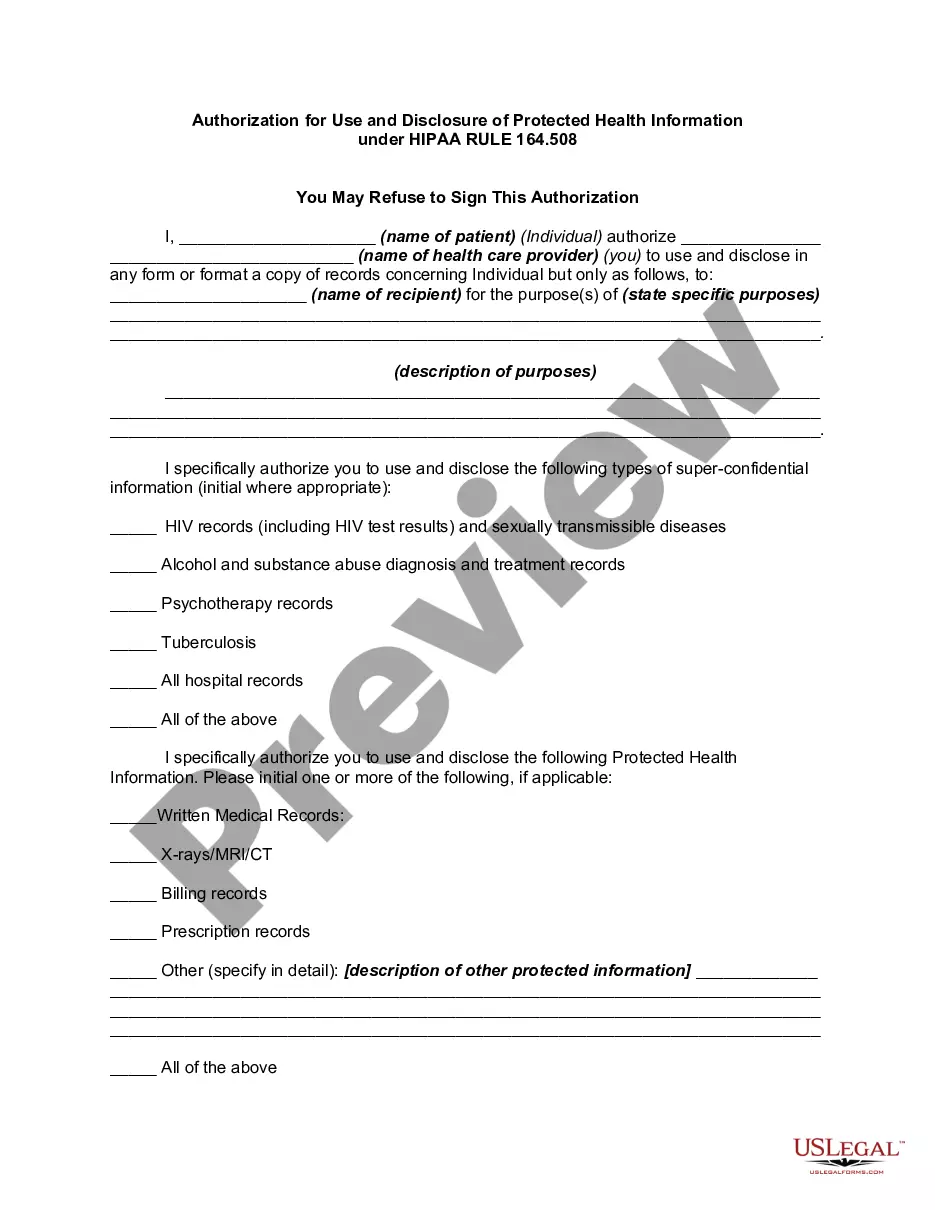
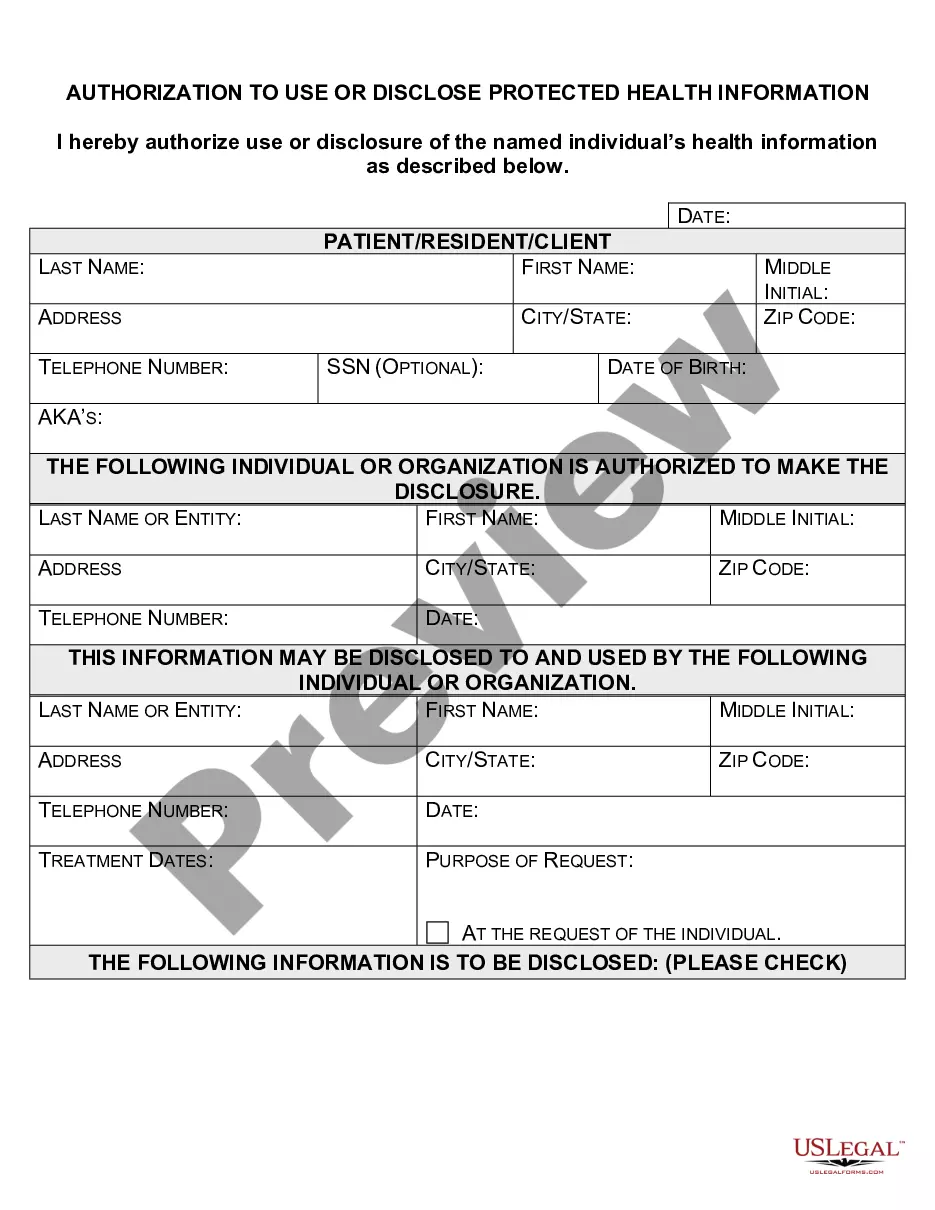
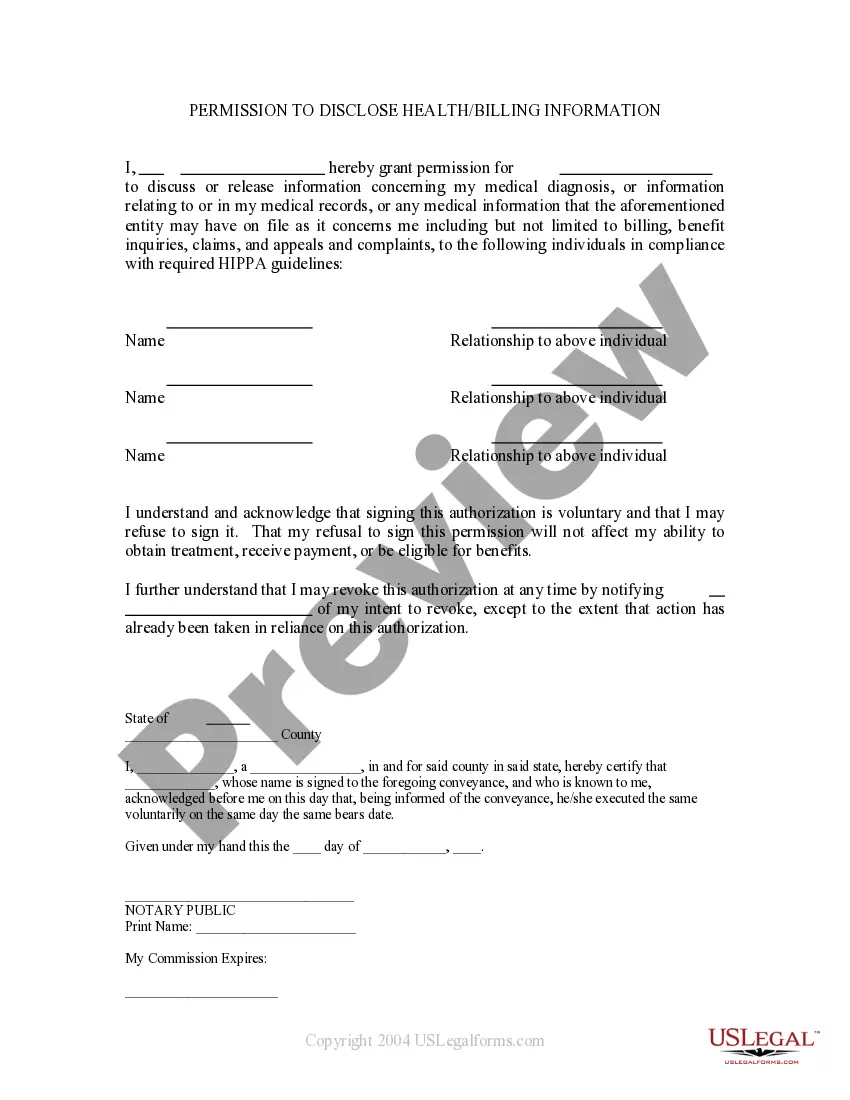
To fill out the authorization to use and disclose health information, start by gathering all necessary personal details, including your name, address, and contact information. Next, specify the type of health information you wish to share, clearly indicating the purpose of the disclosure. Make sure to sign and date the form to validate your request. For a seamless experience, consider using US Legal Forms, which provides templates specifically designed for obtaining Hawaii Permission To Disclose Health Billing Information.
HIPAA does not regulate credit reporting of medical bills. The FCRA does. And the FCRA does not allow deletion of reported debt even in the case of a HIPAA violation. But the creditor may be willing to delete the reporting if you threaten to sue them for violating the law.
