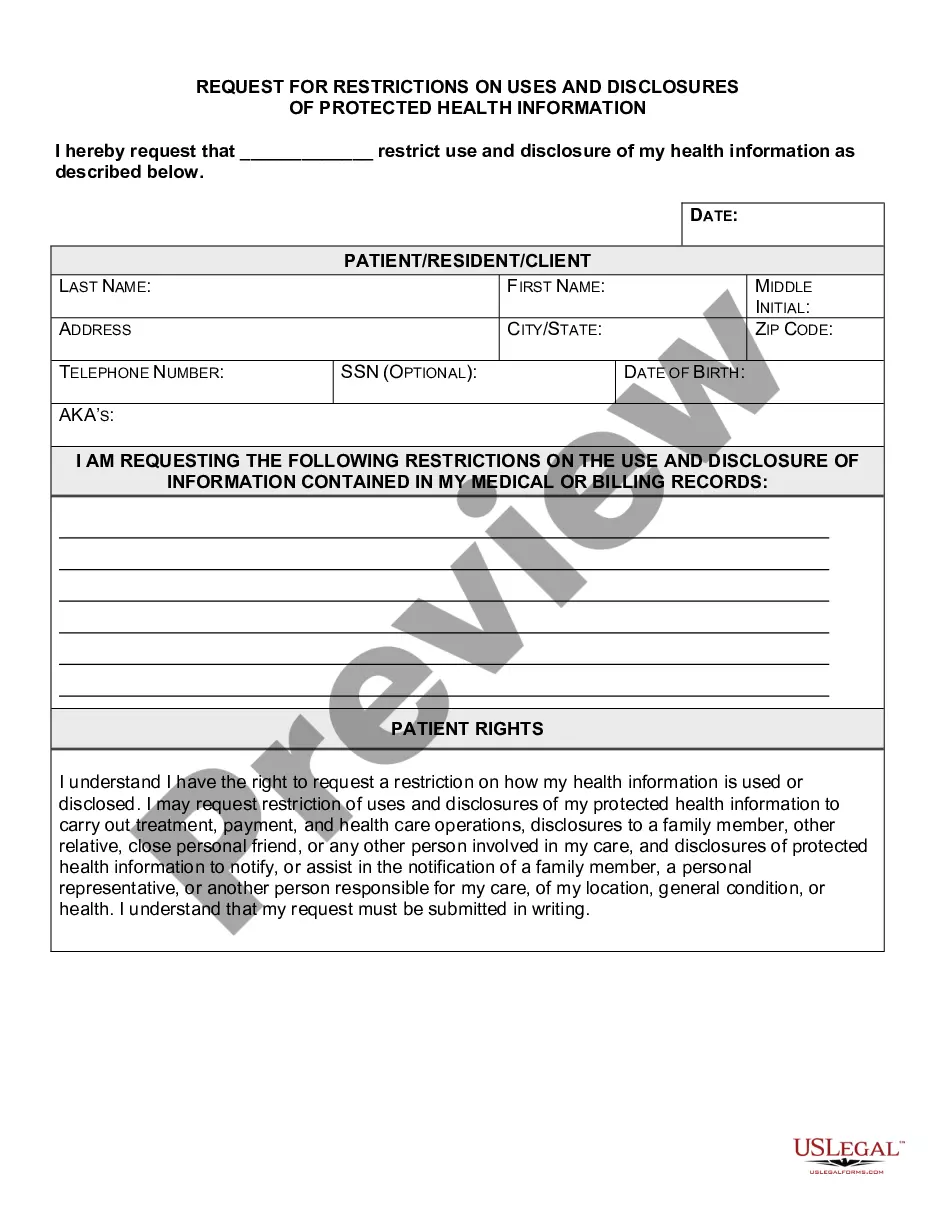
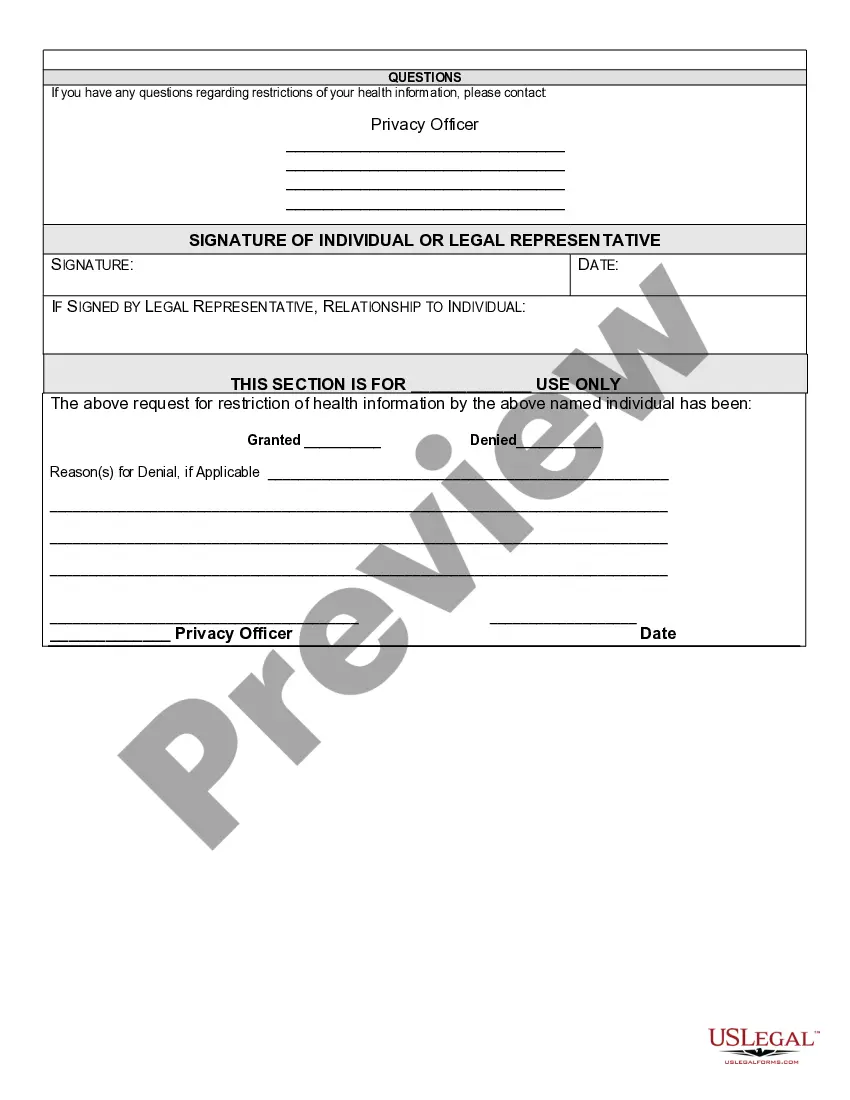
California Request for Restrictions on Uses and Disclosures of Protected Health Information
Description
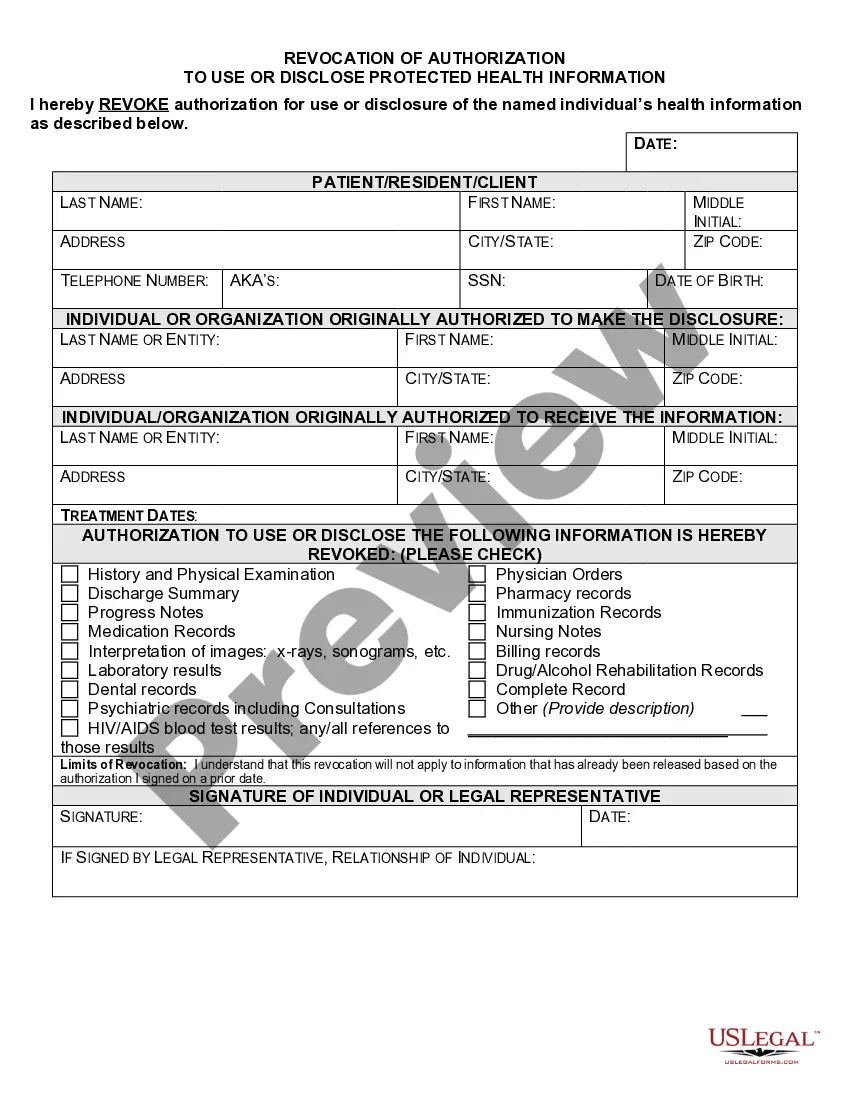
How to fill out Request For Restrictions On Uses And Disclosures Of Protected Health Information?
Finding the appropriate legal document template can be quite challenging. Clearly, there are numerous templates accessible online, but how can you locate the correct one you need? Utilize the US Legal Forms platform. This service offers thousands of templates, including the California Request for Restrictions on Uses and Disclosures of Protected Health Information, that can be utilized for both business and personal purposes. All forms are reviewed by experts and comply with state and federal regulations.
If you are already a registered user, Log In to your account and click on the Download button to retrieve the California Request for Restrictions on Uses and Disclosures of Protected Health Information. Use your account to search for the legal documents you have purchased in the past. Visit the My documents tab in your account to access another version of the document you need.
If you are a new user of US Legal Forms, here are simple instructions for you to follow: First, ensure you have selected the correct document for your city/state. You can review the document using the Review button and read the document details to confirm this is the right one for you. If the document does not meet your expectations, use the Search field to find the appropriate form.
- Once you are certain the document is accurate, click on the Get now button to obtain the form.
- Choose the pricing plan you prefer and provide the necessary information.
- Create your account and complete the payment for the order with your PayPal account or credit card.
- Select the file format and download the legal document template to your device.
- Complete, modify, print, and sign the obtained California Request for Restrictions on Uses and Disclosures of Protected Health Information.
- US Legal Forms is the largest repository of legal documents where you can find a variety of document templates. Take advantage of this service to obtain professionally crafted paperwork that adheres to state regulations.
