Connecticut Qualifying Event Notice Information for Employer to Plan Administrator
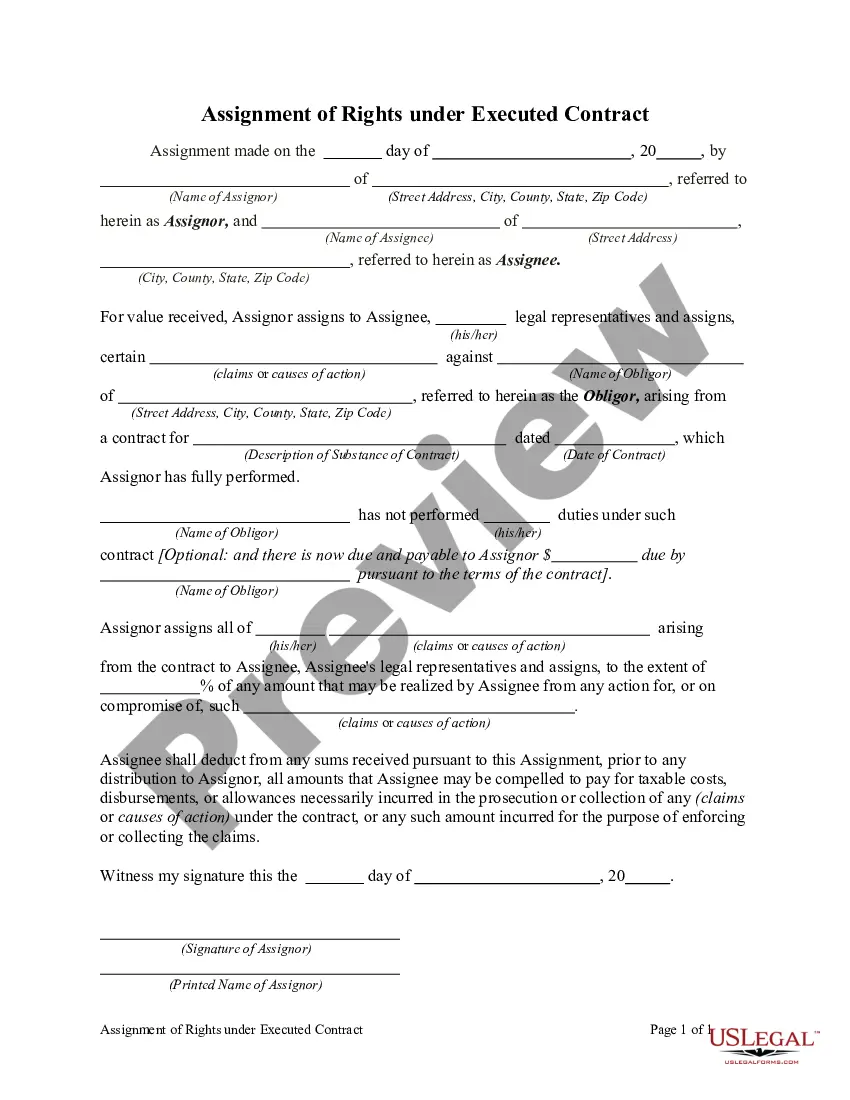
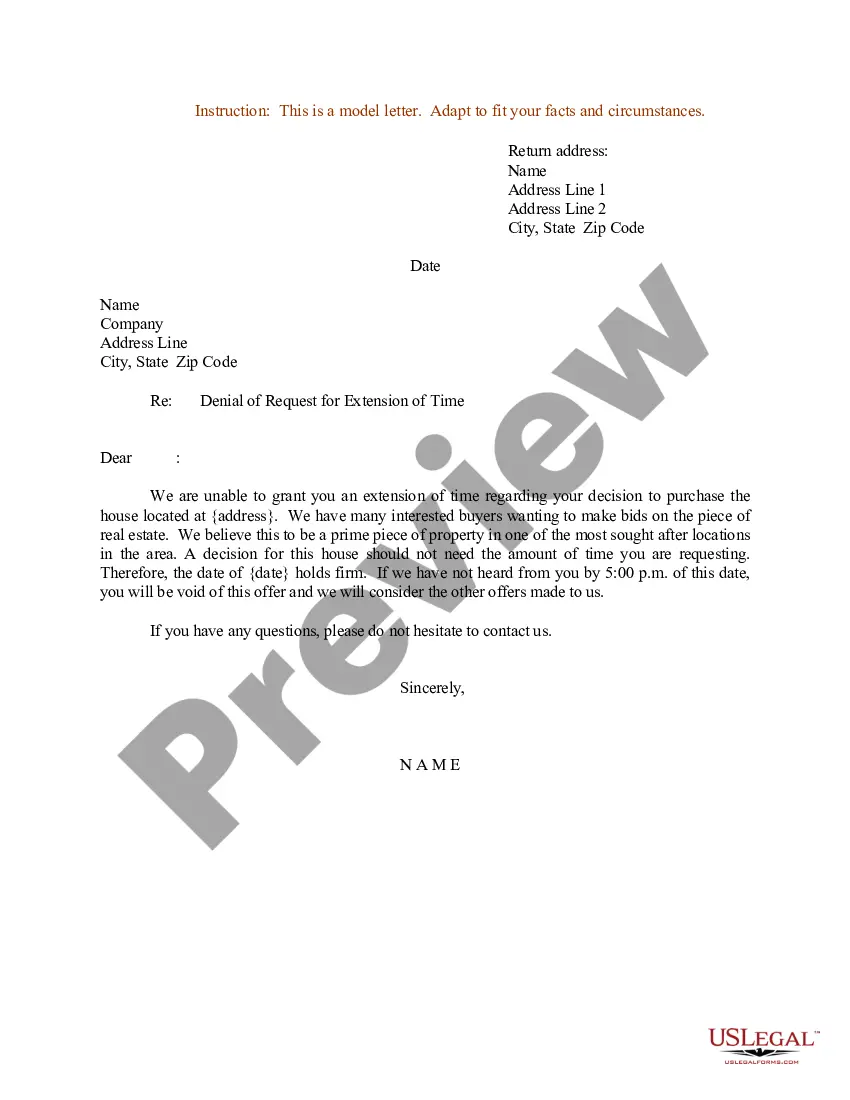
Description
How to fill out Qualifying Event Notice Information For Employer To Plan Administrator?
