District of Columbia Acknowledgment of Receipt of COBRA Notice
Description
How to fill out Acknowledgment Of Receipt Of COBRA Notice?
US Legal Forms - one of the largest collections of legal documents in the United States - offers a variety of legal form templates that you can download or print. By using the site, you can discover thousands of forms for both business and personal purposes, organized by categories, states, or keywords.
You can obtain the latest templates of forms such as the District of Columbia Acknowledgment of Receipt of COBRA Notice within moments. If you hold a subscription, Log In to access the District of Columbia Acknowledgment of Receipt of COBRA Notice in the US Legal Forms library. The Download button will appear on each form you view.
You can find all previously saved forms in the My documents section of your account.
Process the transaction. Use a credit card or PayPal account to complete the transaction.
Select the format and download the form to your device. Make changes. Fill out, edit, print, and sign the saved District of Columbia Acknowledgment of Receipt of COBRA Notice. Each template you added to your account has no expiration date and is yours indefinitely. Thus, if you wish to download or print an additional copy, simply visit the My documents section and click on the form you desire. Access the District of Columbia Acknowledgment of Receipt of COBRA Notice with US Legal Forms, the most extensive library of legal form templates. Utilize thousands of professional and state-specific templates that meet your business or personal needs.
- If you are using US Legal Forms for the first time, here are simple steps to help you get started.
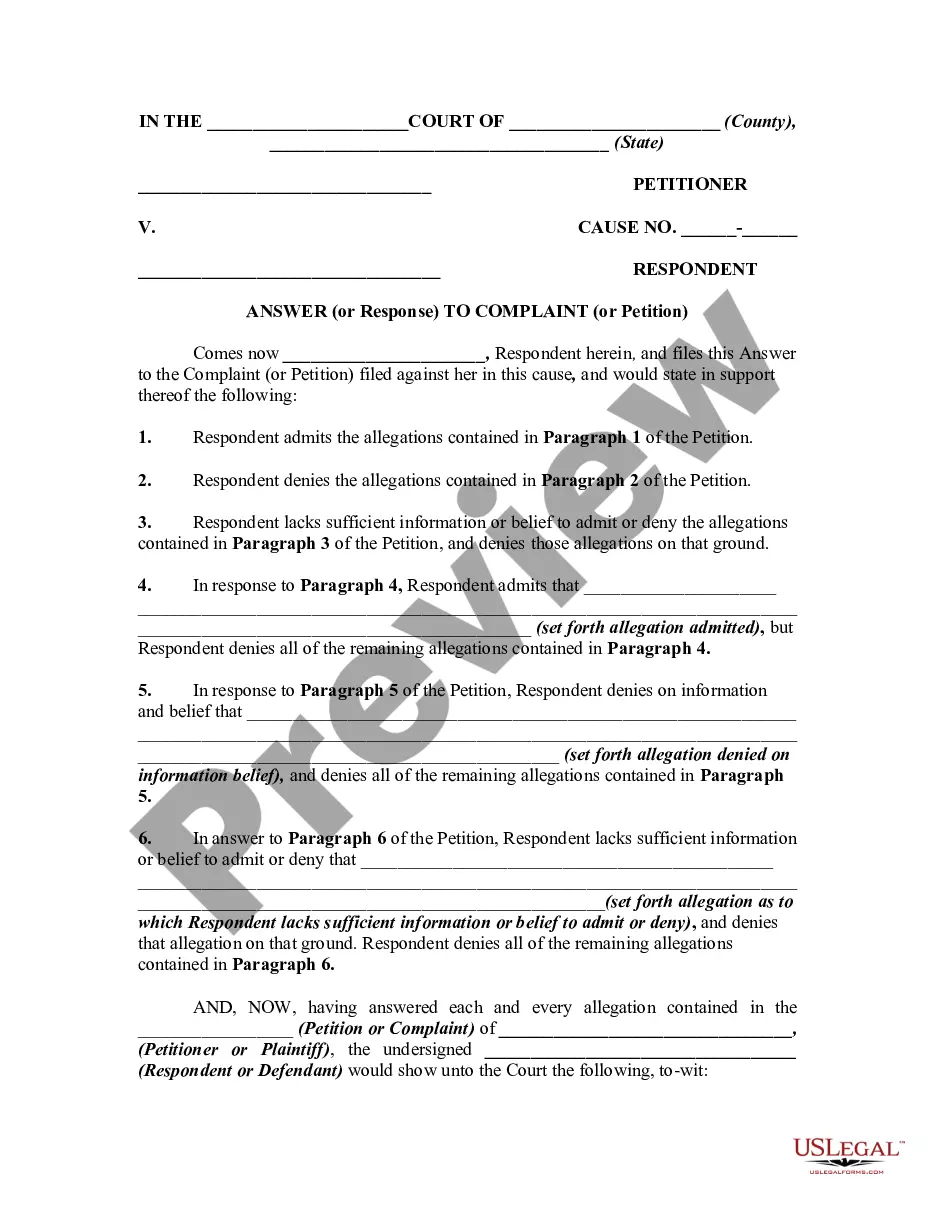
- Ensure you have selected the correct form for your city/state. Click on the Preview button to review the form's content.