Form popularity
FAQ
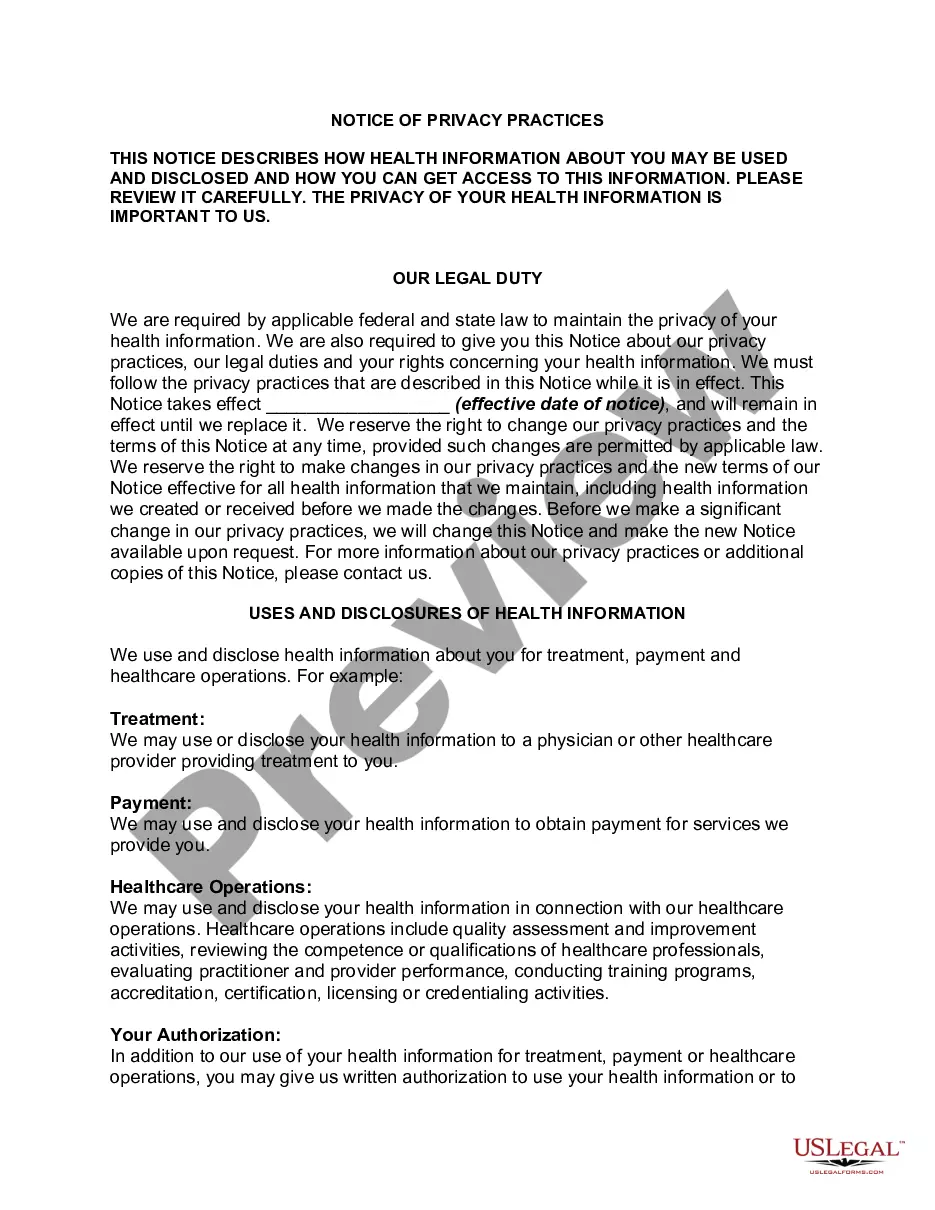
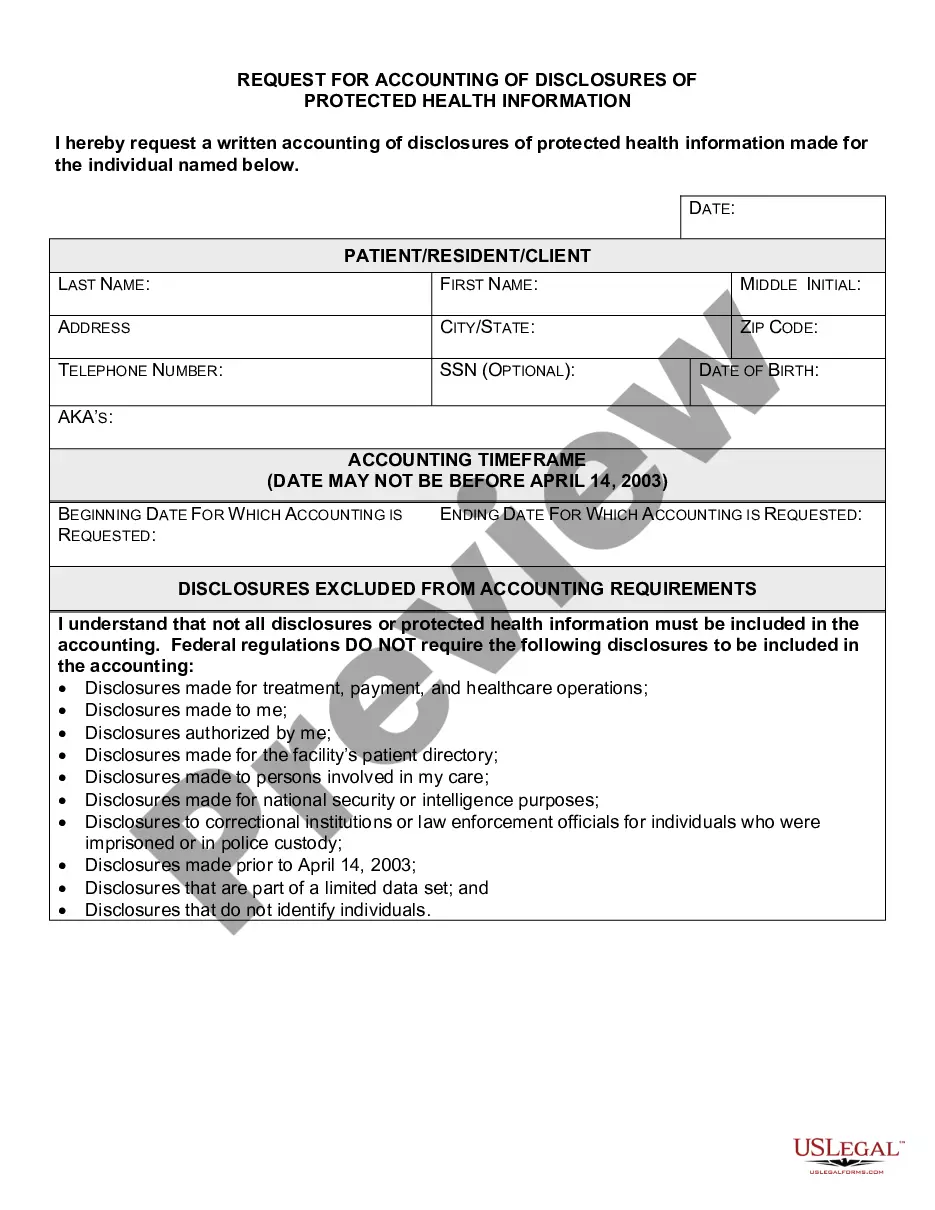
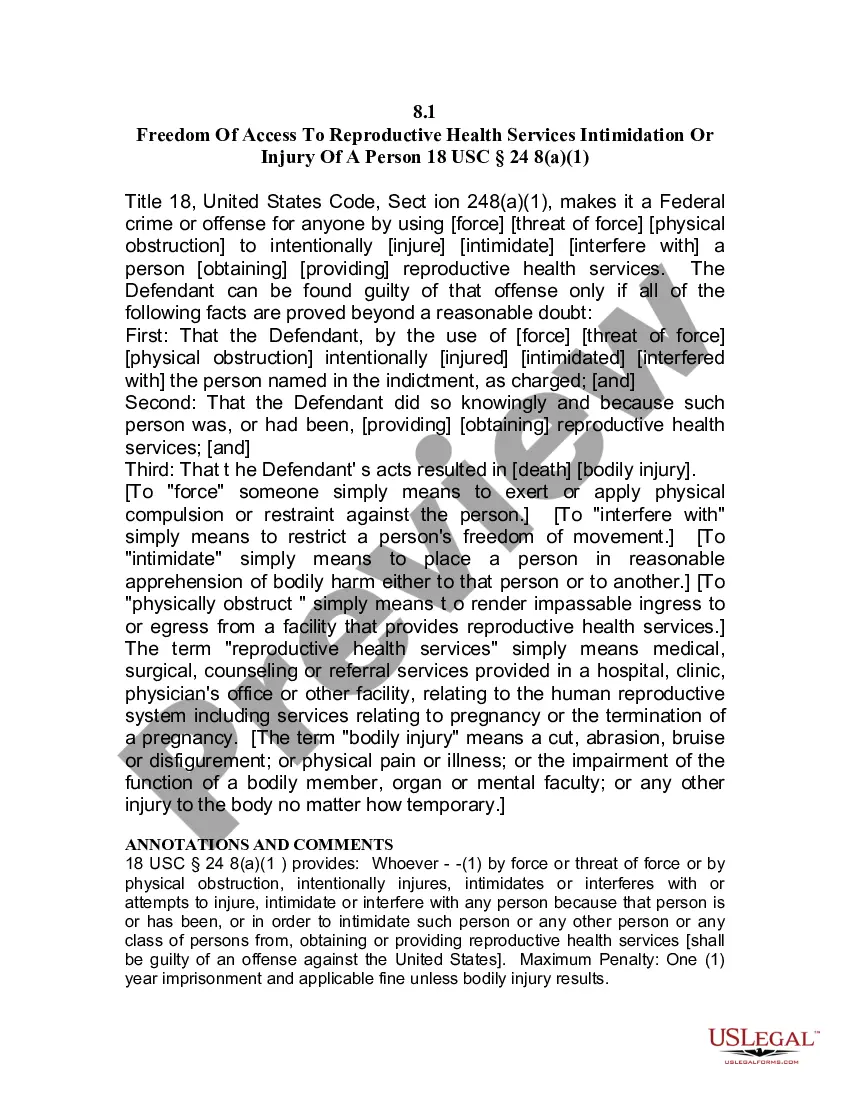
The California Request for Restrictions on Uses and Disclosures of Protected Health Information provides clear guidelines on handling inappropriate disclosures. Typically, if an unauthorized release occurs, it may result in legal repercussions, including fines or disciplinary actions against the offending party. It is crucial to have a thorough understanding of these guidelines to safeguard both patient data and your practice.
There are a few scenarios where you can disclose PHI without patient consent: coroner's investigations, court litigation, reporting communicable diseases to a public health department, and reporting gunshot and knife wounds.