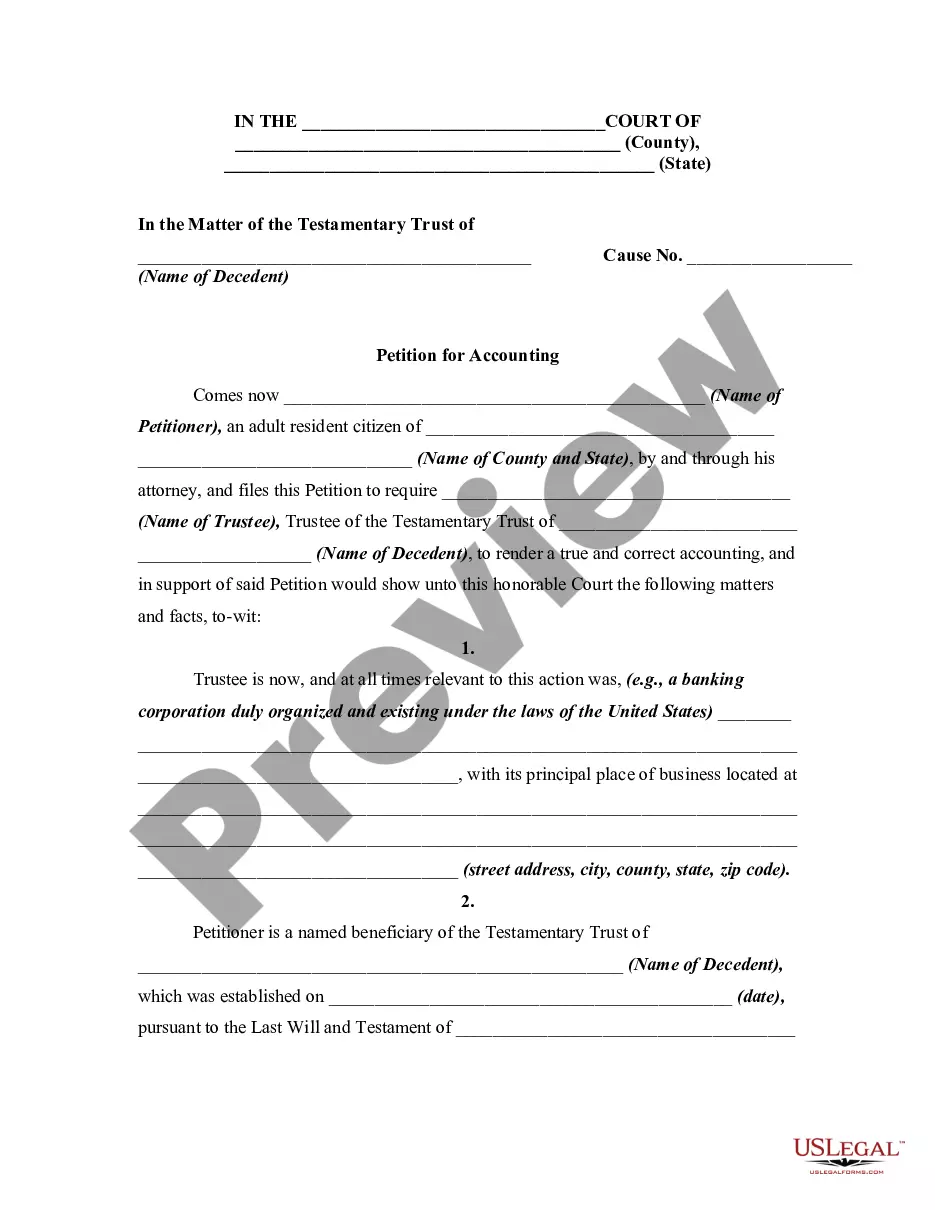
US Legal Forms - one of the largest collections of legal documents in the United States - provides a vast assortment of legal form templates that you can download or print.