One of the most readily felt impacts of HIPAA is the standardization of medical codes used by coders and billers. As we discussed in the last Course, HIPAA formalized the use of ICD codes for diagnosis and CPT and HCPCS codes for procedural reporting. We use these codes every day in medical billing to create claims.
Covered entities may disclose protected health information that they believe is necessary to prevent or lessen a serious and imminent threat to a person or the public, when such disclosure is made to someone they believe can prevent or lessen the threat (including the target of the threat).
HIPAA violation. HIPAA violations involving patient billing and other financial communications happen every day. Patient financial correspondence is absolutely protected health information (PHI) under HIPAA because it contains health information linked to individual identifiers.
An authorization is a detailed document that gives covered entities permission to use protected health information for specified purposes, which are generally other than treatment, payment, or health care operations, or to disclose protected health information to a third party specified by the individual.
Under the HIPAA Privacy Rule, a covered entity must disclose protected health information in only two situations: (a) to individuals (or their personal representatives) specifically when they request access to, or an accounting of disclosures of, their protected health information; and (b) to the Department of Health
Title II of HIPAA applies directly to medical billing companies, as it dictates the proper uses and disclosures of protected health information (PHI), as well as simplifying processing of claims and billing.
In other words, PHI is personally identifiable information in medical records, including conversations between doctors and nurses about treatment. PHI also includes billing information and any patient-identifiable information in a health insurance company's computer system.
Protected health information (PHI), also referred to as personal health information, is the demographic information, medical histories, test and laboratory results, mental health conditions, insurance information and other data that a healthcare professional collects to identify an individual and determine appropriate