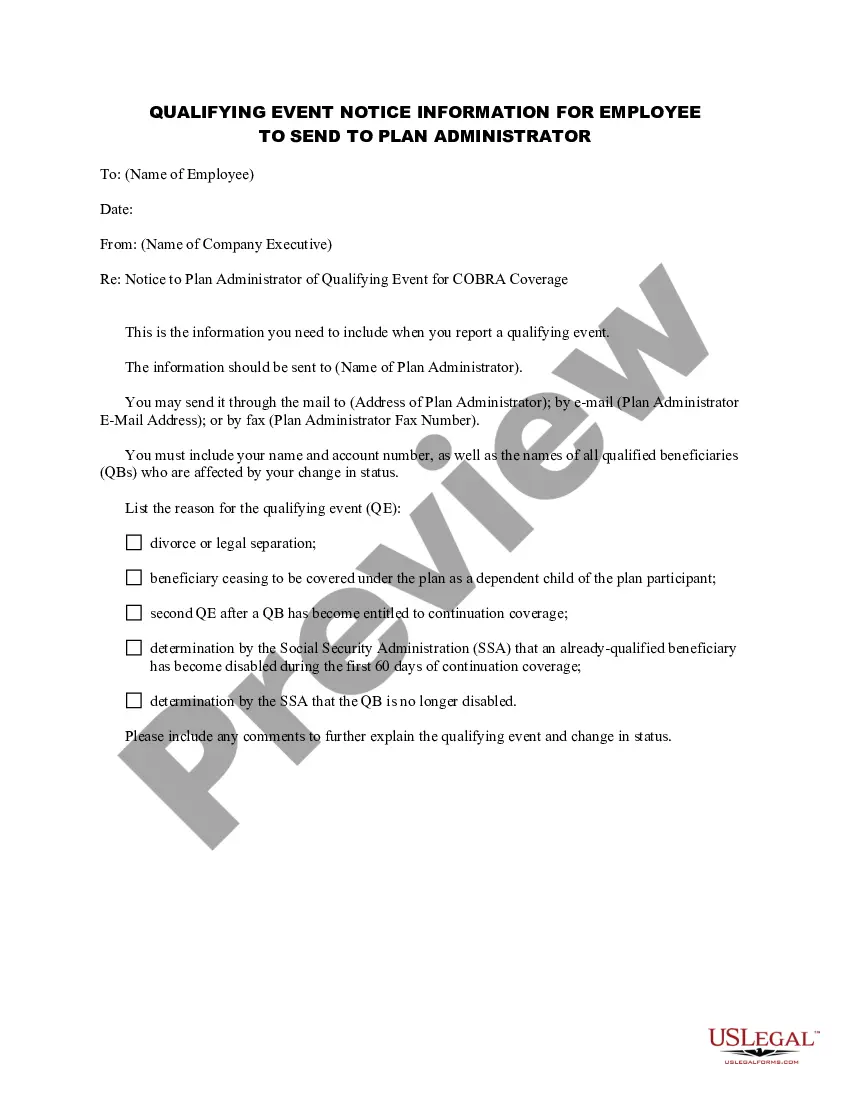
Georgia Qualifying Event Notice Information for Employer to Plan Administrator
Description
How to fill out Qualifying Event Notice Information For Employer To Plan Administrator?
Finding the correct legal document template can be a challenging task.
Certainly, there are numerous templates accessible online, but how will you obtain the legal form you need.
Utilize the US Legal Forms site.