- Examine the form description to ensure you have selected the correct one.
- If the form does not meet your needs, use the Search field at the top of the screen to find one that does.
- If you are satisfied with the form, confirm your selection by clicking the Get now button.
- Then, choose your preferred payment plan and provide your details to register for an account.
Form popularity
FAQ
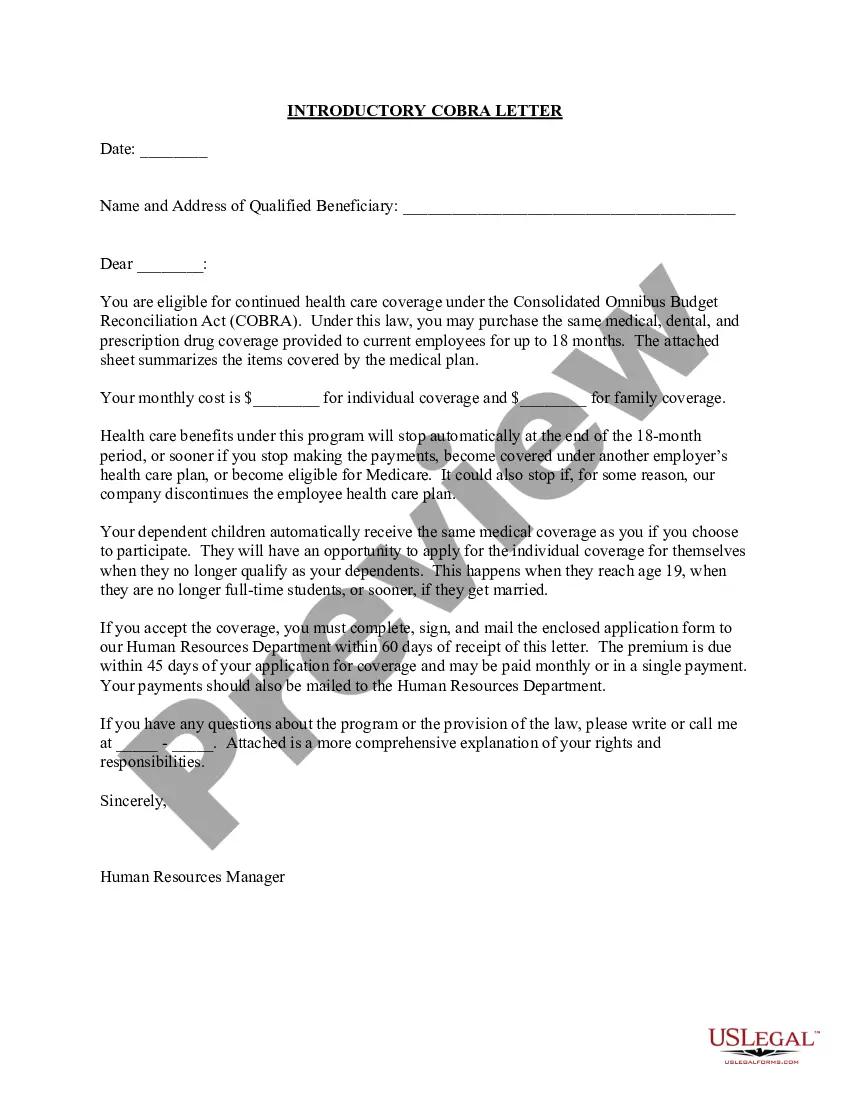
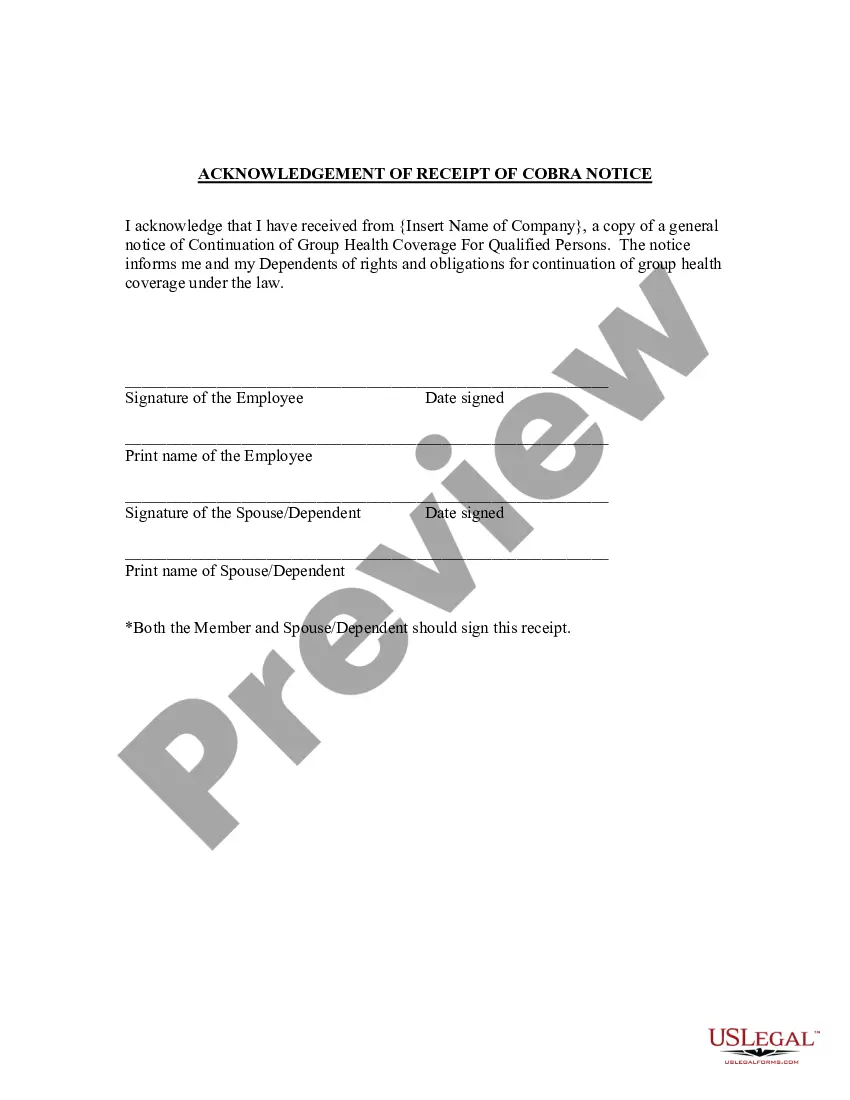
The COBRA Notice informs the qualified beneficiary of their rights under COBRA law, and the form allows the qualified beneficiary to elect COBRA coverage to continue enrollment in benefits.
How COBRA Works In Delaware. The Federal COBRA Law requires businesses with 20 or more workers to provide the option to elect the same group health coverage to workers and their families if that insurance would end. Exempt from this rule are government employers, churches and tax-exempt organizations.
When does COBRA continuation coverage startCOBRA is always effective the day after your active coverage ends. For most, active coverage terminates at the end of a month and COBRA is effective on the first day of the next month.
Maryland law requires continuation coverage be offered to the former spouse and dependent children (qualified secondary beneficiary) of an employee after a divorce. Additionally, coverage must be offered to a child of the employee who is born to the former spouse after the divorce.
The District of Columbia requires that group insurance plans sponsored by employers not covered by the Consolidated Omnibus Budget Reconciliation Act (COBRA) provide three months of continuation coverage following termination of coverage for most of the same reasons that are covered by the federal law (DC Code Sec.
In addition, employers can provide COBRA notices electronically (via email, text message, or through a website) during the Outbreak Period, if they reasonably believe that plan participants and beneficiaries have access to these electronic mediums.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
COBRA continuation coverage notices are documents that explain employees' rights under the Consolidated Omnibus Budget Reconciliation Act of 1985. These documents generally contain a variety of information, including the following: The name of the health insurance plan.
The D.C. mini-COBRA law provides for 3 months of continuation coverage, except in the case of terminations for gross misconduct. The employer is required to provide notice to the employee within 15 days after the date that coverage would otherwise terminate.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,