By using the website, you can access thousands of forms for business and personal use, organized by categories, states, or keywords.
You can find the latest versions of forms such as the Connecticut Qualifying Event Notice Information for Employer to Plan Administrator in just a few moments.
Check the form description to confirm you have chosen the right one.
If the form does not meet your needs, utilize the Search area at the top of the screen to find one that does.
- If you already have an account, Log In to download the Connecticut Qualifying Event Notice Information for Employer to Plan Administrator from the US Legal Forms library.
- The Download button will appear on every form you view.
- You have access to all previously saved forms in the My documents section of your profile.
- If this is your first time using US Legal Forms, here are some straightforward steps to get started.
- Ensure you select the correct form for your region/county.
- Click the Review button to examine the form's content.
Form popularity
FAQ
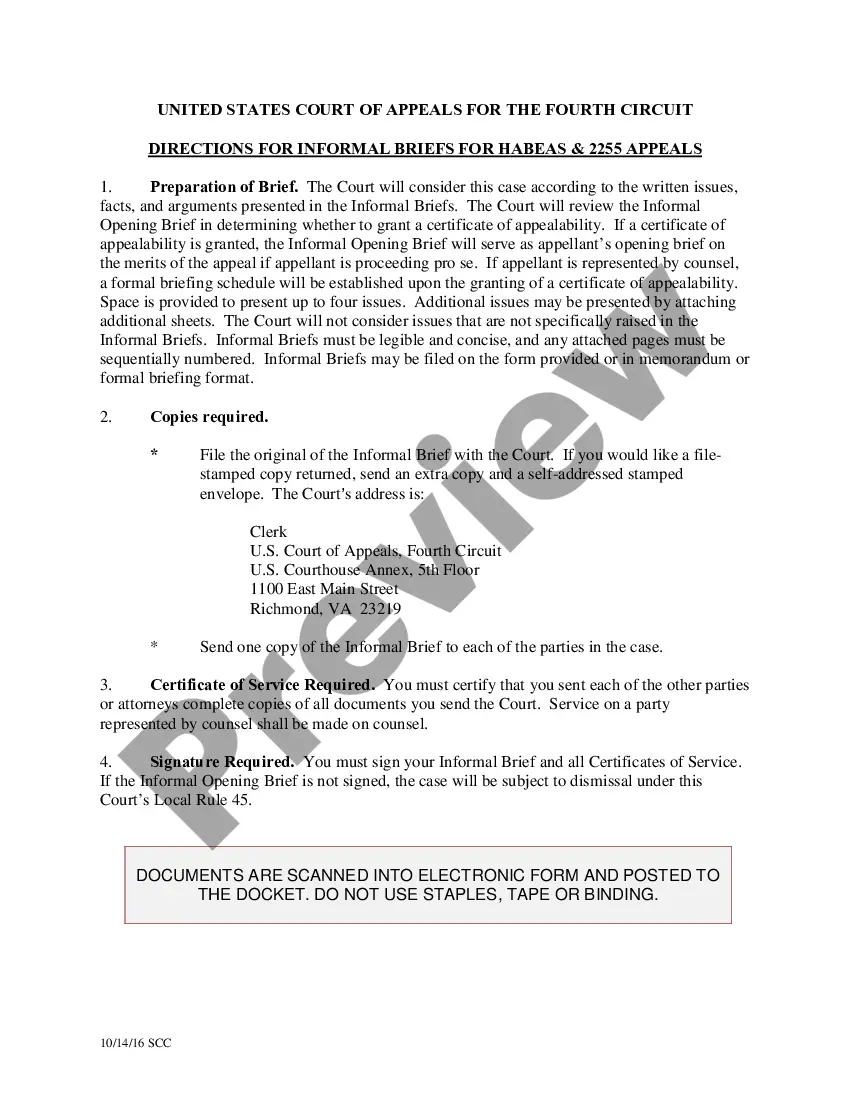
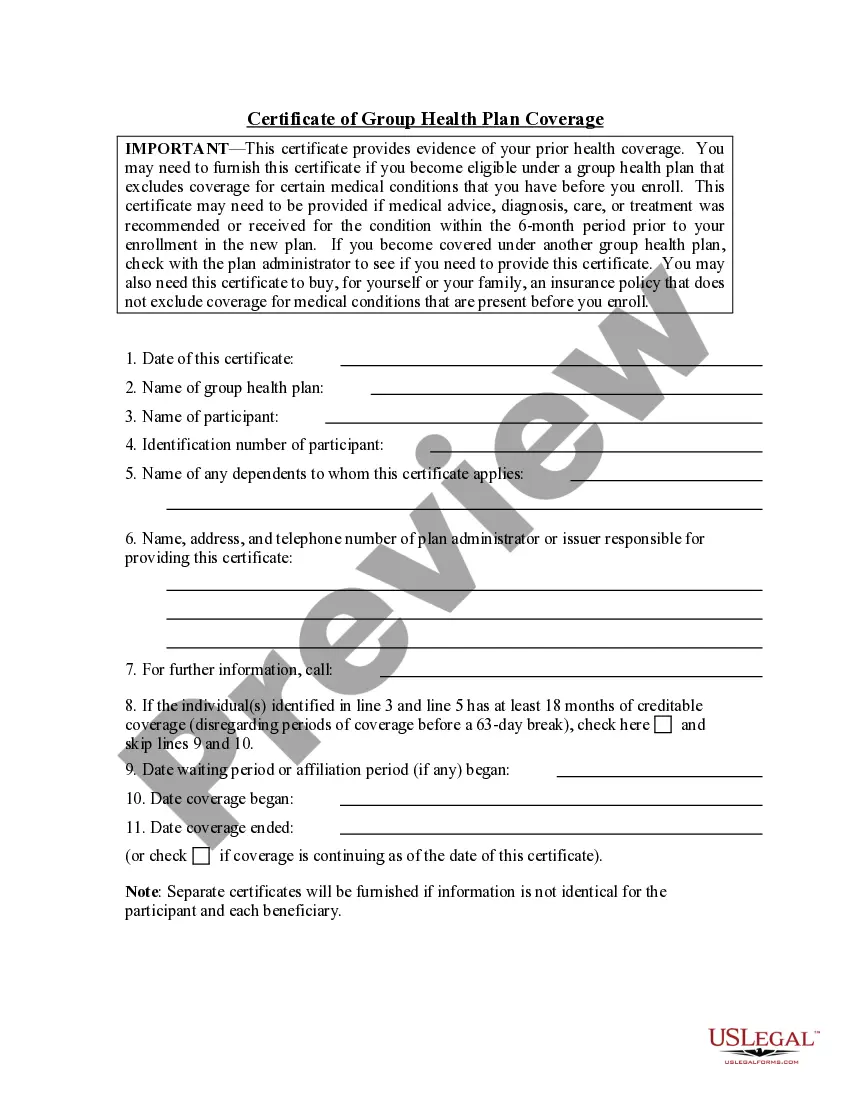
When the qualifying event is the covered employee's termination of employment or reduction in hours of employment, qualified beneficiaries are entitled to 18 months of continuation coverage.
