Arkansas Qualifying Event Notice Information for Employer to Plan Administrator
Description
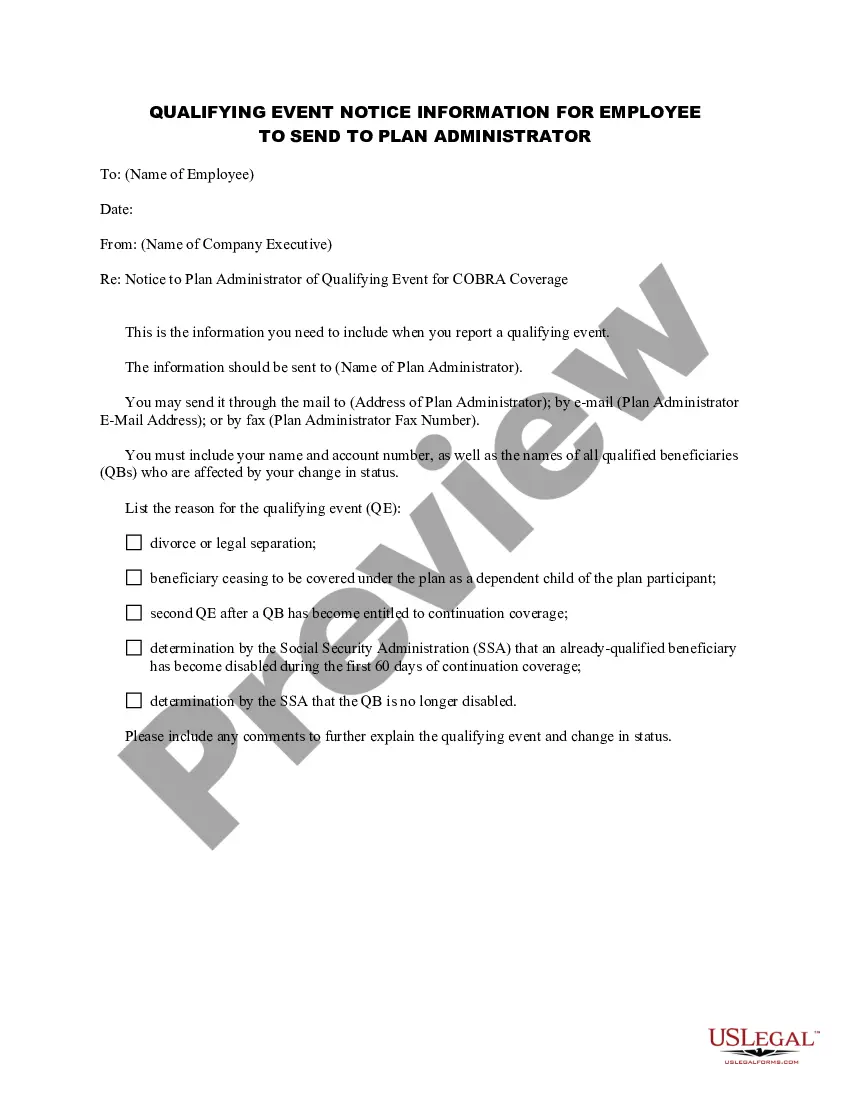
How to fill out Qualifying Event Notice Information For Employer To Plan Administrator?
Have you ever found yourself in a situation where you need documentation for either business or personal purposes almost every day.
There are numerous legal document templates accessible on the web, but pinpointing trustworthy versions can be challenging.
US Legal Forms offers thousands of form templates, including the Arkansas Qualifying Event Notice Information for Employer to Plan Administrator, specifically designed to comply with federal and state regulations.
You can find all the document templates you have purchased in the My documents section.
You can obtain an additional copy of the Arkansas Qualifying Event Notice Information for Employer to Plan Administrator at any time if needed. Just click on the required form to download or print the document template.
- If you are already familiar with the US Legal Forms website and have an account, simply Log In.
- Then, you can download the Arkansas Qualifying Event Notice Information for Employer to Plan Administrator template.
- If you don't have an account and wish to start using US Legal Forms, follow these steps.
- Obtain the form you need and ensure it corresponds to the correct region/area.
