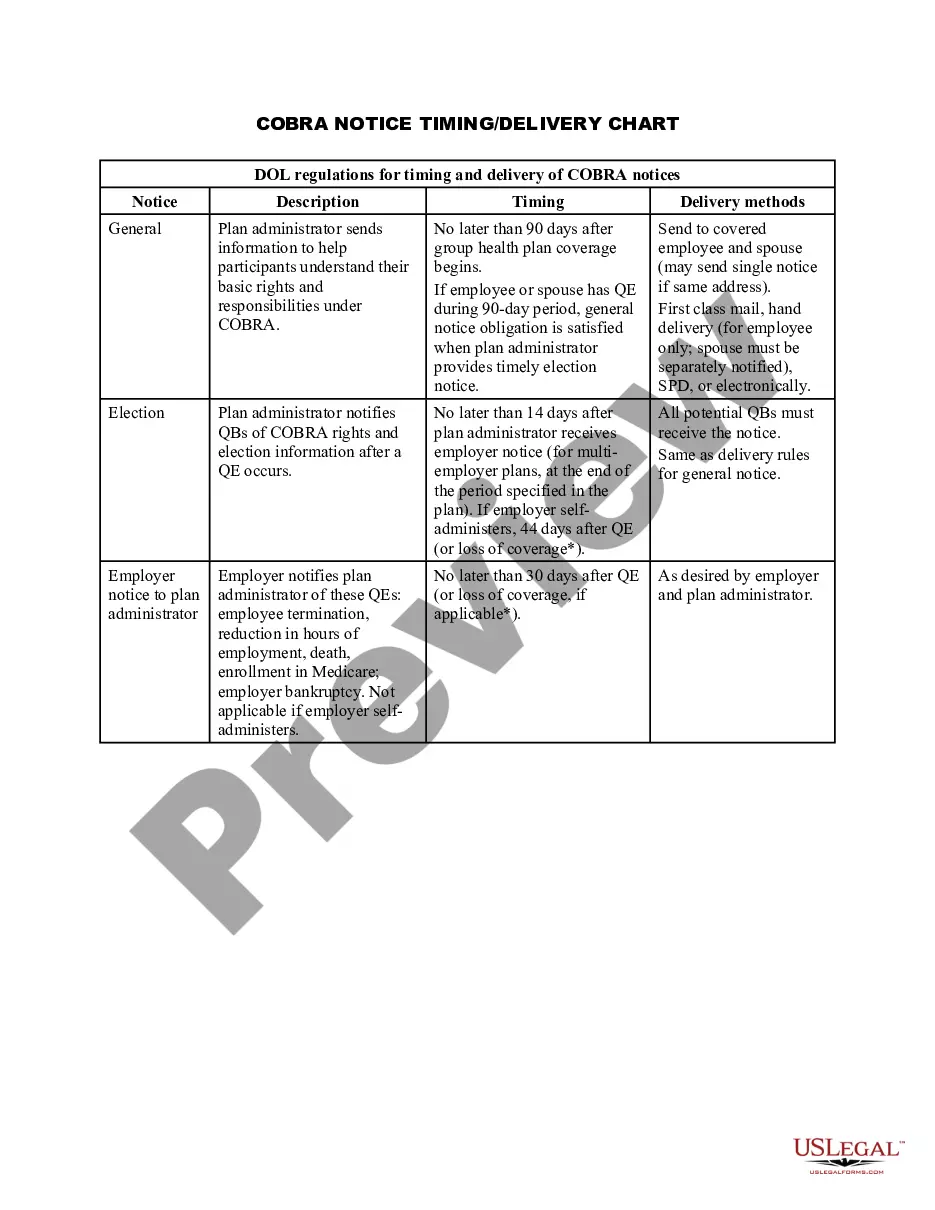
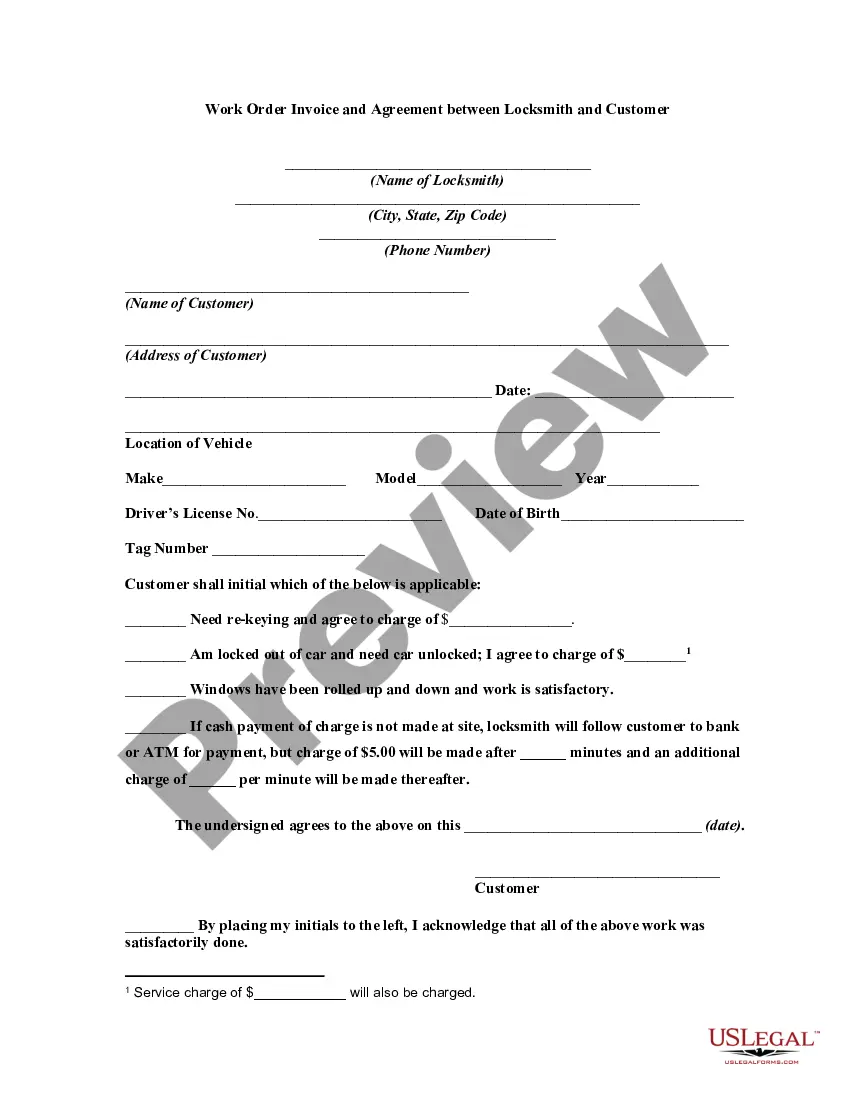
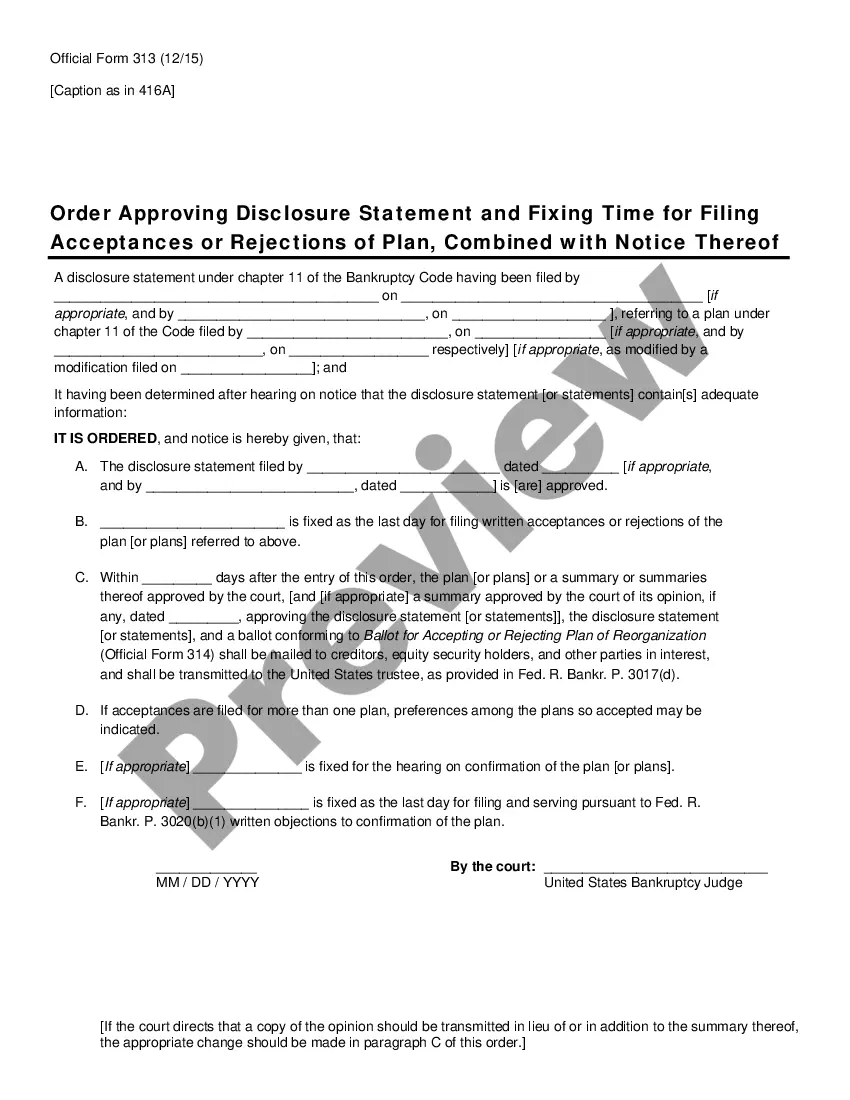
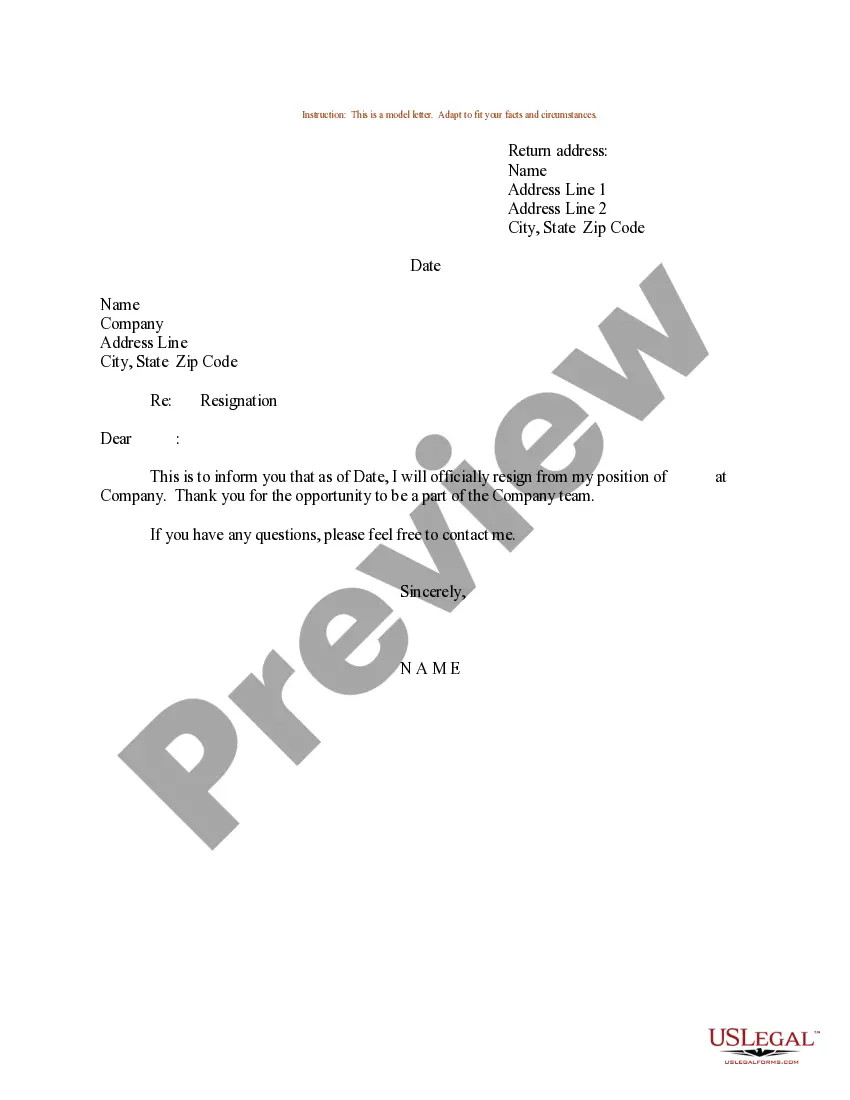
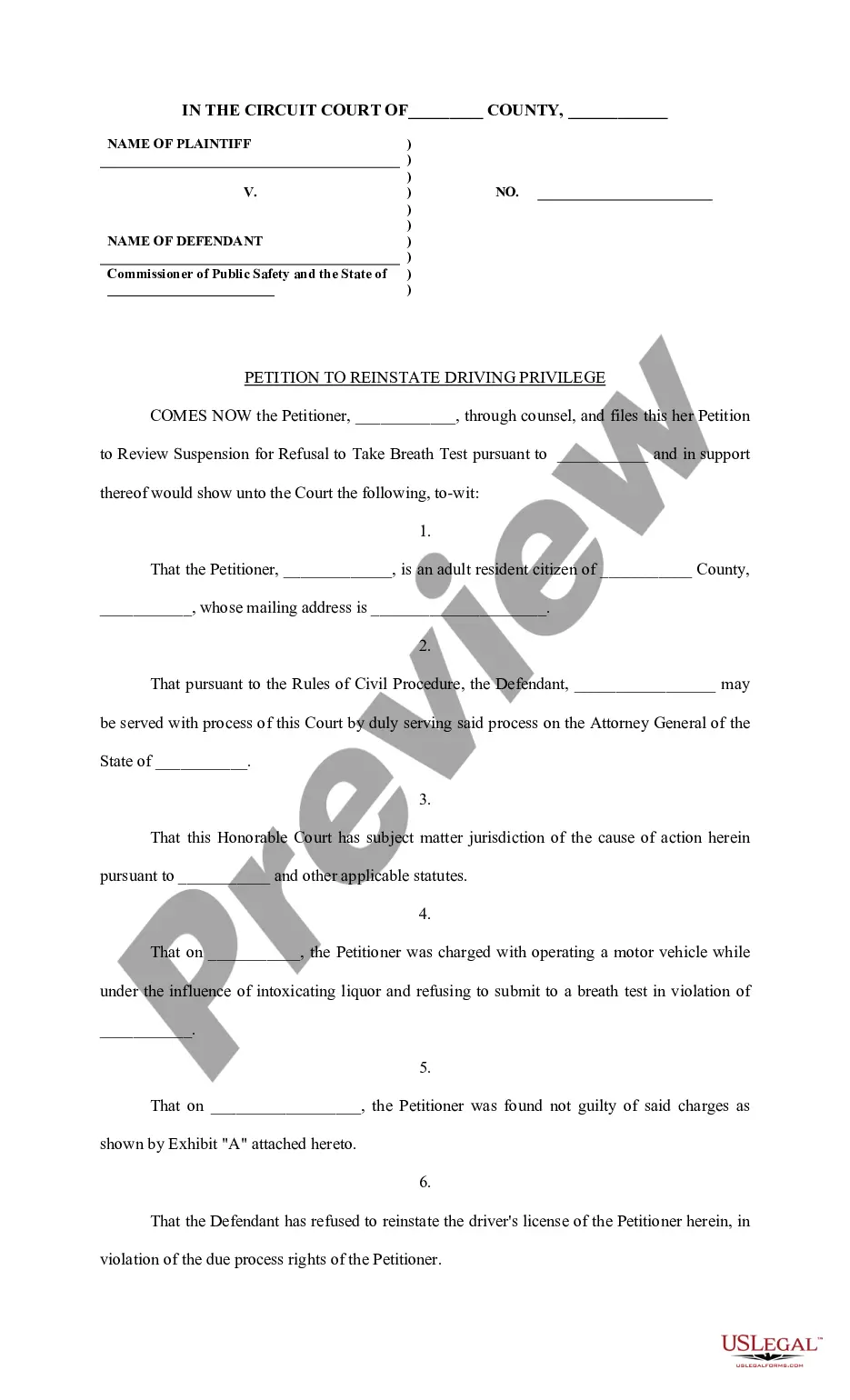
Guam COBRA Notice Timing Delivery Chart
Description
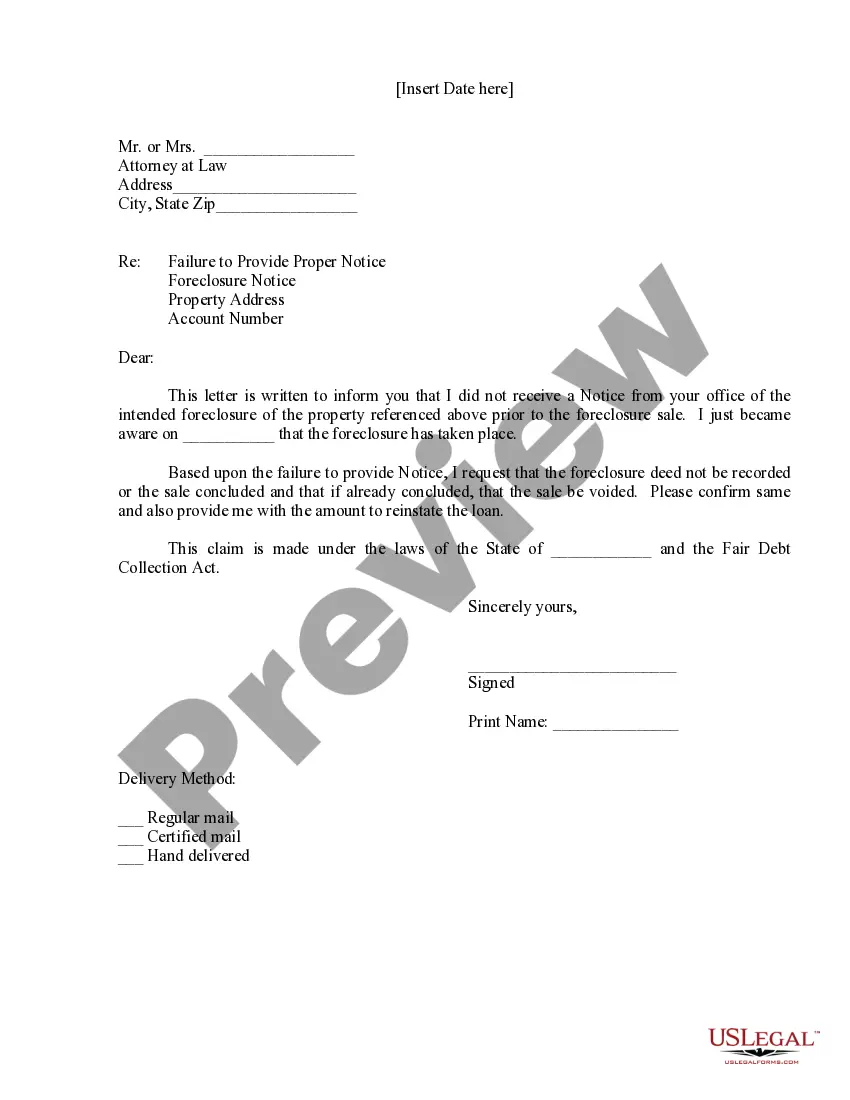
How to fill out COBRA Notice Timing Delivery Chart?
US Legal Forms - one among the largest collections of legal documents in the United States - provides a diverse array of legal form templates that you can download or print.
By utilizing the website, you can access thousands of forms for business and personal purposes, organized by categories, states, or keywords. You can find the most recent versions of forms such as the Guam COBRA Notice Timing Delivery Chart in mere moments.
If you already possess a subscription, Log In and retrieve the Guam COBRA Notice Timing Delivery Chart from the US Legal Forms collection. The Download button will appear on each form you access. You have access to all previously downloaded forms in the My documents section of your account.
Make edits. Complete, alter, print, and sign the downloaded Guam COBRA Notice Timing Delivery Chart.
Every template you added to your account does not have an expiration date and is yours indefinitely. So, to download or print another copy, simply go to the My documents section and click on the form you require.
- Make sure you have selected the correct form for your jurisdiction/county. Click the Preview button to review the details of the form.
- Check the form description to confirm that you have selected the correct one.
- If the form does not meet your requirements, utilize the Search area at the top of the screen to find one that does.
- Once you are satisfied with the form, confirm your choice by clicking the Purchase now button. Then, choose your preferred payment plan and provide your details to register for an account.
- Process the transaction. Use your Visa or Mastercard or PayPal account to complete the transaction.
- Select the format and download the form to your device.
