California COBRA Continuation Coverage Election Form
Description
How to fill out COBRA Continuation Coverage Election Form?
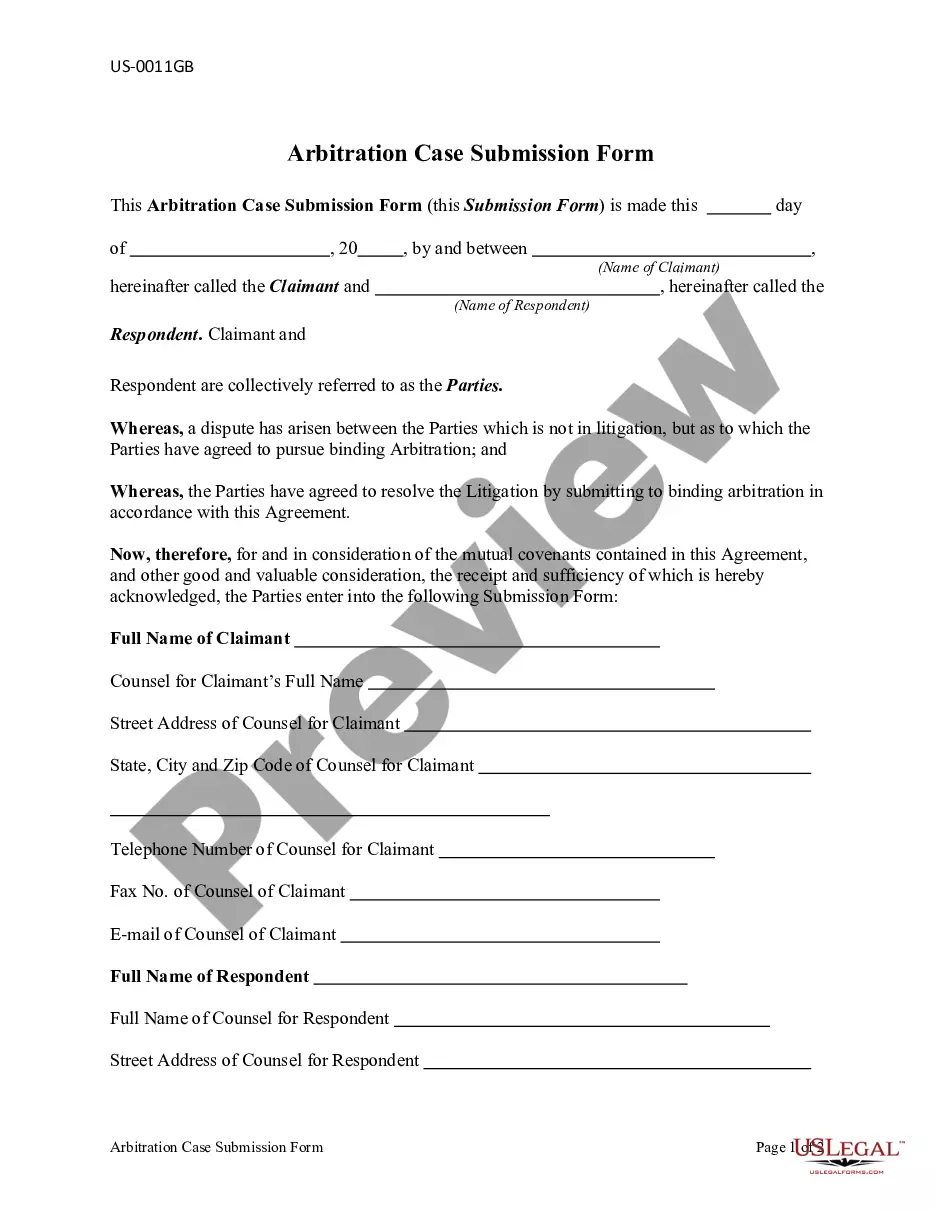
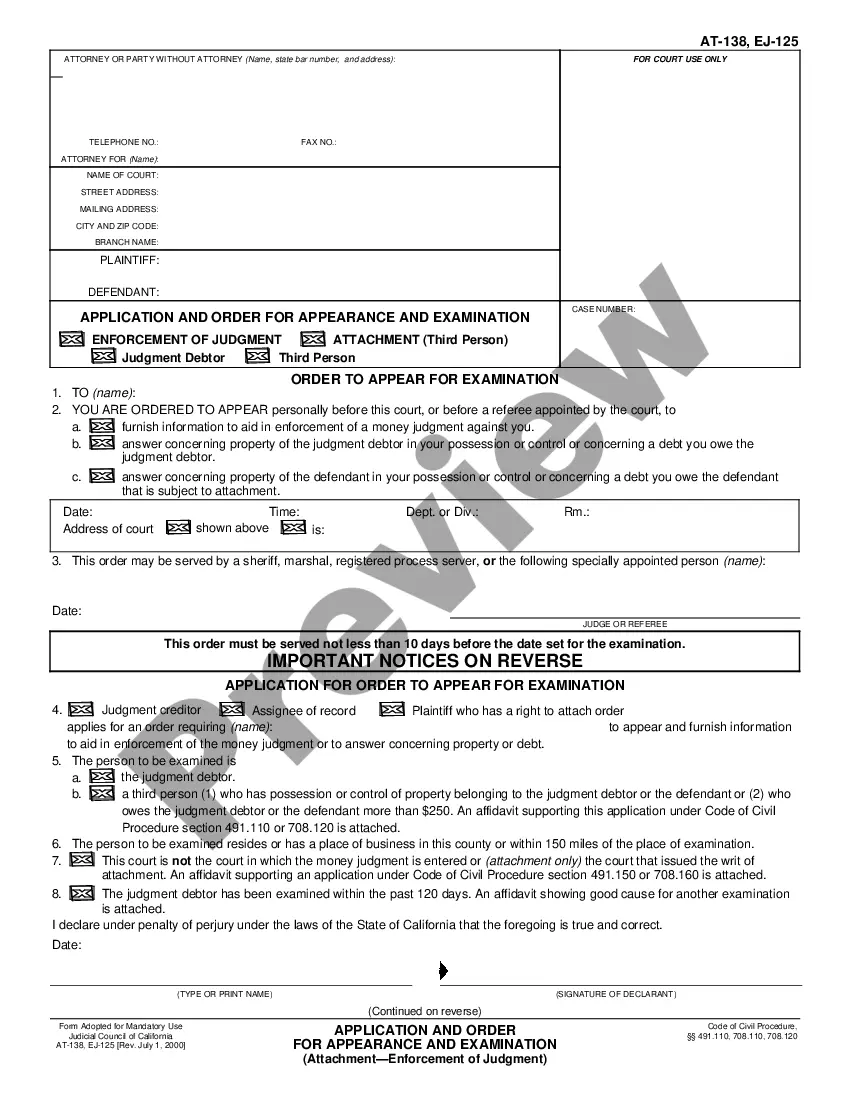
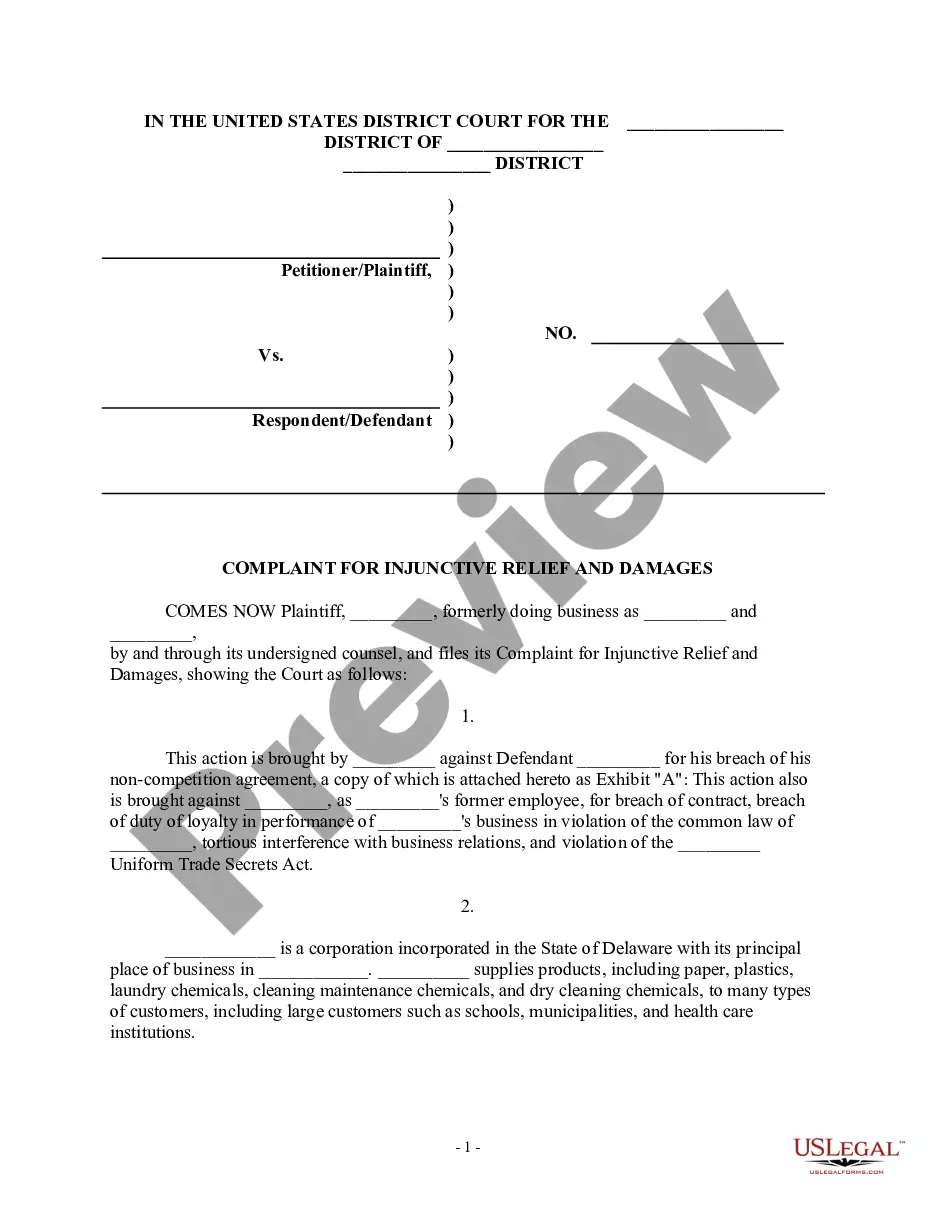
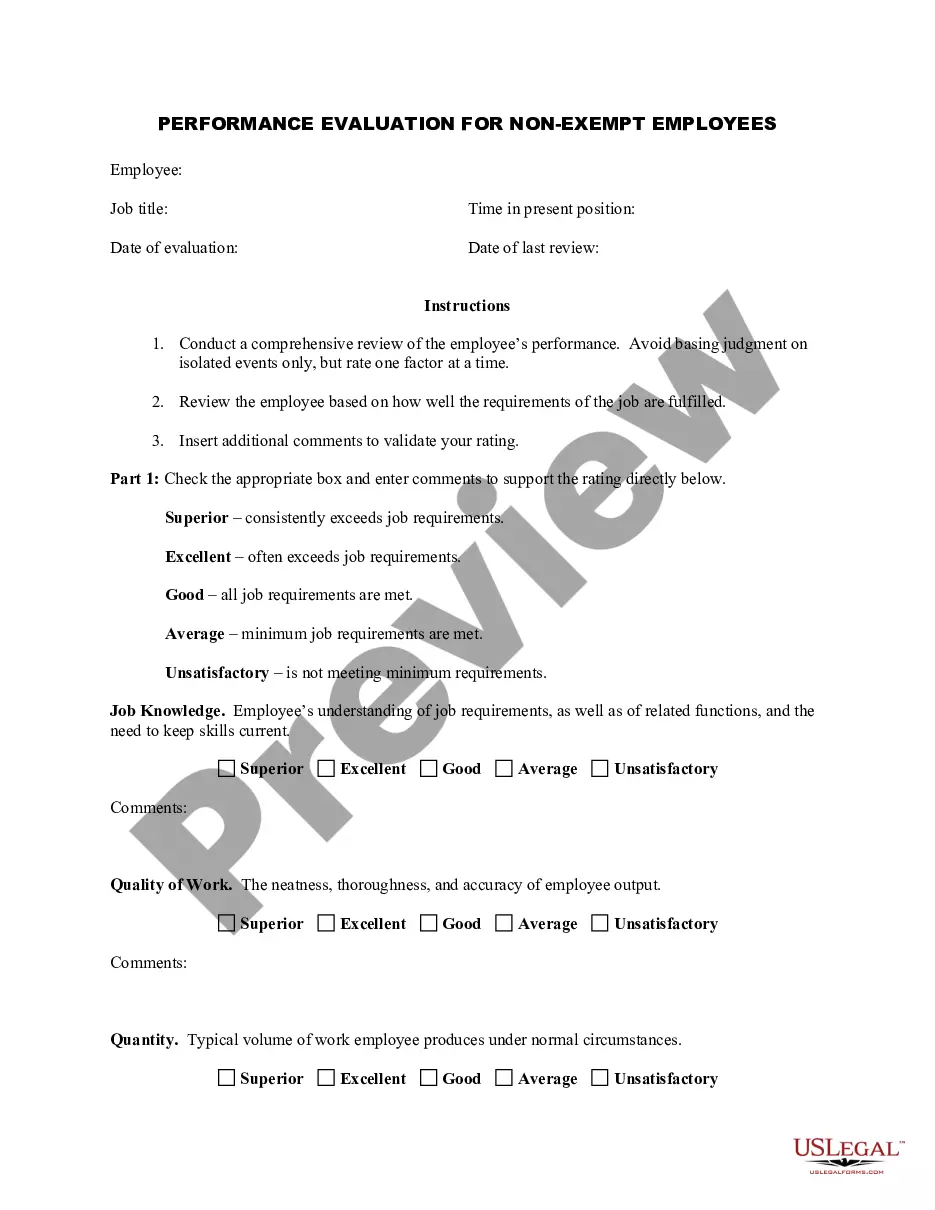
It is feasible to spend hours online searching for the authentic document template that complies with the state and federal requirements you need.
US Legal Forms provides a vast array of official forms that can be evaluated by experts.
