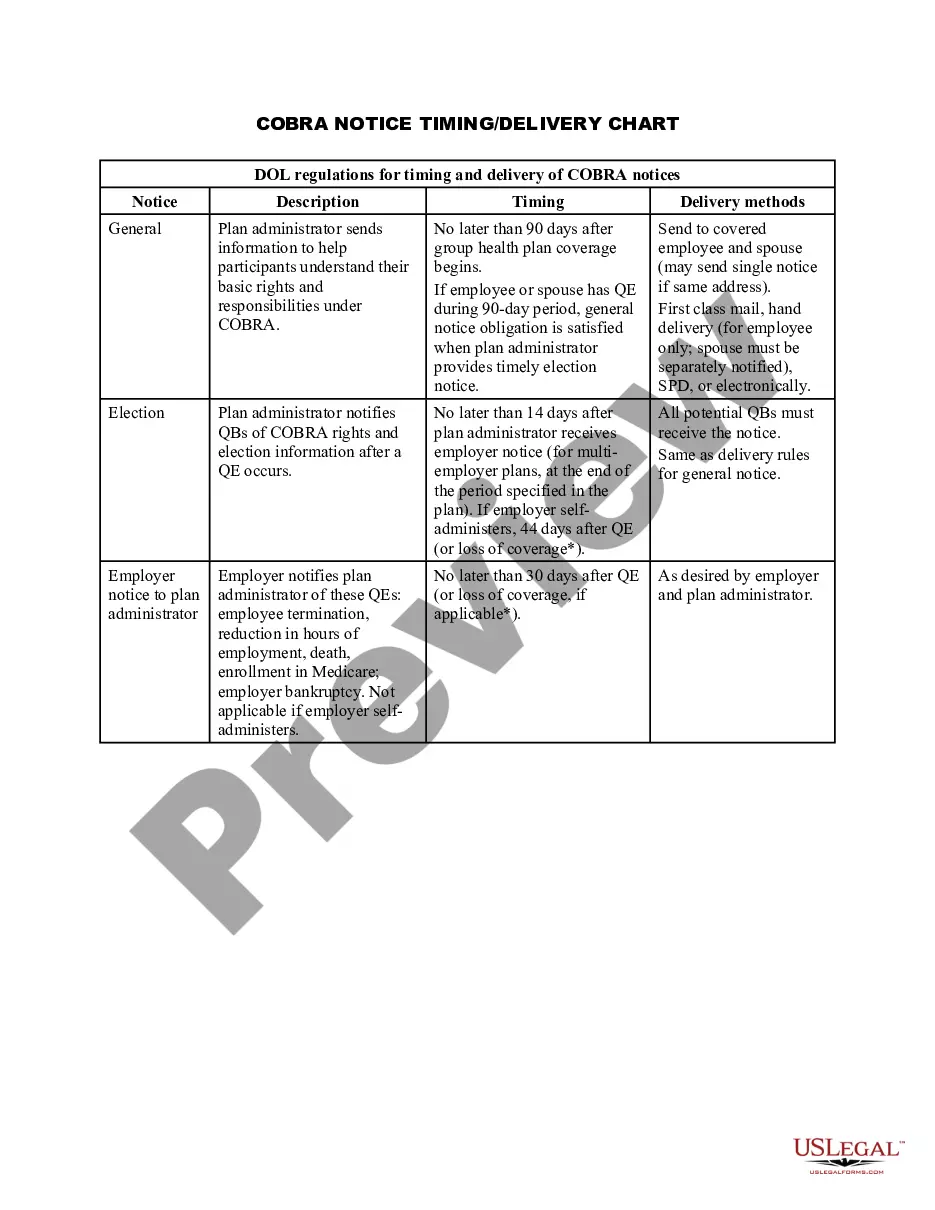
Connecticut COBRA Notice Timing Delivery Chart
Description
How to fill out COBRA Notice Timing Delivery Chart?
Selecting the optimal approved document template can be quite a challenge.
Clearly, there are numerous templates accessible online, but how can you find the authorized form you require.
Utilize the US Legal Forms website. The service offers thousands of templates, including the Connecticut COBRA Notice Timing Delivery Chart, that can be utilized for both commercial and personal purposes.
Firstly, ensure that you have selected the appropriate form for your city/state. You can review the form using the Preview option and examine the form summary to confirm that this is indeed the correct one for you.
- All the forms are reviewed by experts and comply with federal and state regulations.
- If you are already registered, sign in to your account and click the Download button to access the Connecticut COBRA Notice Timing Delivery Chart.
- Use your account to search through the legal forms you have previously acquired.
- Navigate to the My documents section of your account and obtain another copy of the document you need.
- If you are a new customer of US Legal Forms, here are some straightforward instructions for you to follow.
