Arkansas COBRA Continuation Coverage Election Notice
Description
How to fill out COBRA Continuation Coverage Election Notice?
Are you in the situation where you need documents for either business or particular functions almost every working day? There are numerous legal document formats accessible online, but finding reliable templates is not simple.
US Legal Forms offers thousands of template formats, such as the Arkansas COBRA Continuation Coverage Election Notice, that are designed to meet both federal and state requirements.
If you are already familiar with the US Legal Forms website and have an account, simply Log In. After that, you can download the Arkansas COBRA Continuation Coverage Election Notice template.
- Find the document you need and ensure it is for the correct area/state.
- Use the Review button to look over the document.
- Check the details to confirm that you have selected the right form.
- If the document does not match your needs, use the Lookup field to find the template that suits your requirements.
- Once you find the correct document, click Acquire now.
- Choose the subscription plan you want, complete the necessary details to create your account, and pay for the order using your PayPal or credit card.
- Select a convenient file format and download your copy.
Form popularity
FAQ
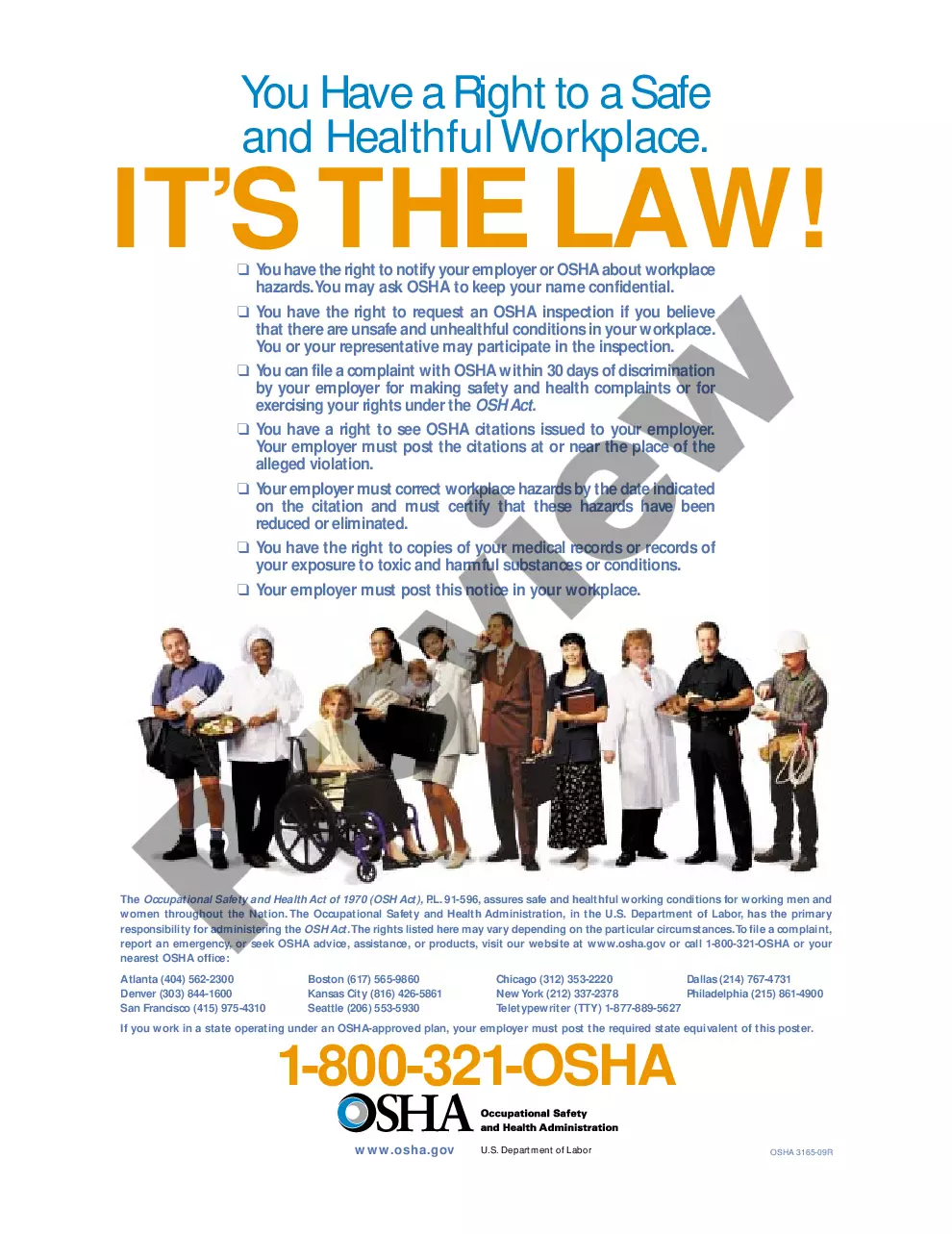
Arkansas has a mini-COBRA law that extends COBRA insurance plans for employees at companies with less than 20 employees. This means workers in Arkansas have a right to continue their workplace insurance, even if they quit their jobs or were involuntarily terminated (getting fired).
COBRA is always effective the day after your active coverage ends. For most, active coverage terminates at the end of a month and COBRA is effective on the first day of the next month.
COBRA is a federal law about health insurance. If you lose or leave your job, COBRA lets you keep your existing employer-based coverage for at least the next 18 months. Your existing healthcare plan will now cost you more. Under COBRA, you pay the whole premium including the share your former employer used to pay.
The following are qualifying events: the death of the covered employee; a covered employee's termination of employment or reduction of the hours of employment; the covered employee becoming entitled to Medicare; divorce or legal separation from the covered employee; or a dependent child ceasing to be a dependent under
Federal law requires that most group health plans (including this Plan) give employees and their families the opportunity to continue their health care coverage through COBRA continuation coverage when there's a qualifying event that would result in a loss of coverage under an employer's plan.
COBRA the Consolidated Omnibus Budget Reconciliation Act -- requires group health plans to offer continuation coverage to covered employees, former employees, spouses, former spouses, and dependent children when group health coverage would otherwise be lost due to certain events.
Key Takeaways. COBRA provides a good option for keeping your employer-sponsored health plan for a while after you leave your job. Although, the cost can be high. Make an informed choice by looking at all your options during the 60-day enrollment period, and don't focus on the premium alone.
The general notice describes general COBRA rights and employee obligations. This notice must be provided to each covered employee and each covered spouse of an employee who becomes covered under the plan. The notice must be provided within the first 90 days of coverage under the group health plan.
COBRA continuation rights are usually limited to either 18 or 36 months (with the exception of continued coverage under COBRA for a maximum period of: 1. 18 months if coverage would otherwise end due to: Termination, or 2022 Reduction of hours.