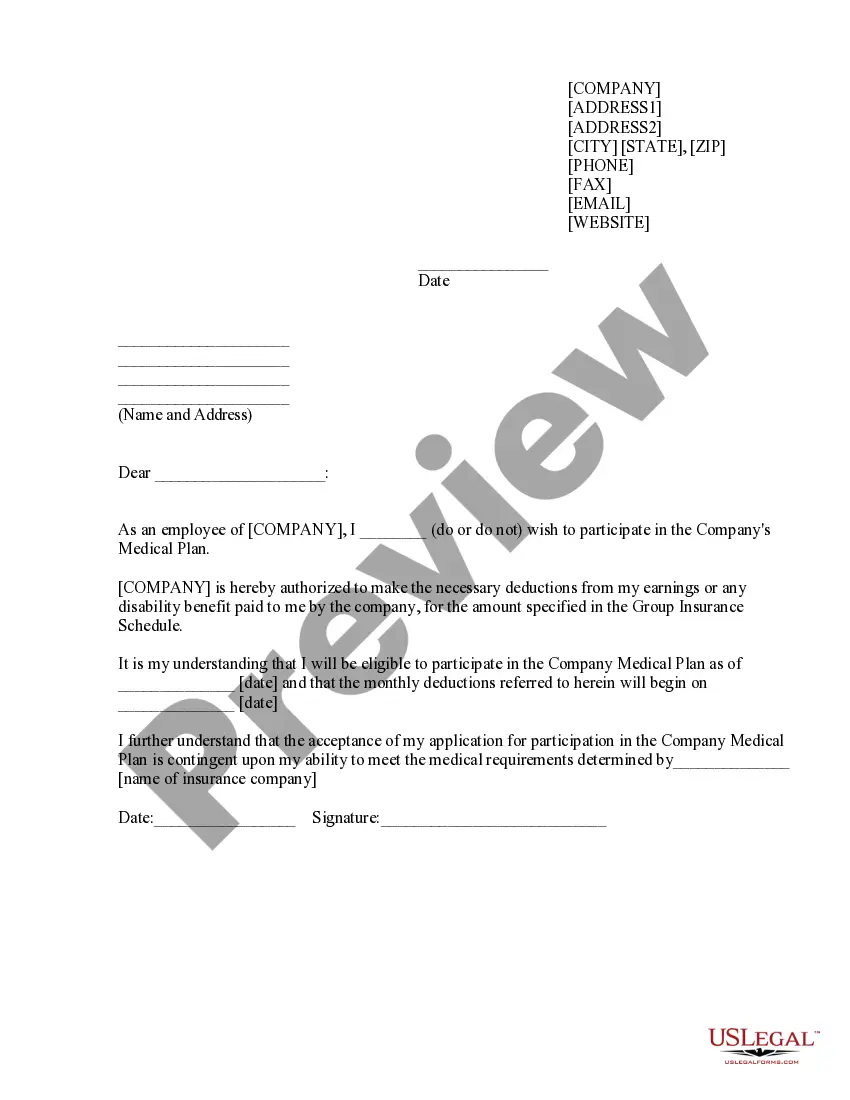
Delaware Sample COBRA Enrollment and / or Waiver Letter
Description
How to fill out Sample COBRA Enrollment And / Or Waiver Letter?
It is feasible to spend countless hours online searching for the valid document template that meets the state and federal criteria you need.
US Legal Forms offers an extensive array of legal forms that can be reviewed by experts.
It is easy to download or print the Delaware Sample COBRA Enrollment and/or Waiver Letter from the service.
- If you already possess a US Legal Forms account, you can Log In and select the Obtain option.
- Subsequently, you can complete, modify, print, or sign the Delaware Sample COBRA Enrollment and/or Waiver Letter.
- Every legal document template you purchase is yours permanently.
- To acquire another copy of the purchased form, visit the My documents section and click on the relevant option.
- If this is your initial time using the US Legal Forms site, follow the straightforward instructions below.
- First, ensure that you have selected the correct document template for the county/city of your choice.
- Read the form description to confirm you have selected the correct form. If available, utilize the Review option to check the document template as well.
- If you wish to find another version of the form, use the Search field to locate the template that suits your needs and requirements.
- Once you have found the template you desire, click on Buy now to proceed.
- Select the pricing plan you prefer, enter your details, and register for your account on US Legal Forms.
- Complete the payment. You can use your Visa or Mastercard or PayPal account to purchase the legal document.
- Choose the format of the document and download it to your device.
- Make modifications to your document if necessary.
- You can complete, edit, sign, and print the Delaware Sample COBRA Enrollment and/or Waiver Letter.
- Access and print a vast number of document templates using the US Legal Forms site, which offers the most extensive collection of legal forms.
- Utilize professional and state-specific templates to address your business or personal needs.
Form popularity
FAQ
Employers should send notices by first-class mail, obtain a certificate of mailing from the post office, and keep a log of letters sent. Certified mailing should be avoided, as a returned receipt with no delivery acceptance signature proves the participant did not receive the required notice.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) is federal law that extends your current group health insurance when you experience a qualifying event such as termination of employment or reduction of hours to part-time status.
