California Certificate of Group Health Plan Coverage
Description
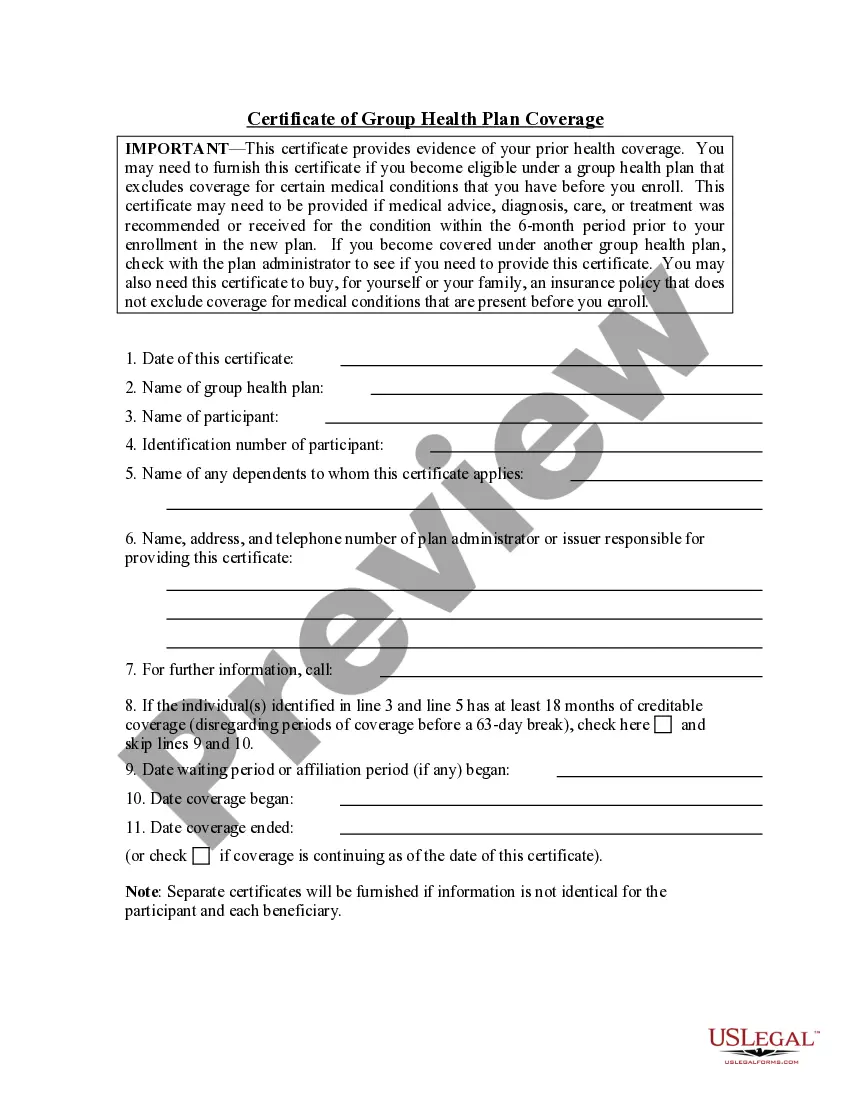
How to fill out Certificate Of Group Health Plan Coverage?
US Legal Forms - among the biggest libraries of authorized kinds in America - gives a wide array of authorized document web templates you are able to download or print out. Utilizing the web site, you can get thousands of kinds for company and person uses, categorized by groups, claims, or keywords and phrases.You can get the latest types of kinds like the California Certificate of Group Health Plan Coverage in seconds.
If you currently have a monthly subscription, log in and download California Certificate of Group Health Plan Coverage from the US Legal Forms collection. The Obtain switch can look on every single kind you look at. You get access to all previously delivered electronically kinds within the My Forms tab of the profile.
If you want to use US Legal Forms initially, here are basic instructions to help you started:
- Ensure you have chosen the best kind for your town/area. Go through the Review switch to examine the form`s information. Read the kind outline to actually have chosen the proper kind.
- When the kind doesn`t suit your demands, use the Look for field towards the top of the screen to find the one who does.
- When you are satisfied with the shape, confirm your option by clicking the Purchase now switch. Then, select the costs strategy you want and give your accreditations to sign up on an profile.
- Procedure the transaction. Utilize your charge card or PayPal profile to finish the transaction.
- Select the formatting and download the shape on the gadget.
- Make changes. Load, revise and print out and indicator the delivered electronically California Certificate of Group Health Plan Coverage.
Every template you included with your account lacks an expiry particular date and is also yours forever. So, if you want to download or print out yet another copy, just visit the My Forms section and click on around the kind you will need.
Get access to the California Certificate of Group Health Plan Coverage with US Legal Forms, one of the most substantial collection of authorized document web templates. Use thousands of skilled and condition-particular web templates that fulfill your company or person requires and demands.
