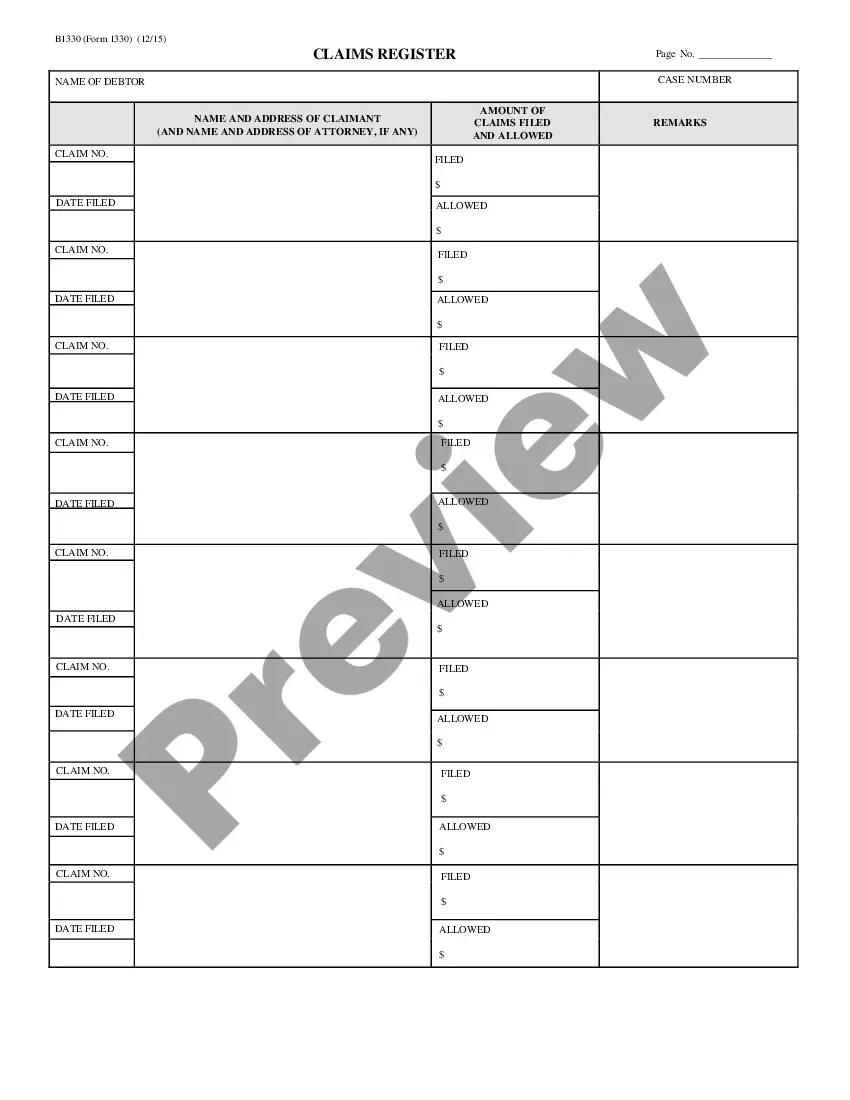
Arkansas Claims Register - B 133
Description
How to fill out Claims Register - B 133?
You are able to commit several hours on-line searching for the authorized file web template that fits the state and federal specifications you want. US Legal Forms offers thousands of authorized kinds that are analyzed by pros. You can actually download or print the Arkansas Claims Register - B 133 from my service.
If you already possess a US Legal Forms accounts, it is possible to log in and click on the Down load key. Following that, it is possible to complete, modify, print, or indication the Arkansas Claims Register - B 133. Every single authorized file web template you buy is your own property permanently. To have one more backup of any acquired form, go to the My Forms tab and click on the related key.