COBRA coverage follows a "qualifying event". An example of a qualifying event would be if your hours were reduced or you lost your job (as long as there was no gross misconduct). Your employer must mail you the COBRA information and forms within 14 days after receiving notification of the qualifying event.
If You Do Not Receive Your COBRA PaperworkReach out to the Human Resources Department and ask for the COBRA Administrator. They may use a third-party administrator to handle your enrollment. If the employer still does not comply you can call the Department of Labor at 1-866-487-2365.
You should get a notice in the mail about your COBRA and Cal-COBRA rights. You have 60 days after being notified to sign up. If you are eligible for Federal COBRA and did not get a notice, contact your employer. If you are eligible for Cal-COBRA and did not get a notice, contact your health plan.
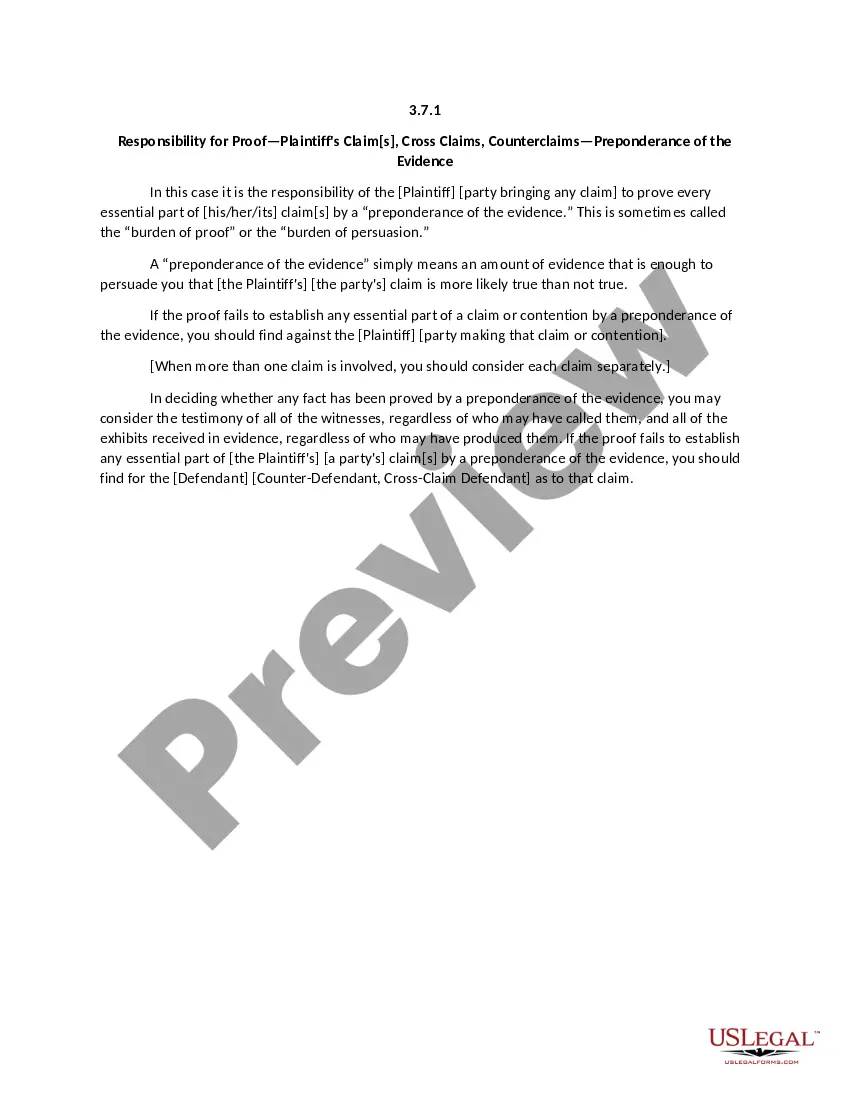
COBRA continuation coverage notices are documents that explain employees' rights under the Consolidated Omnibus Budget Reconciliation Act of 1985. These documents generally contain a variety of information, including the following: The name of the health insurance plan.
The purpose of this letter is to inform you of your rights and responsibilities as a plan participant. Qualifying Event: At the end of your employment or because of reduction of hours (not maintain full-time status) you will receive this letter.
In addition, employers can provide COBRA notices electronically (via email, text message, or through a website) during the Outbreak Period, if they reasonably believe that plan participants and beneficiaries have access to these electronic mediums.
The initial notice, also referred to as the general notice, communicates general COBRA rights and obligations to each covered employee (and his or her spouse) who becomes covered under the group health plan.
Although the earlier rules only covered summary plan descriptions (SPDs) and summary annual reports, the final rules provide that all ERISA-required disclosure documents can be sent electronically -- this includes COBRA notices as well as certificates of creditable coverage under the Health Insurance Portability and