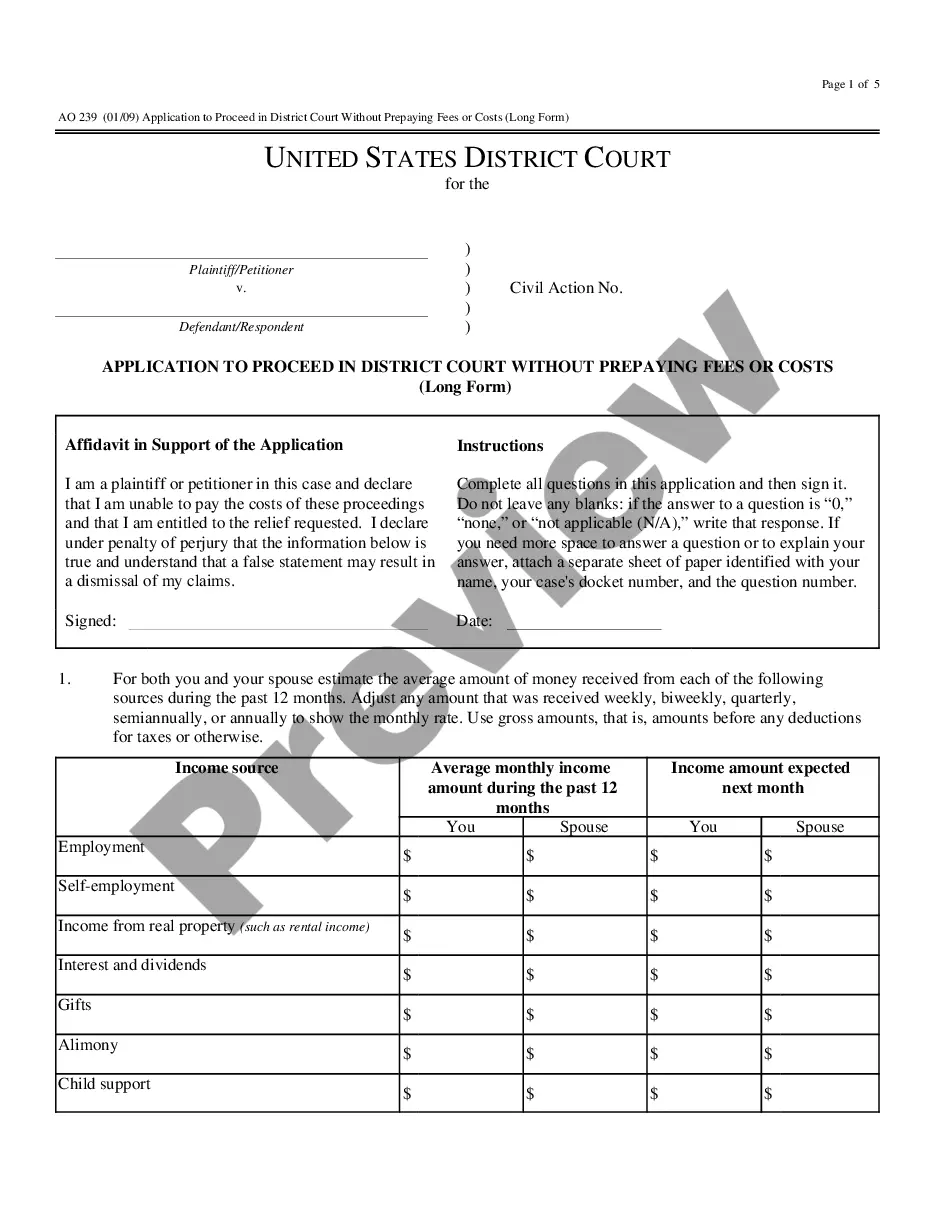
First, ensure you have selected the correct form for your city/state. You can view the form using the Preview button and read the form description to confirm it is the right one for you.
- The service offers thousands of templates, including the Georgia Qualifying Event Notice Information for Employer to Plan Administrator, which you can use for both business and personal needs.
- All forms are verified by specialists and comply with federal and state regulations.
- If you are already registered, Log In to your account and click the Download button to get the Georgia Qualifying Event Notice Information for Employer to Plan Administrator.
- Use your account to browse the legal forms you may have purchased previously.
- Go to the My documents section of your account to obtain another copy of the document you need.
- If you are a new user of US Legal Forms, here are easy steps for you to follow.
Form popularity
FAQ
What is mini-COBRA? Georgia, like some other states, has passed mini-COBRA laws to cover businesses that offer group health insurance but employ fewer than 20 employees. As such, in Georgia, if you employ at least two employees, you're obligated to offer COBRA to former employees.