If you are using the US Legal Forms website initially, follow the simple instructions listed below:
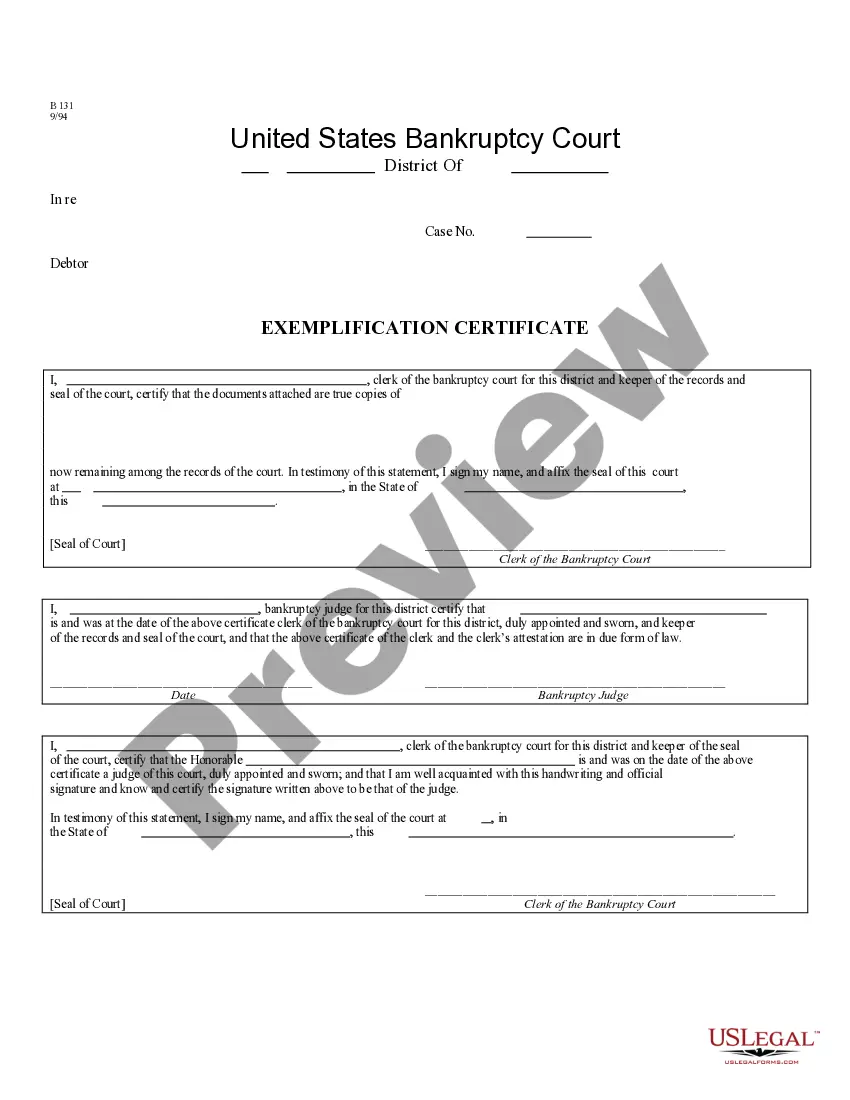
- Very first, ensure that you have selected the best file web template to the area/metropolis of your choice. Look at the form explanation to ensure you have chosen the proper form. If accessible, use the Review key to look with the file web template too.
- If you would like discover one more version in the form, use the Research field to discover the web template that fits your needs and specifications.
- Upon having found the web template you desire, click Acquire now to continue.
- Pick the prices plan you desire, enter your accreditations, and sign up for a free account on US Legal Forms.
- Total the transaction. You should use your Visa or Mastercard or PayPal accounts to purchase the authorized form.
- Pick the formatting in the file and download it to your system.
- Make changes to your file if needed. You are able to complete, modify and indication and print Arkansas Claims Register - B 133.
Down load and print thousands of file themes using the US Legal Forms web site, which provides the most important selection of authorized kinds. Use expert and condition-certain themes to take on your organization or person needs.
Form popularity
FAQ
Denial Code CO 97 occurs because the benefit for a service in the allowance/payment for another service that was already adjudicated. In simpler terms, the service or procedure is not paid for individually. One example is when a provider bills a procedure code that is inclusive with another procedure code.
-GY ? Item or service statutorily excluded, does not meet the definition of any Medicare benefit or for non-Medicare insurers, and is not a contract benefit. If you do not provide the beneficiary with notice that the services are excluded from coverage, you should append modifier -GY to the line item.
Medicaid and ARKids First will pay for pelvic exams, pap tests, and mammograms for all ages. You can go to your PCP for these services, or you can go to a gynecologist (a women's health specialist). No referral is needed for these services.
CO-167 ? Diagnosis is Not Covered: Health insurance plans don't cover all diagnoses. The payer will use denial code CO 167 when they do not cover the diagnosis or diagnoses. If you face this denial code, review the diagnosis codes reported in the claim.
CO 109 denial code indicates that the claim was rejected due to coordination of benefits (COB) issues. Coordination of benefits refers to situations where a patient is covered by multiple insurance policies, and the primary and secondary insurers have not coordinated their payment responsibilities appropriately.
241 Low Income Subsidy (LIS) Co-payment Amount 242 Services not provided by network/primary care providers. 243 Services not authorized by network/primary care providers.
Group Codes assign financial responsibility for the unpaid portion of the claim balance e.g., CO (Contractual Obligation) assigns responsibility to the provider and PR (Patient Responsibility) assigns responsibility to the patient. Medicare beneficiaries may be billed only when Group Code PR is used with an adjustment.
CO 22 ? Payment adjusted because this care may be covered by another payer per coordination of benefits. This denial indicates that the Medicare carrier has information that the patient has insurance that is primary to Medicare, such as through employment of the patient or spouse.