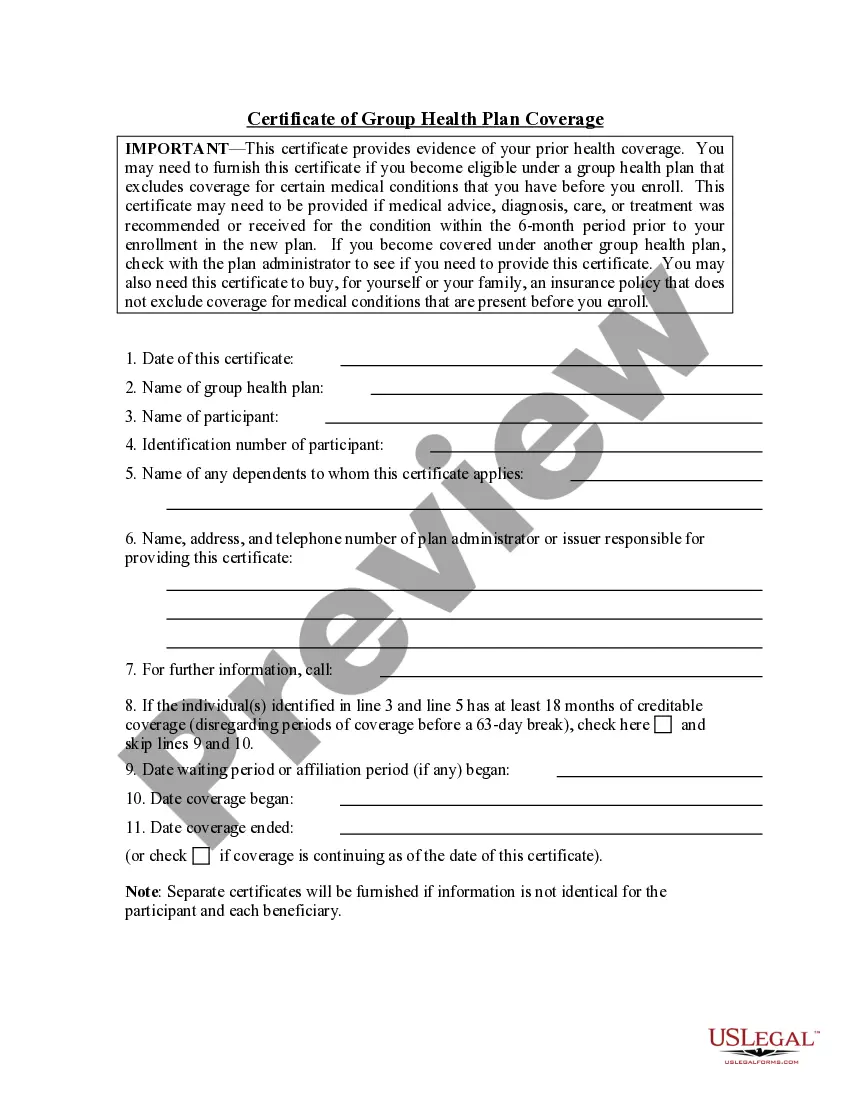
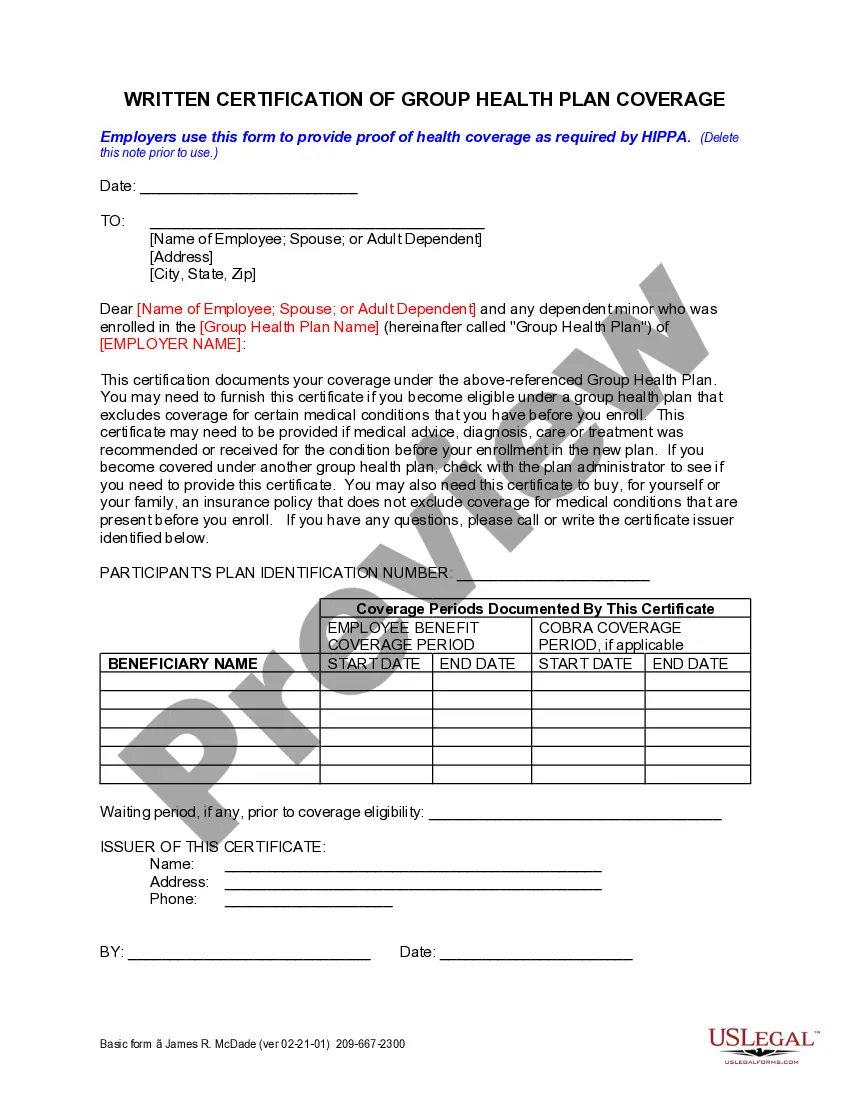
Employers use this form to provide proof to the employee of health coverage as required by HIPPA.
California Certification of Group Health Plan Coverage
Description
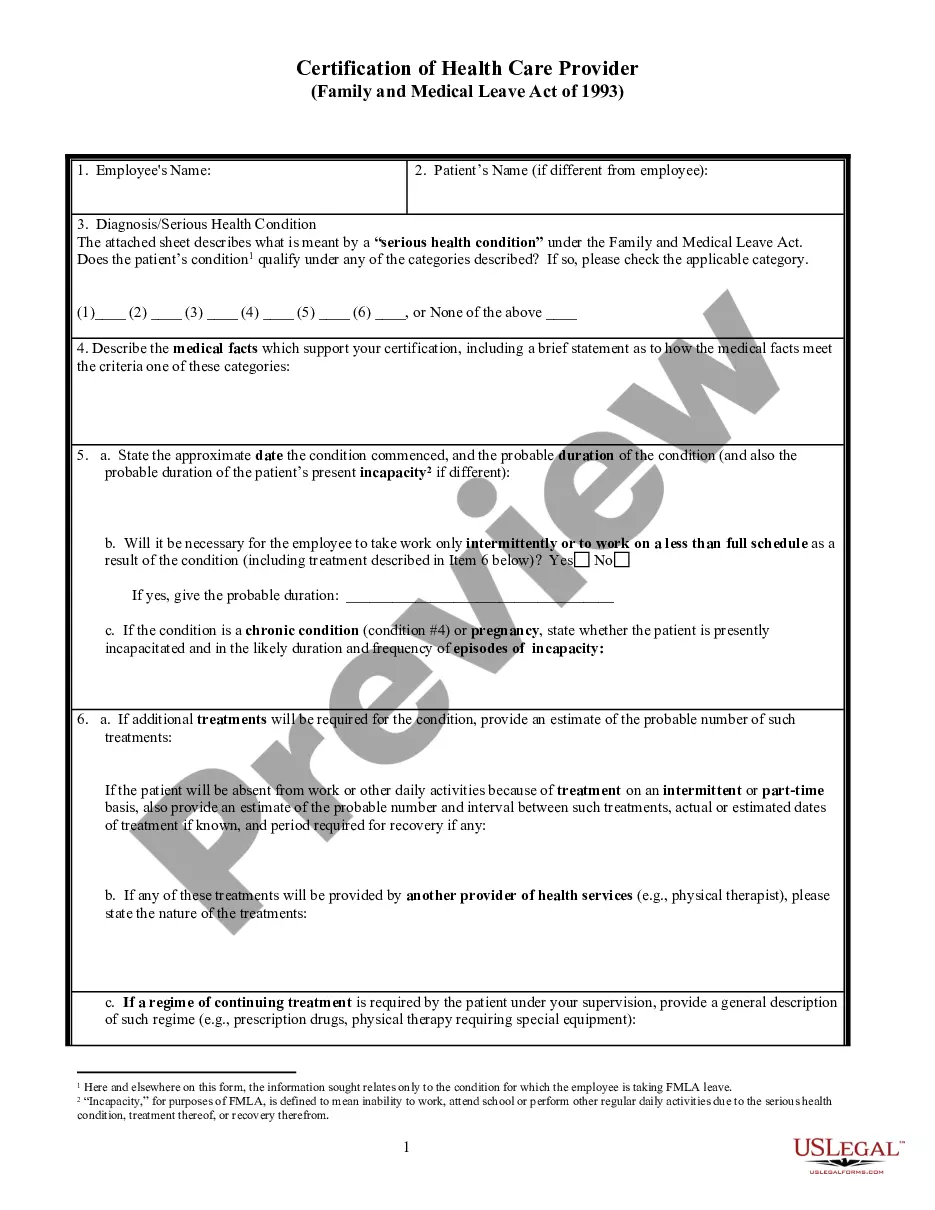
How to fill out California Certification Of Group Health Plan Coverage?
If you're looking for appropriate California Certification of Group Health Plan Coverage examples, US Legal Forms is exactly what you require; access documents crafted and verified by state-authorized attorneys.
Utilizing US Legal Forms not only saves you from frustrations related to legal documentation; you also save time, effort, and money!
And that's it. In just a few easy clicks, you have an editable California Certification of Group Health Plan Coverage. Once you create your account, all future orders will be processed even more effortlessly. If you possess a US Legal Forms subscription, simply Log In to your account and click the Download option available on the forms webpage. Then, when you need to use this template again, you'll always be able to find it in the My documents section. Don't waste your time searching through numerous forms across various web sources. Obtain precise documents from a single, secure platform!