Form popularity
FAQ
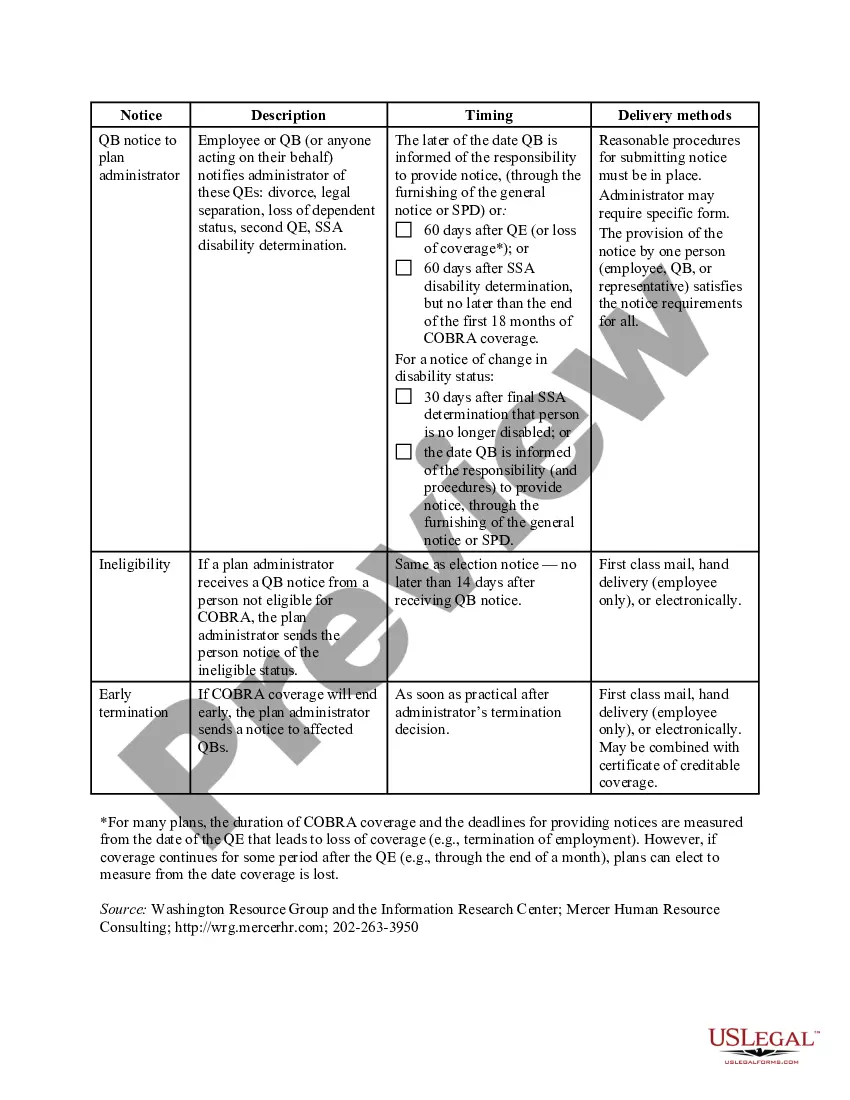
COBRA continuation coverage may be terminated if we don't receive timely payment of the premium. What is the grace period for monthly COBRA premiums? After election and initial payment, qualified beneficiaries have a 30-day grace period to make monthly payments (that is, 30 days from the due date).
COBRA permits you and your dependents to continue in your employer's group health plan after your job ends. If your employer has 20 or more employees, you may be eligible for COBRA continuation coverage when you retire, quit, are fired, or work reduced hours.
If You Do Not Receive Your COBRA PaperworkReach out to the Human Resources Department and ask for the COBRA Administrator. They may use a third-party administrator to handle your enrollment. If the employer still does not comply you can call the Department of Labor at 1-866-487-2365.
COBRA allows a 30-day grace period. If your premium payment is not received within the 30-day grace period, your coverage will automatically be terminated without advance warning. You will receive a termination letter at that time to notify you of a lapse in your coverage due to non-payment of premiums.
Are there penalties for failing to provide a COBRA notice? Yes, and the penalties can be substantial. Under the Employment Retirement Income Security Act of 1974 (ERISA), a penalty of up to $110 per day may be imposed for failing to provide a COBRA notice.
Employers who fail to comply with the COBRA requirements can be required to pay a steep price. Failure to provide the COBRA election notice within this time period can subject employers to a penalty of up to $110 per day, as well as the cost of medical expenses incurred by the qualified beneficiary.
COBRA coverage follows a "qualifying event". An example of a qualifying event would be if your hours were reduced or you lost your job (as long as there was no gross misconduct). Your employer must mail you the COBRA information and forms within 14 days after receiving notification of the qualifying event.
In most cases, COBRA provides for continuation of health plan coverage for up to 18 months following the work separation. COBRA rights accrue once a "qualifying event" occurs - basically, a qualifying event is any change in the employment relationship that results in loss of health plan benefits.
New York State law requires small employers (less than 20 employees) to provide the equivalent of COBRA benefits. You are entitled to 36 months of continued health coverage at a monthly cost to you of 102% of the actual cost to the employer which may be different from the amount deducted from your paychecks.
Initial COBRA notices must generally be provided within 14 days of the employer notifying the third-party administrator (TPA) of a qualifying event.