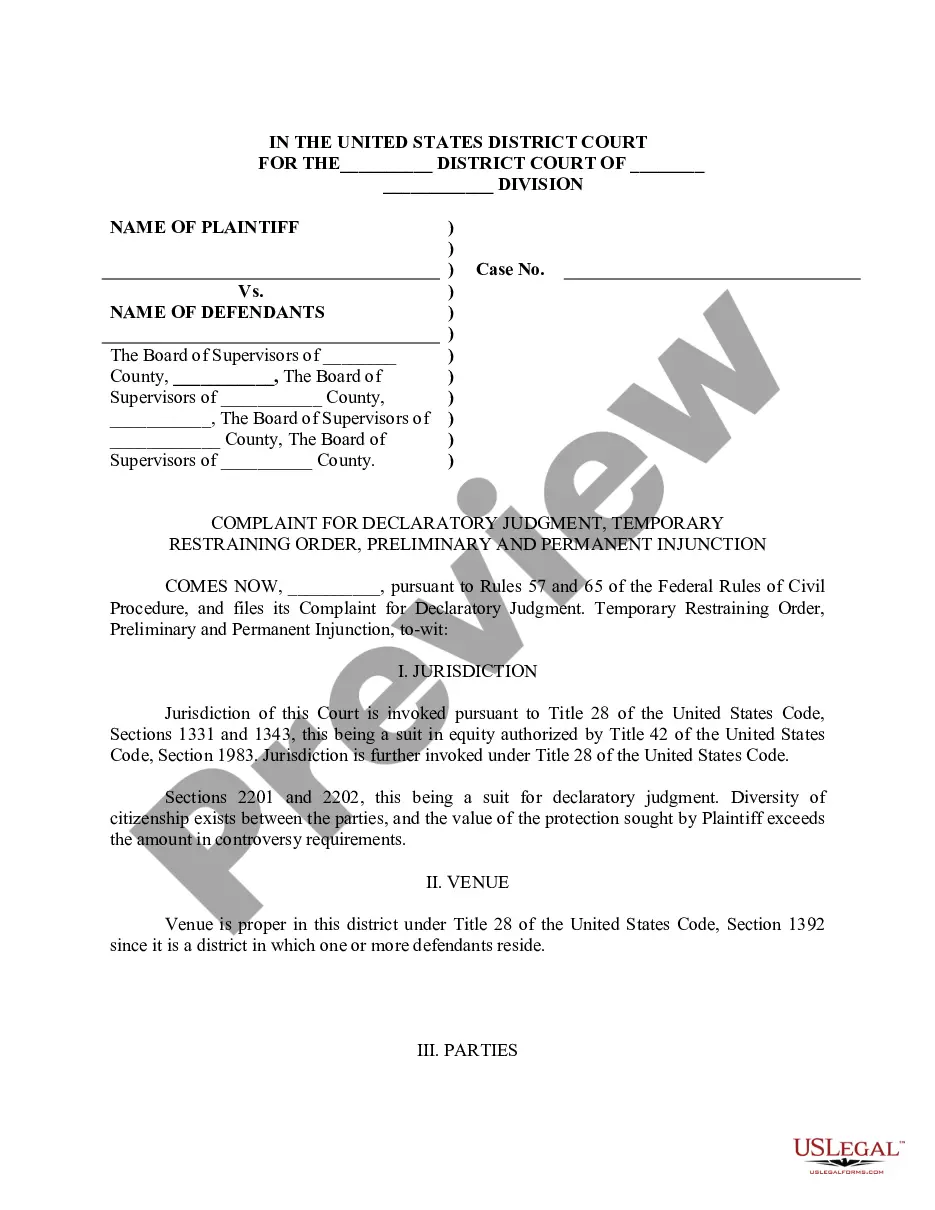
The Patient Protection and Affordable Care Act, referred to as the Affordable Care Act or ACA for short, is the comprehensive health care reform law enacted in March 2010. The law has 3 primary goals: Make affordable health insurance available to more people.
The following are qualifying events: the death of the covered employee; a covered employee's termination of employment or reduction of the hours of employment; the covered employee becoming entitled to Medicare; divorce or legal separation from the covered employee; or a dependent child ceasing to be a dependent under
Do small employers have to offer health insurance in Connecticut? In Connecticut, all employers with 50 or more full-time employees are required to offer some form of health insurance benefit.
COBRA Qualifying Event Notice The employer must notify the plan if the qualifying event is: Termination or reduction in hours of employment of the covered employee, 2022 Death of the covered employee, 2022 Covered employee becoming entitled to Medicare, or 2022 Employer bankruptcy.
The federal agency that oversees CMS, which administers programs for protecting the health of all Americans, including Medicare, the Marketplace, Medicaid, and the Children's Health Insurance Program (CHIP). For more information, visit hhs.gov.
Second qualifying events may include the death of the covered employee, divorce or legal separation from the covered employee, the covered employee becoming entitled to Medicare benefits (under Part A, Part B or both), or a dependent child ceasing to be eligible for coverage as a dependent under the group health plan.
The federal ERISA laws govern employer-sponsored health plans, except those offered by a church or a governmental entity for its employees.
Losing COBRA Benefits Here's the good news: Rolling off of COBRA coverage is a qualifying event that opens a special enrollment period for you to purchase your own health coverage. And you'll have more options, flexibility and control of your health plan outside of COBRA with an individual health insurance plan.
D&R coverage ends when one of the following occurs: Your employment terminates. You transfer to an employer who does not participate in the D&R Plan. You change jobs with a Participating Employer and start working in an employee group that does not participate in the D&R Plan.