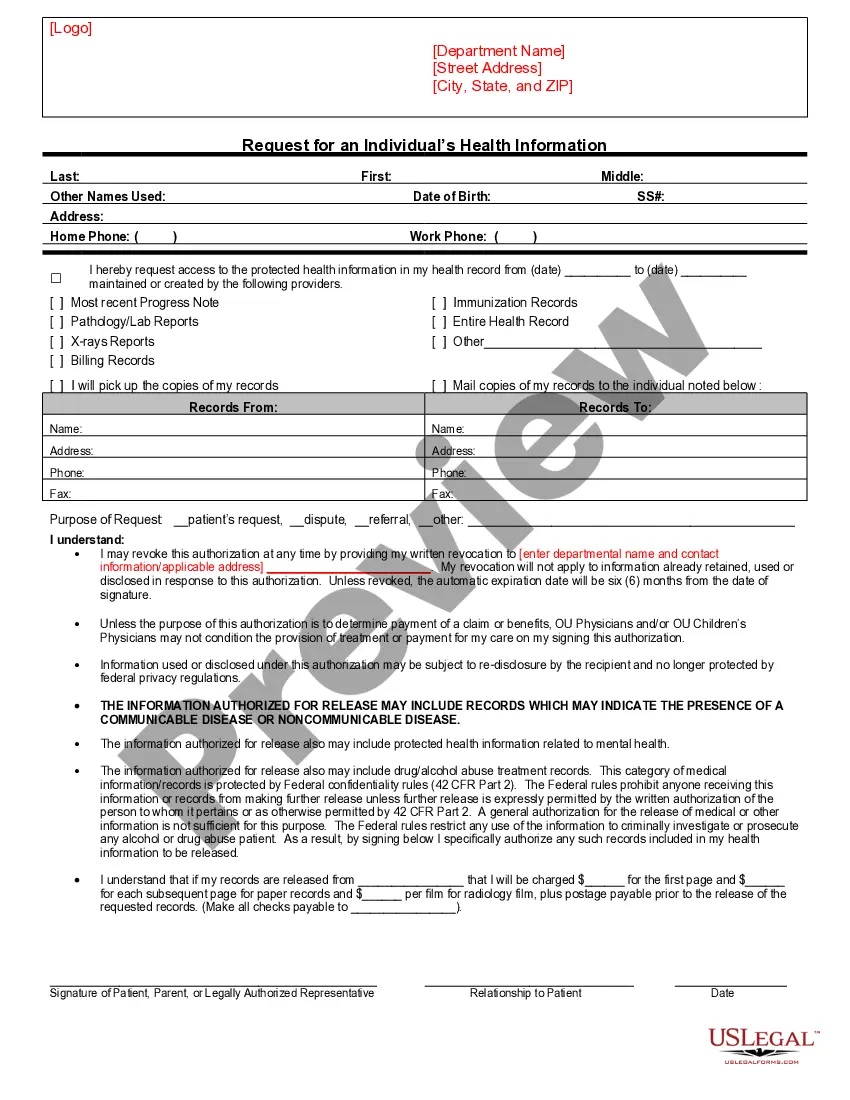
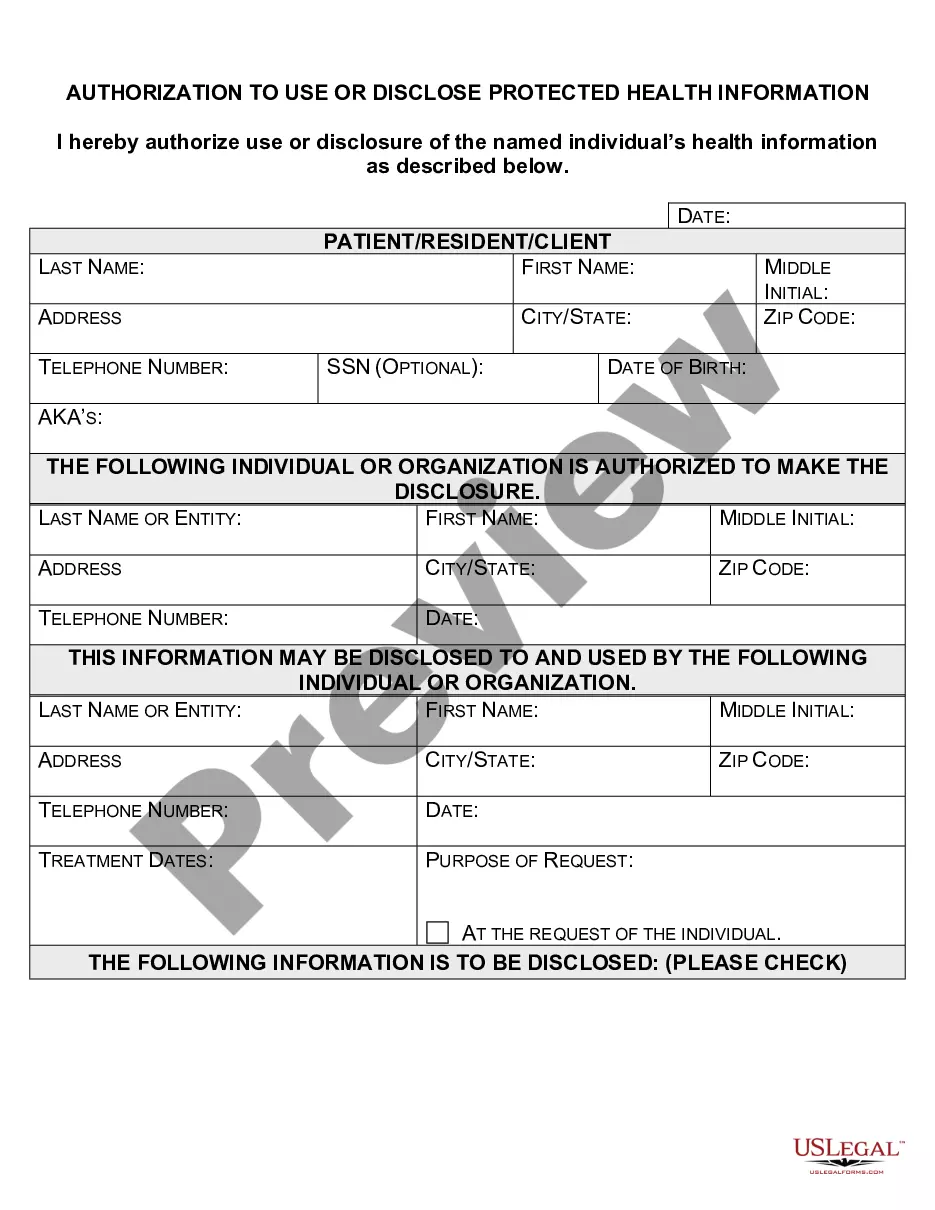
Under the new rule, individuals now have a right to obtain restrictions on the disclosure of health information (protected health information or PHI) in electronic or any other form to a health plan for payment or healthcare operations with respect to specific items and services for which the individual has paid the
Covered entities may disclose protected health information that they believe is necessary to prevent or lessen a serious and imminent threat to a person or the public, when such disclosure is made to someone they believe can prevent or lessen the threat (including the target of the threat).
A covered entity is required to agree to an individual's request to restrict the disclosure of their PHI to a health plan when both of the following conditions are met: (1) the disclosure is for payment or health care operations and is not otherwise required by law; and (2) the PHI pertains solely to a health care item
A covered entity such as a doctor must agree to an individual's request to restrict disclosure of her PHI to a health plan if: the disclosure is for the purpose of carrying out payment or health care operations and is not required by law; and.
Under the new rule, individuals now have a right to obtain restrictions on the disclosure of health information (protected health information or PHI) in electronic or any other form to a health plan for payment or healthcare operations with respect to specific items and services for which the individual has paid the
Yes, but only within specific limits. The Privacy Rule permits a covered entity to impose a reasonable, cost-based fee to provide the individual (or the individual's personal representative) with a copy of the individual's PHI, or to direct the copy to a designated third party.
What is a patient required to do in order for a request to restrict the use or disclosure of their PHI to their health plan to be granted? The Privacy Rule allows for a patient to request that no information be shared with others even to the point of not acknowledging the patient's presence in the covered entity.
If a covered entity denies access, in whole or in part, to PHI requested by the individual based on one or more permitted grounds, the covered entity must provide a denial in writing to the individual no later than 30 calendar days after the request (or no more than 60 calendar days if the covered entity notified the