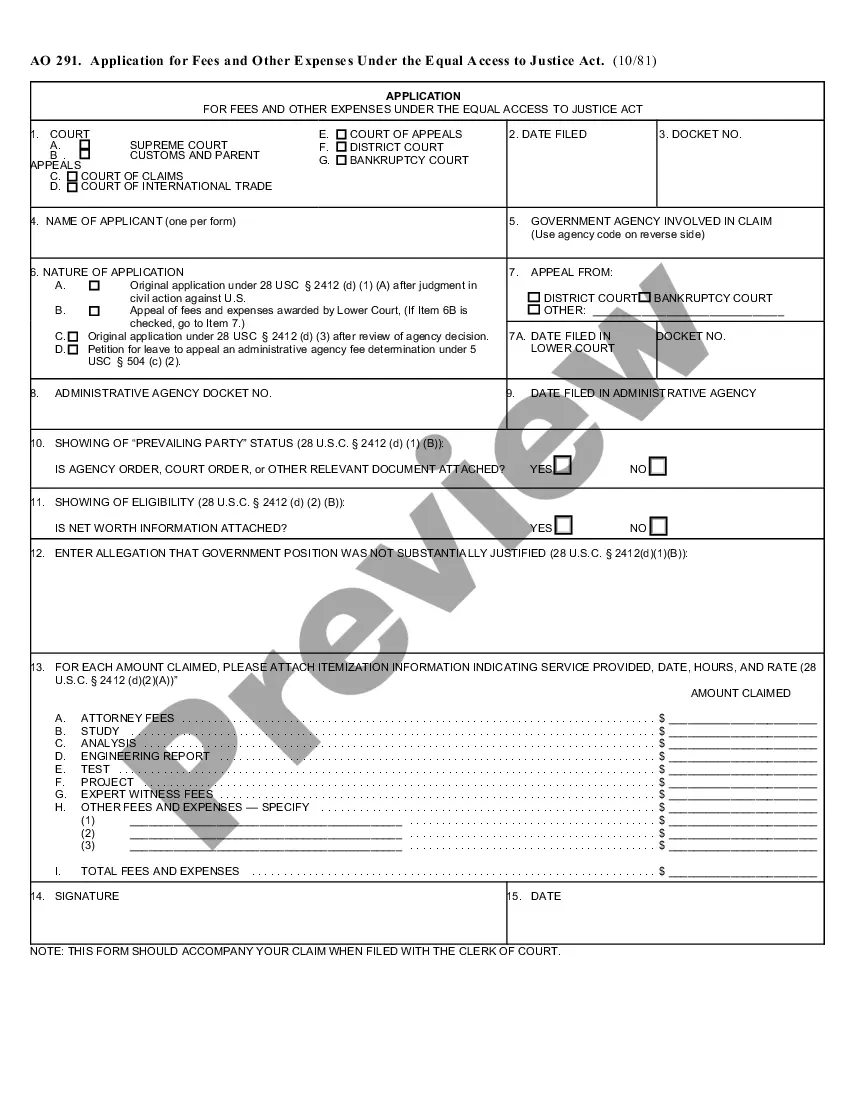
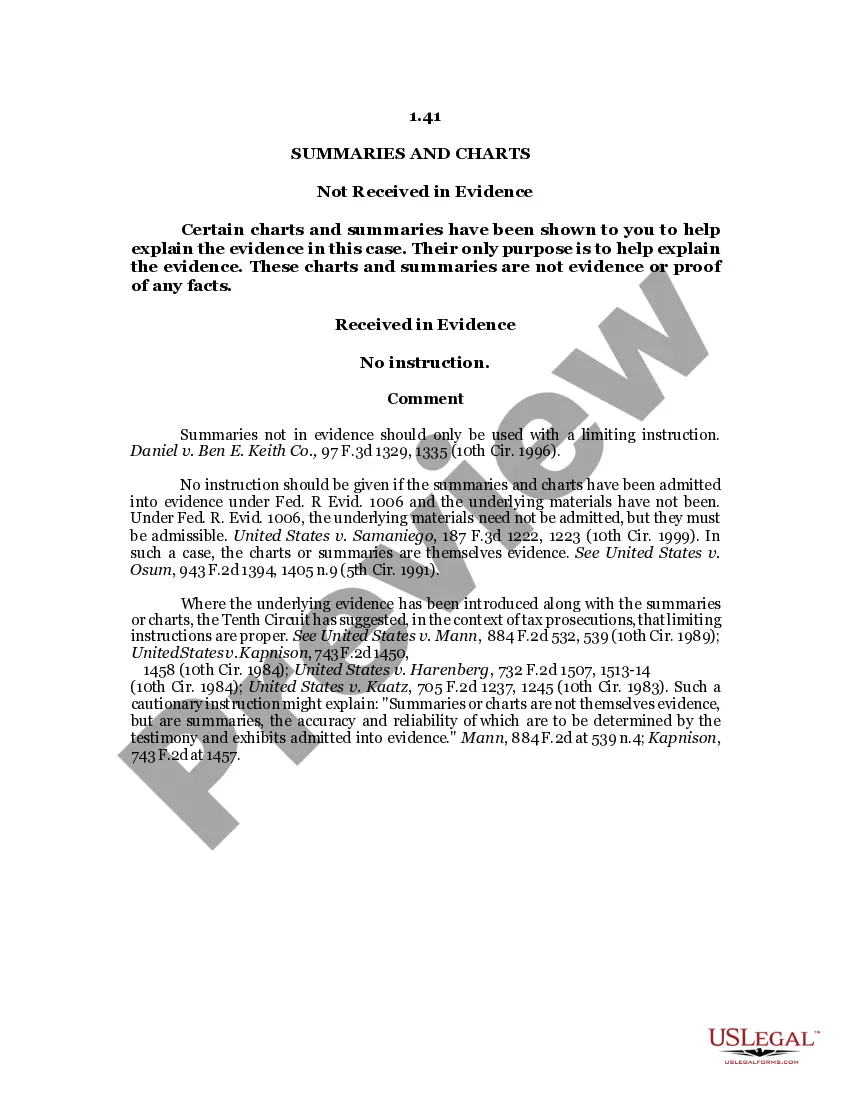
- Use the Review option to examine the form.
- Check the details to make sure you have selected the correct form.
- If the form is not what you're looking for, utilize the Search field to find the form that suits your needs.
- Once you find the right form, click Get now.
- Choose a payment plan that suits you, provide the necessary information to create your account, and pay for your order using PayPal or Visa or Mastercard.
- Select a convenient document format and download your copy.
Form popularity
FAQ
COBRA continuation rights are usually limited to either 18 or 36 months (with the exception of continued coverage under COBRA for a maximum period of: 1. 18 months if coverage would otherwise end due to: Termination, or 2022 Reduction of hours.
Second qualifying events may include the death of the covered employee, divorce or legal separation from the covered employee, the covered employee becoming entitled to Medicare benefits (under Part A, Part B or both), or a dependent child ceasing to be eligible for coverage as a dependent under the group health plan.
Losing COBRA Benefits Here's the good news: Rolling off of COBRA coverage is a qualifying event that opens a special enrollment period for you to purchase your own health coverage. And you'll have more options, flexibility and control of your health plan outside of COBRA with an individual health insurance plan.
For covered employees, the only qualifying event is termination of employment (whether the termination is voluntary or involuntary) including by retirement, or reduction of employment hours. In that case, COBRA lasts for eighteen months.