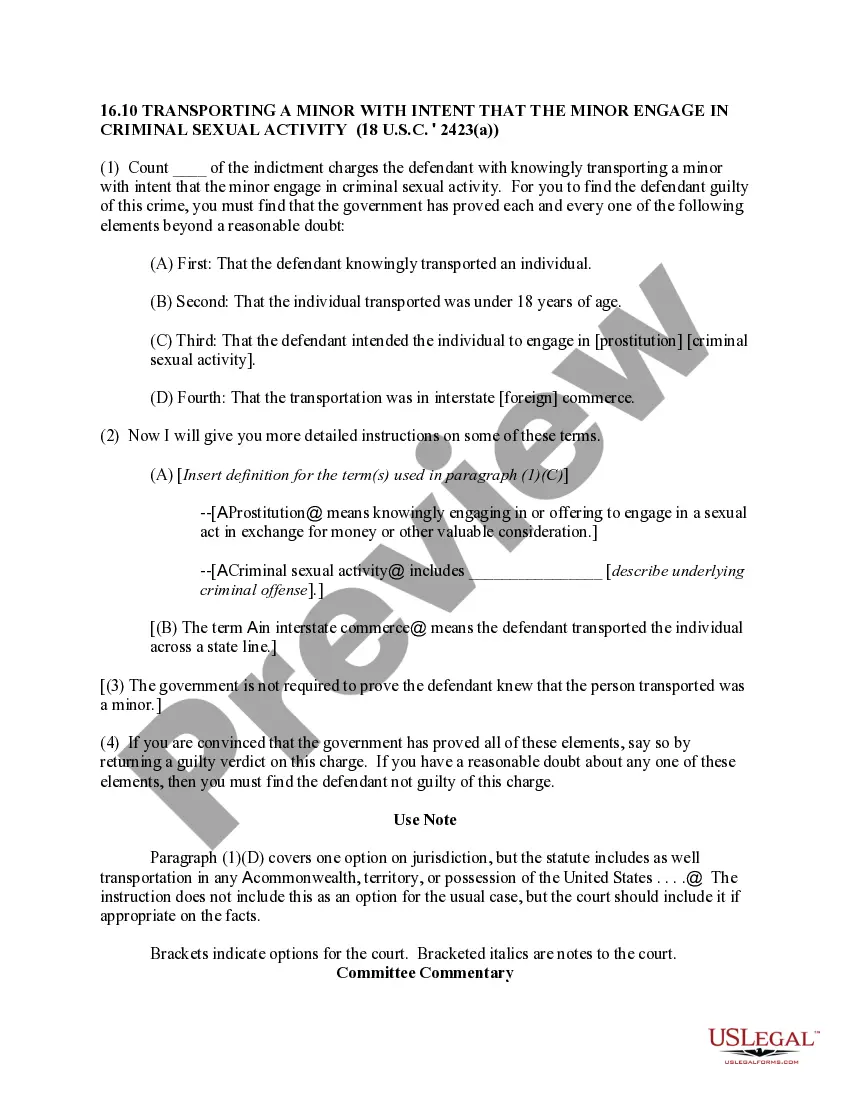
COBRA Qualifying Event Notice The employer must notify the plan if the qualifying event is: Termination or reduction in hours of employment of the covered employee, 2022 Death of the covered employee, 2022 Covered employee becoming entitled to Medicare, or 2022 Employer bankruptcy.
When the qualifying event is the covered employee's termination of employment or reduction in hours of employment, qualified beneficiaries are entitled to 18 months of continuation coverage.
Key Takeaways. COBRA provides a good option for keeping your employer-sponsored health plan for a while after you leave your job. Although, the cost can be high. Make an informed choice by looking at all your options during the 60-day enrollment period, and don't focus on the premium alone.
COBRA is a federal law about health insurance. If you lose or leave your job, COBRA lets you keep your existing employer-based coverage for at least the next 18 months. Your existing healthcare plan will now cost you more. Under COBRA, you pay the whole premium including the share your former employer used to pay.
Losing COBRA Benefits Here's the good news: Rolling off of COBRA coverage is a qualifying event that opens a special enrollment period for you to purchase your own health coverage. And you'll have more options, flexibility and control of your health plan outside of COBRA with an individual health insurance plan.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
The following are qualifying events: the death of the covered employee; a covered employee's termination of employment or reduction of the hours of employment; the covered employee becoming entitled to Medicare; divorce or legal separation from the covered employee; or a dependent child ceasing to be a dependent under
Second qualifying events may include the death of the covered employee, divorce or legal separation from the covered employee, the covered employee becoming entitled to Medicare benefits (under Part A, Part B or both), or a dependent child ceasing to be eligible for coverage as a dependent under the group health plan.