You can easily download or print the California COBRA Continuation Coverage Election Form from my service.
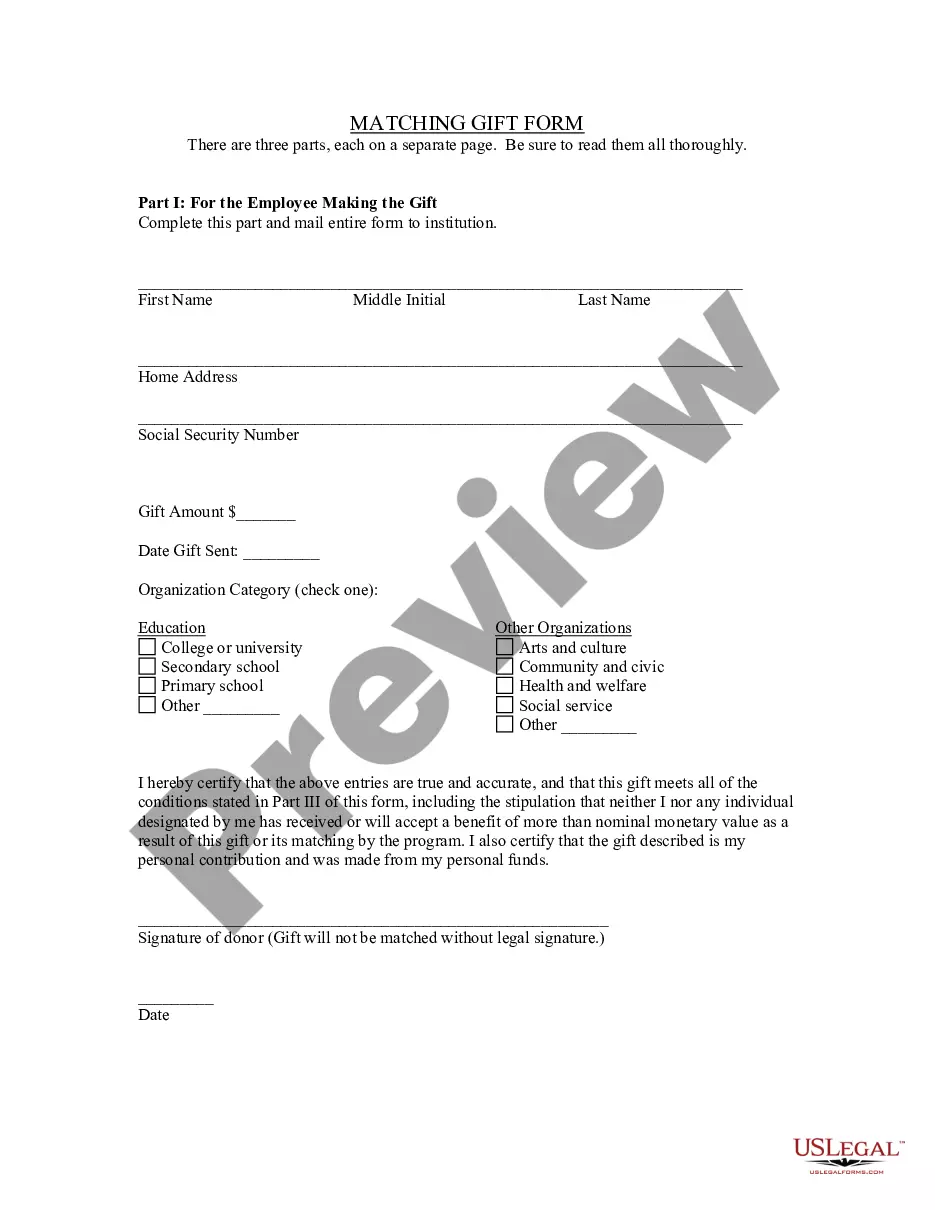
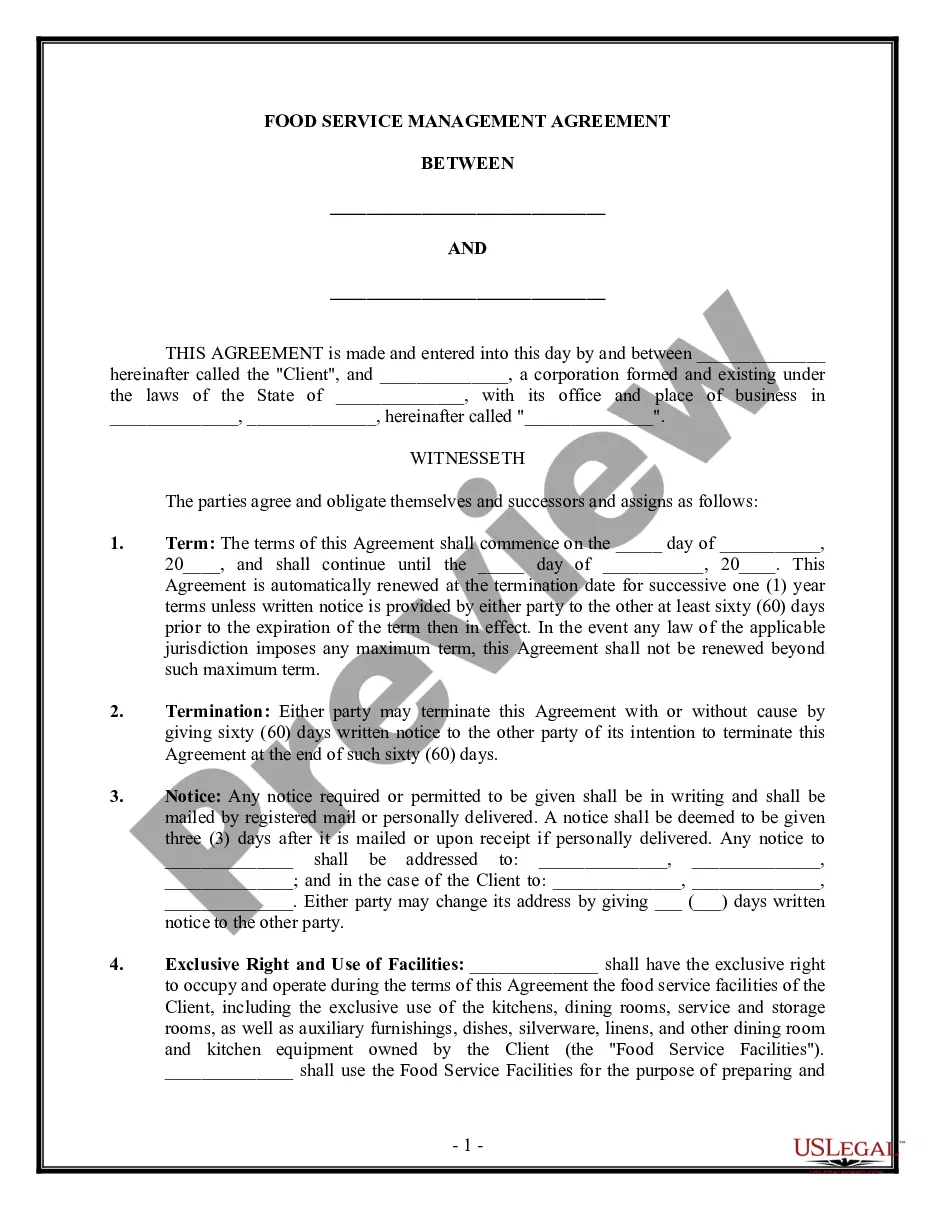
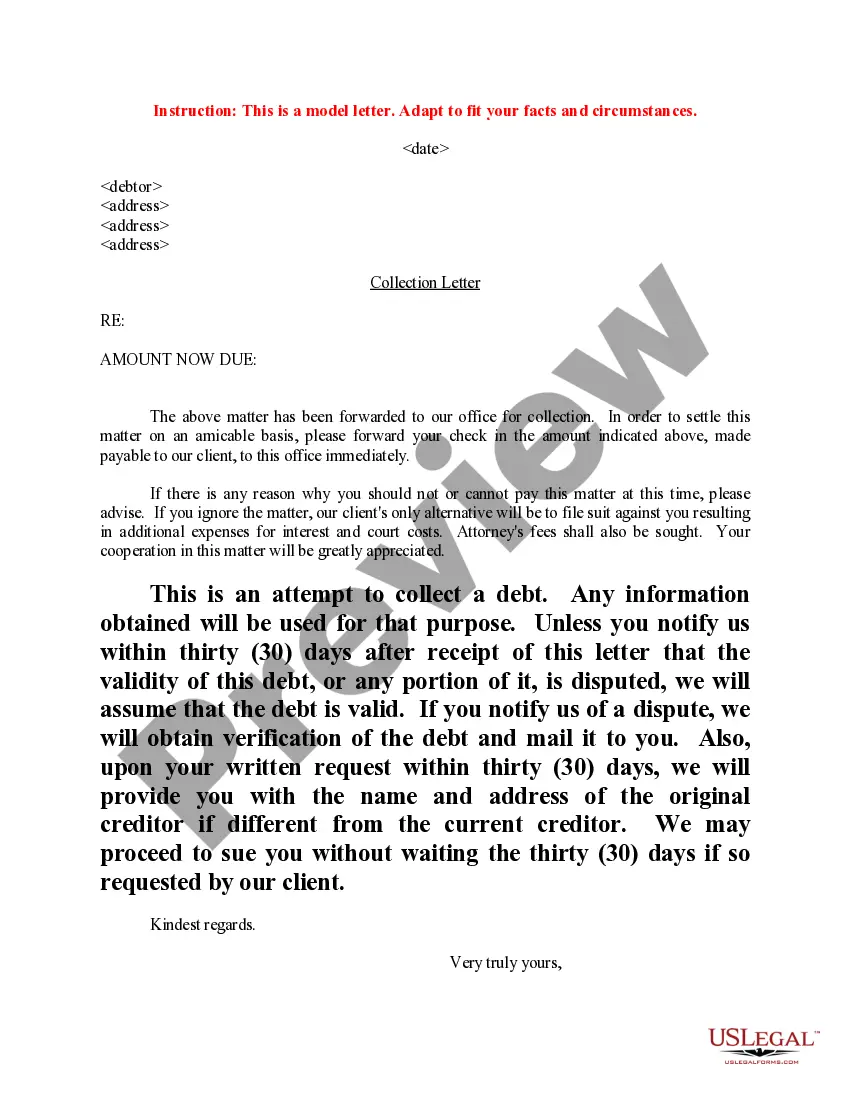
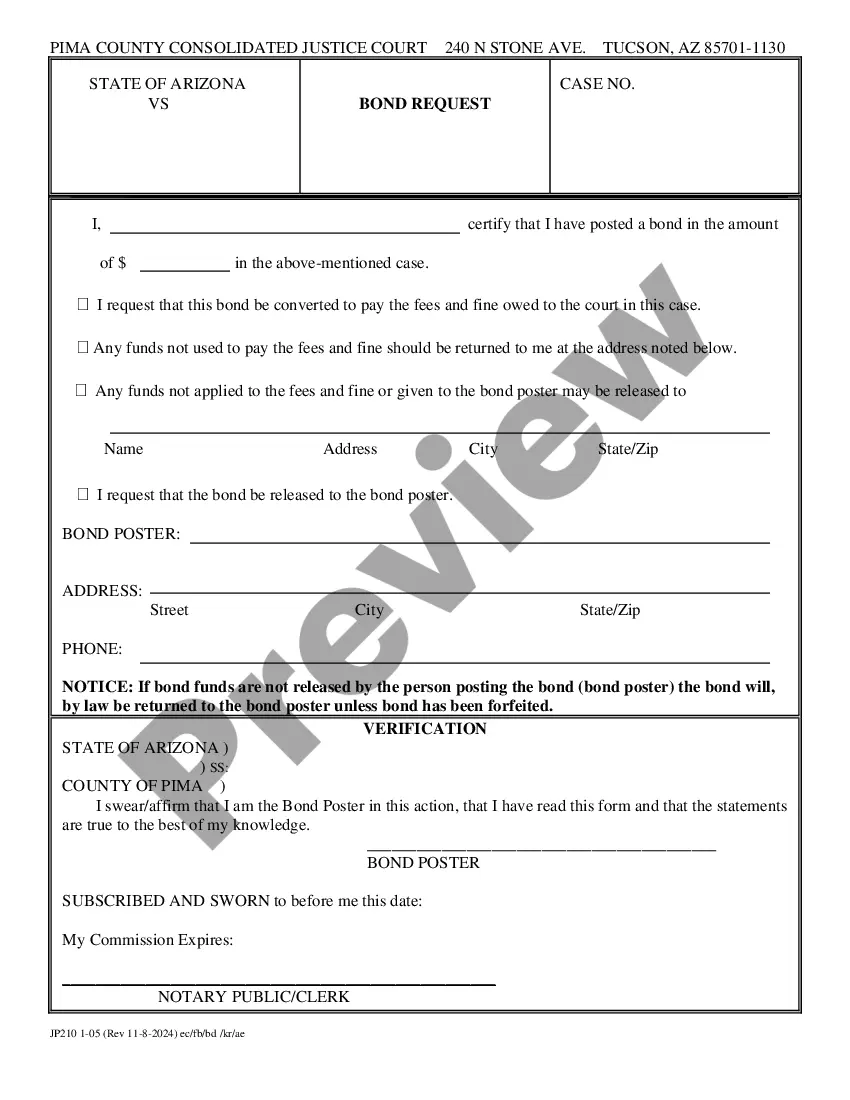
If available, use the Review button to inspect the document template as well.
- If you already have a US Legal Forms account, you can Log In and click the Download button.
- Then you can fill out, modify, print, or sign the California COBRA Continuation Coverage Election Form.