Form popularity
FAQ
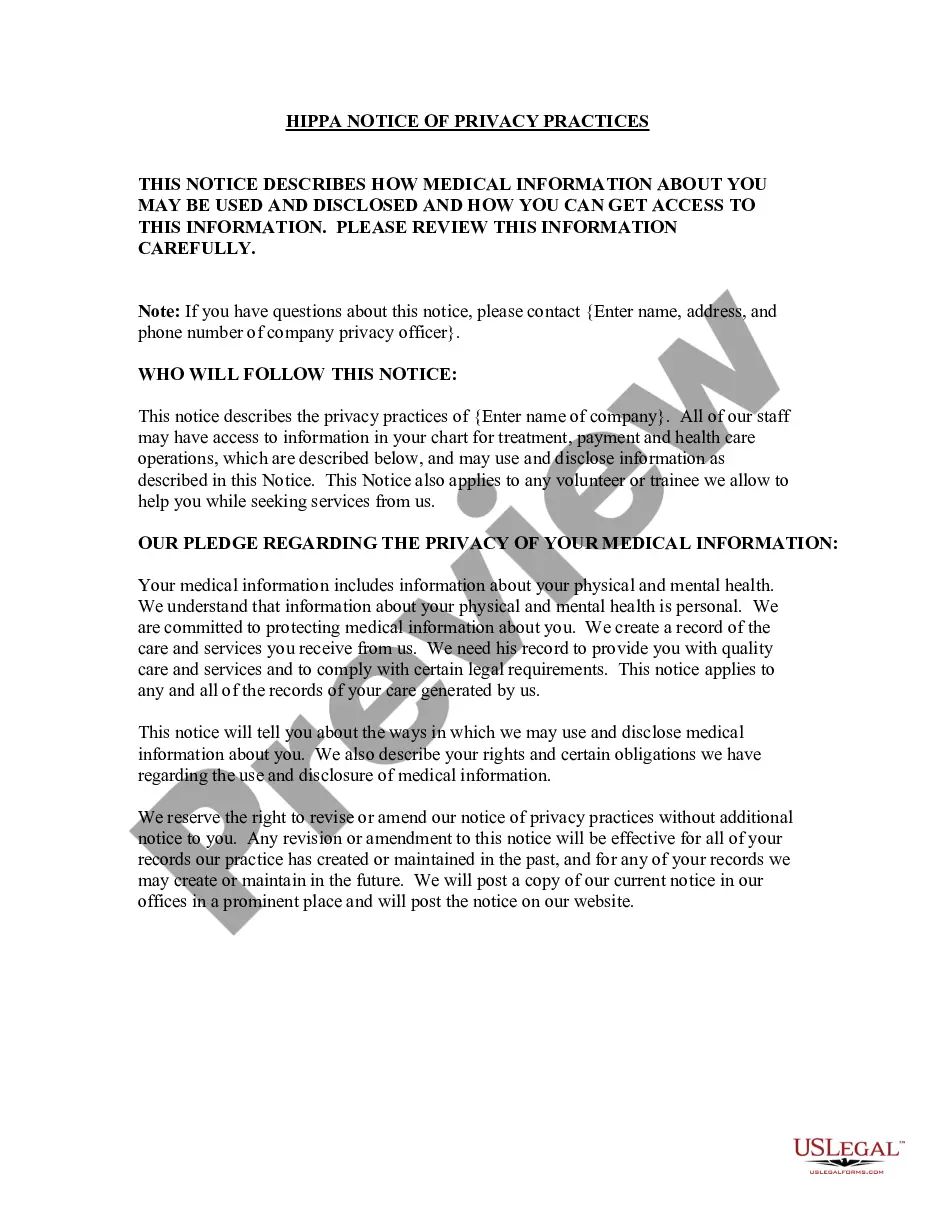
A certificate of coverage (CoC) is a contract that lists an individual's health insurance coverage with their payor.
The Differences Cal-COBRA applies to employers with 2-19 employees, whereas federal COBRA applies to employers with more than 20 employees. Cal-COBRA offers coverage for up to 36 months, while federal COBRA offers coverage for 18 months for the former employee and up to 36 months for any dependents.
Form FTB 3853 Health Coverage Exemptions and Individual Shared Responsibility Penalty Select the tax year in which you need information. Enter your ZIP code (and county, if prompted) Enter your total household income for the tax filing year. Enter the number of people in your tax household.
California law requires that insurers and HMOs provide continuation coverage known as Cal-COBRA.
How to get COBRA coverage. When a qualifying life event happens, you or your employer will notify the health plan. The plan will send an election notice that you will have 60 days to respond to. If you elect to take COBRA coverage, your employer may pay a portion of or the full amount of your insurance premium.
You will get a Form 1095-B for your Medi-Cal coverage from DHCS and you will also get a Form 1095?A from Covered California. Each form will show the months of coverage that met the requirement for MEC for any months of coverage you got from either Medi?Cal or Covered California.
Employers should send notices by first-class mail, obtain a certificate of mailing from the post office, and keep a log of letters sent. Certified mailing should be avoided, as a returned receipt with no delivery acceptance signature proves the participant did not receive the required notice.
Cal-COBRA administration requires four basic compliance components: Notifying all eligible group health care participants of their Cal-COBRA rights. Providing timely notice of Cal-COBRA eligibility, enrollment forms, and notice of the duration of coverage and terms of payment after a qualifying event has occurred.