Form popularity
FAQ
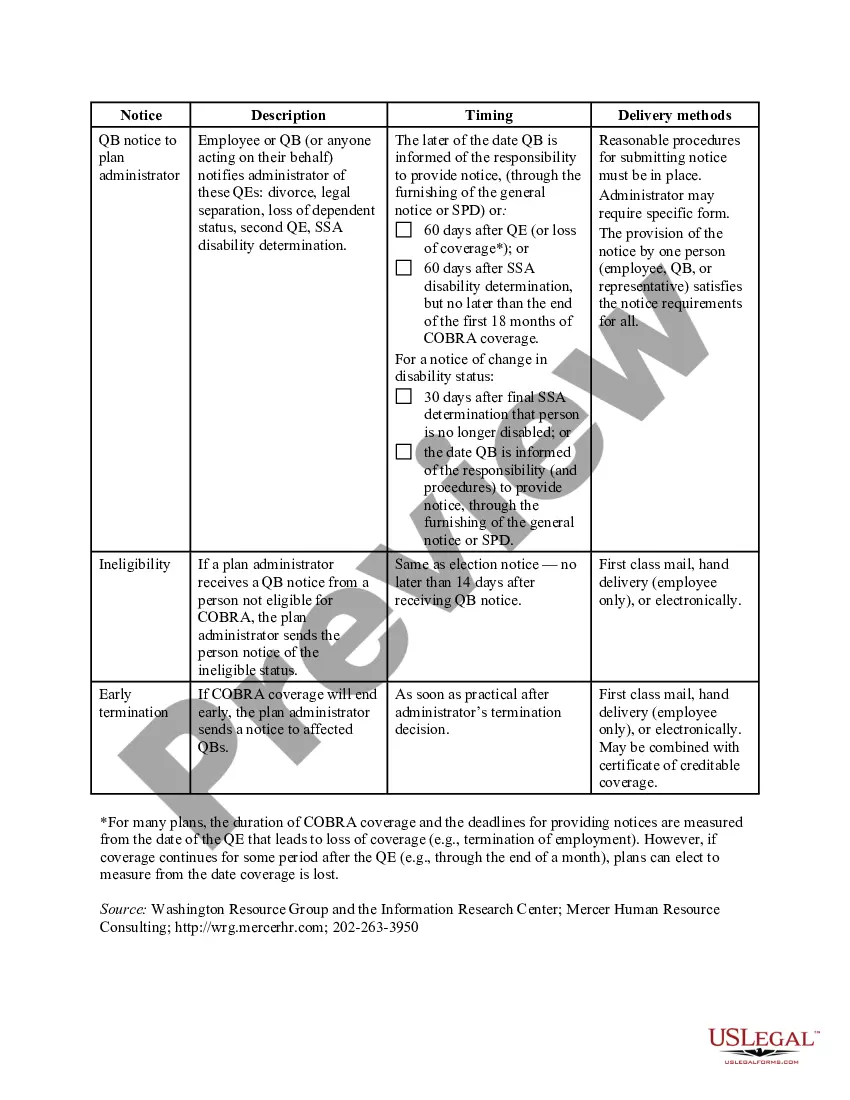
The initial notice, also referred to as the general notice, communicates general COBRA rights and obligations to each covered employee (and his or her spouse) who becomes covered under the group health plan.
COBRA is always retroactive to the day after your previous coverage ends, and you'll need to pay your premiums for that period too. One advantage of enrolling right away is that you can keep seeing doctors and filling prescriptions without a break in coverage. COBRA allows you to keep the exact same benefits as before.
In addition, employers can provide COBRA notices electronically (via email, text message, or through a website) during the Outbreak Period, if they reasonably believe that plan participants and beneficiaries have access to these electronic mediums.
Your employer must mail you the COBRA information and forms within 14 days after receiving notification of the qualifying event. You are responsible for making sure your COBRA coverage goes into and stays in effect - if you do not ask for COBRA coverage before the deadline, you may lose your right to COBRA coverage.
In addition, employers can provide COBRA notices electronically (via email, text message, or through a website) during the Outbreak Period, if they reasonably believe that plan participants and beneficiaries have access to these electronic mediums.
The initial notice, also referred to as the general notice, communicates general COBRA rights and obligations to each covered employee (and his or her spouse) who becomes covered under the group health plan.
Employers should send notices by first-class mail, obtain a certificate of mailing from the post office, and keep a log of letters sent. Certified mailing should be avoided, as a returned receipt with no delivery acceptance signature proves the participant did not receive the required notice.
If You Do Not Receive Your COBRA PaperworkReach out to the Human Resources Department and ask for the COBRA Administrator. They may use a third-party administrator to handle your enrollment. If the employer still does not comply you can call the Department of Labor at 1-866-487-2365.
COBRA is always retroactive to the day after your previous coverage ends, and you'll need to pay your premiums for that period too. One advantage of enrolling right away is that you can keep seeing doctors and filling prescriptions without a break in coverage. COBRA allows you to keep the exact same benefits as before.
Both full- and part-time employees are counted to determine whether a plan is subject to COBRA. Each part-time employee counts as a fraction of a full-time employee, with the fraction equal to the number of hours worked divided by the hours an employee must work to be considered full time.