ARBenefits is a comprehensive major medical health plan, with covered services including preventative care, physician services, hospital admissions & outpatient care, prescription drug coverage, behavioral/mental health services, rehabilitation, emergency care, and much more.
When the qualifying event is the covered employee's termination of employment or reduction in hours of employment, qualified beneficiaries are entitled to 18 months of continuation coverage.
Yes, You Can Get COBRA Insurance After Quitting Your Job According to the Consolidated Omnibus Budget Reconciliation Act of 1985 (COBRA), companies with 20 or more employees are required to allow workers to keep their health insurance coverage, if that coverage would end due to a qualifying event.
The following are qualifying events: the death of the covered employee; a covered employee's termination of employment or reduction of the hours of employment; the covered employee becoming entitled to Medicare; divorce or legal separation from the covered employee; or a dependent child ceasing to be a dependent under
COBRA allows you to continue coverage typically for up to 18 months after you leave your employer. You can buy an Affordable Care Act (ACA) plan through a public exchange on the health insurance marketplace. Or you can switch to your spouse or partner's plan, if possible.
COBRA Qualifying Event Notice The employer must notify the plan if the qualifying event is: Termination or reduction in hours of employment of the covered employee, 2022 Death of the covered employee, 2022 Covered employee becoming entitled to Medicare, or 2022 Employer bankruptcy.