- Initiate your registration process by providing your email and establishing a password.
- Follow the steps below to create your account and locate the California Certification of Group Health Plan Coverage template to address your needs.
- Use the Preview feature or read the file description (if provided) to ensure that the template is what you desire.
- Verify its applicability in your location.
- Click Buy Now to place your order.
- Choose a suitable pricing plan.
- Create an account and pay using your credit card or PayPal.
- Select an appropriate format and download the document.
Form popularity
FAQ
To obtain an insurance certificate, contact your insurance company or agent for assistance. They will likely require details about your coverage to issue the document. For specific needs related to the California Certification of Group Health Plan Coverage, consider using the US Legal Forms platform, which provides templates and guidance for common insurance forms.
To get a certificate of health insurance, reach out to your insurance provider and request the document. You may need to provide specific details regarding your policy or coverage. If you require the California Certification of Group Health Plan Coverage, ensure you specify this when making your request.
Form 3853 is typically required for individuals applying for premium tax credits under the Affordable Care Act related to their health insurance coverage. It's crucial for those who received premium assistance and need to report their enrollment. This process aligns with maintaining compliance with the California Certification of Group Health Plan Coverage.
A certificate of insurance in a group health plan serves as proof of coverage for group members. It outlines the specifics of the health plan, including benefits and eligibility. Obtaining this certificate is essential for demonstrating compliance with the California Certification of Group Health Plan Coverage requirements.
Covered California is not classified as a group health plan, but it offers individual and family health insurance options. However, it does help individuals access quality healthcare through various plans. If you're looking for group health plan coverage, you may still need to review options outside of Covered California for your specific requirements.
To obtain a health insurance certificate, first, contact your health insurance provider directly. They usually issue certificates upon request, and you may need to provide basic personal information. Additionally, consider exploring the California Certification of Group Health Plan Coverage, as it may meet your needs for official documentation.