- Every official document template you purchase is yours indefinitely.
- To obtain another copy of the acquired form, go to the My documents tab and click the relevant button.
- If this is your first time using the US Legal Forms website, follow the simple instructions provided below.
- First, ensure you have selected the appropriate document template for the state/city of your choice.
- Review the form description to confirm you have chosen the correct form.
Form popularity
FAQ
Key Takeaways. COBRA provides a good option for keeping your employer-sponsored health plan for a while after you leave your job. Although, the cost can be high. Make an informed choice by looking at all your options during the 60-day enrollment period, and don't focus on the premium alone.
The general notice describes general COBRA rights and employee obligations. This notice must be provided to each covered employee and each covered spouse of an employee who becomes covered under the plan. The notice must be provided within the first 90 days of coverage under the group health plan.
Cal-COBRA is a California Law that lets you keep your group health plan when your job ends or your hours are cut. It may also be available to people who have exhausted their Federal COBRA.
The extension period is 18 months and some people with special qualifying events may be eligible for a longer extension. To be eligible for COBRA, your group policy must be in force with 20 or more employees covered on more than 50 percent of its typical business days in the previous calendar year.
If you want to avoid paying the COBRA cost, go with a short-term plan if you're waiting for approval on another health plan. Choose a Marketplace or independent plan for broader coverage. Choose a high-deductible plan to keep your costs low.
Qualified beneficiaries must be given an election period of at least 60 days during which each qualified beneficiary may choose whether to elect COBRA coverage. This period is measured from the later of the date of the qualifying event or the date the COBRA election notice is provided.
COBRA the Consolidated Omnibus Budget Reconciliation Act -- requires group health plans to offer continuation coverage to covered employees, former employees, spouses, former spouses, and dependent children when group health coverage would otherwise be lost due to certain events.
Federal law requires that most group health plans (including this Plan) give employees and their families the opportunity to continue their health care coverage through COBRA continuation coverage when there's a qualifying event that would result in a loss of coverage under an employer's plan.