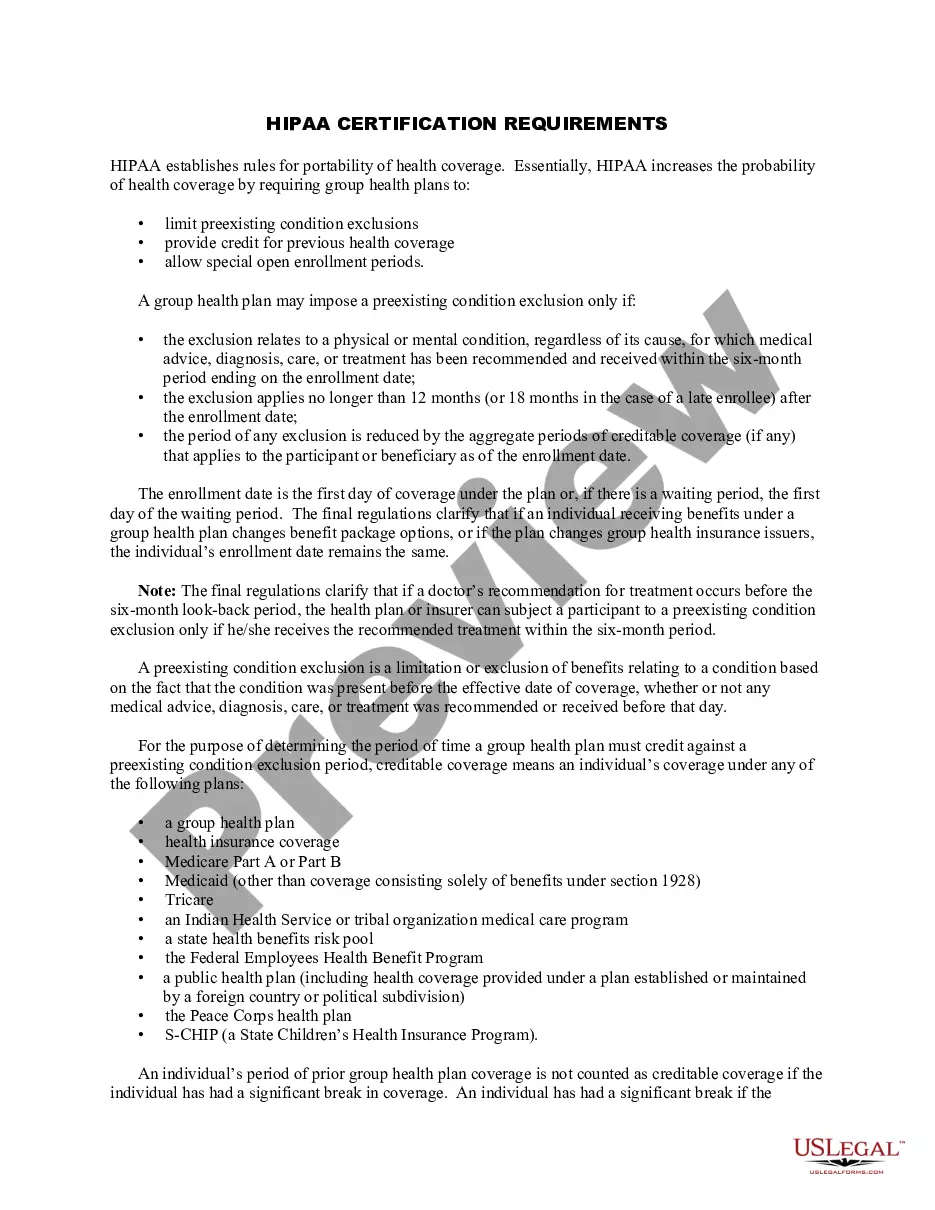
Yes, qualified health plans must be certified to ensure they meet both federal and state criteria for coverage. This process often includes the California Certification of Group Health Plan Coverage. By obtaining this certification, plans demonstrate their compliance and commitment to providing quality healthcare services.
Yes, all health insurance plans that are issued in the United States must comply with the Affordable Care Act regulations. This means they need to meet essential coverage standards, including those outlined in the California Certification of Group Health Plan Coverage. Understanding these requirements is vital for ensuring you have adequate protection.
A qualified group health plan is a type of insurance that meets essential health benefit requirements while complying with state and federal regulations. These plans must provide comprehensive coverage and undergo the California Certification of Group Health Plan Coverage to ensure compliance. As a consumer, you can benefit from protections afforded to these plans.
A qualified health plan is defined by its adherence to specific criteria set forth by the Affordable Care Act. This includes coverage for essential health benefits and consumer protections. Plans must also achieve the California Certification of Group Health Plan Coverage to be considered qualified in the state.