Arkansas Affidavit of No Coverage by Another Group Health Plan
Description
How to fill out Affidavit Of No Coverage By Another Group Health Plan?
Are you currently in a situation where you frequently require documents for either business or personal purposes almost every day.
There are numerous legal document templates accessible online, but locating reliable ones can be challenging.
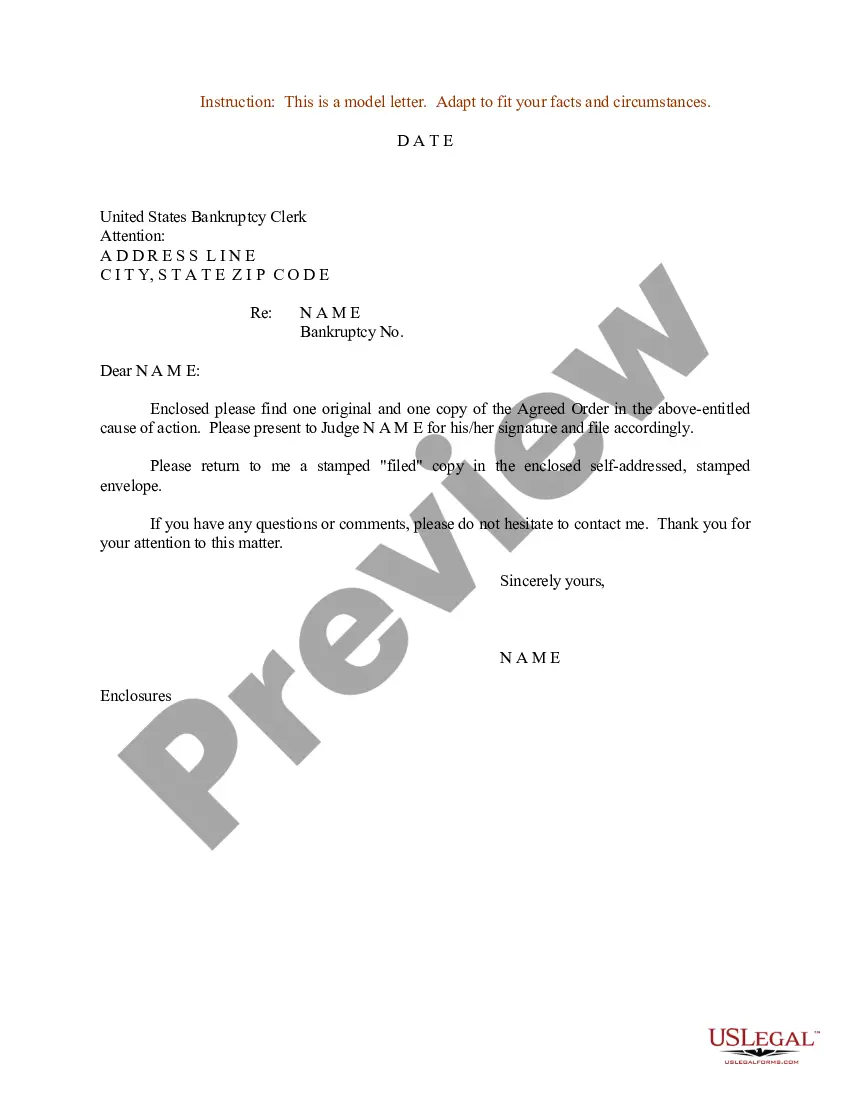
US Legal Forms offers thousands of form templates, including the Arkansas Affidavit of No Coverage by Another Group Health Plan, designed to comply with state and federal requirements.
Once you find the correct form, click on Get now.
Choose the pricing plan you want, complete the necessary details to create your account, and pay for the order using your PayPal or credit card.
- If you are already familiar with the US Legal Forms website and have an account, simply Log In.
- From there, you can download the Arkansas Affidavit of No Coverage by Another Group Health Plan template.
- If you do not have an account and wish to start using US Legal Forms, follow these steps.
- Obtain the form you need and ensure it is for your correct city/state.
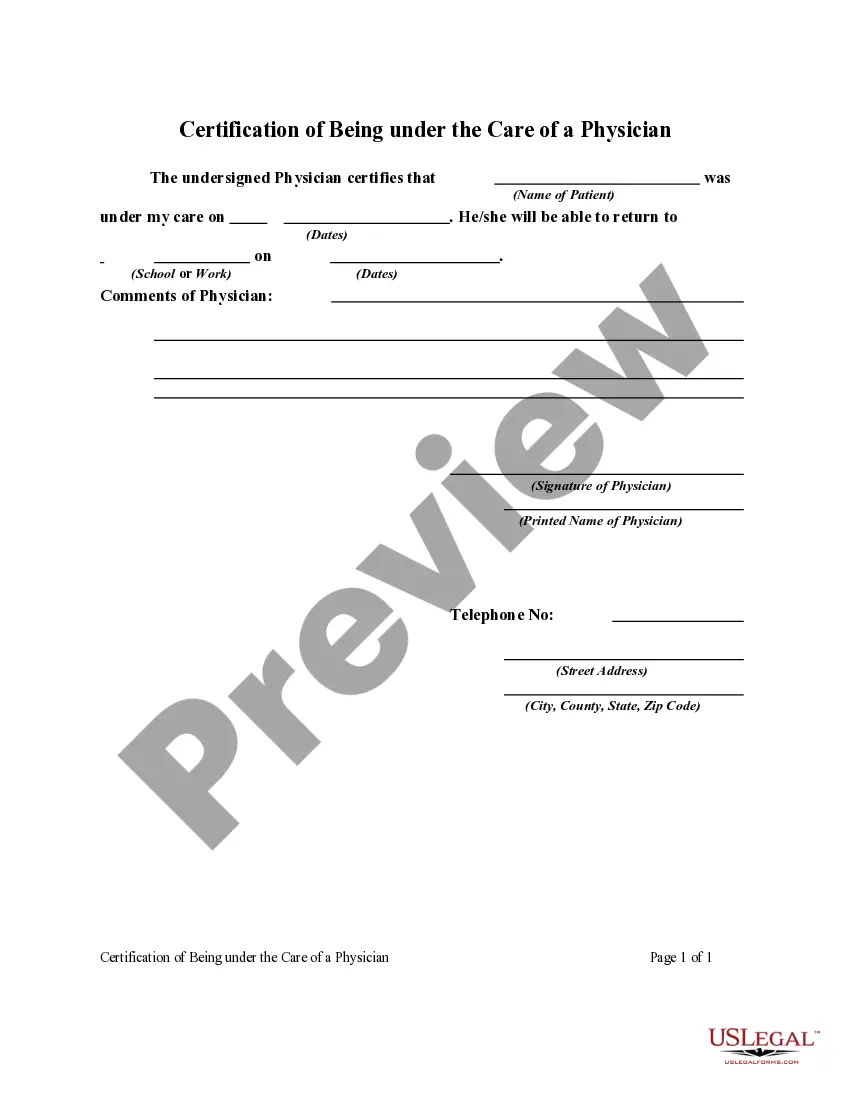
- Use the Preview button to view the form.
- Read the description to ensure you have selected the right document.
- If the form is not what you are looking for, use the Lookup field to find the form that fits your needs and requirements.
Form popularity
FAQ
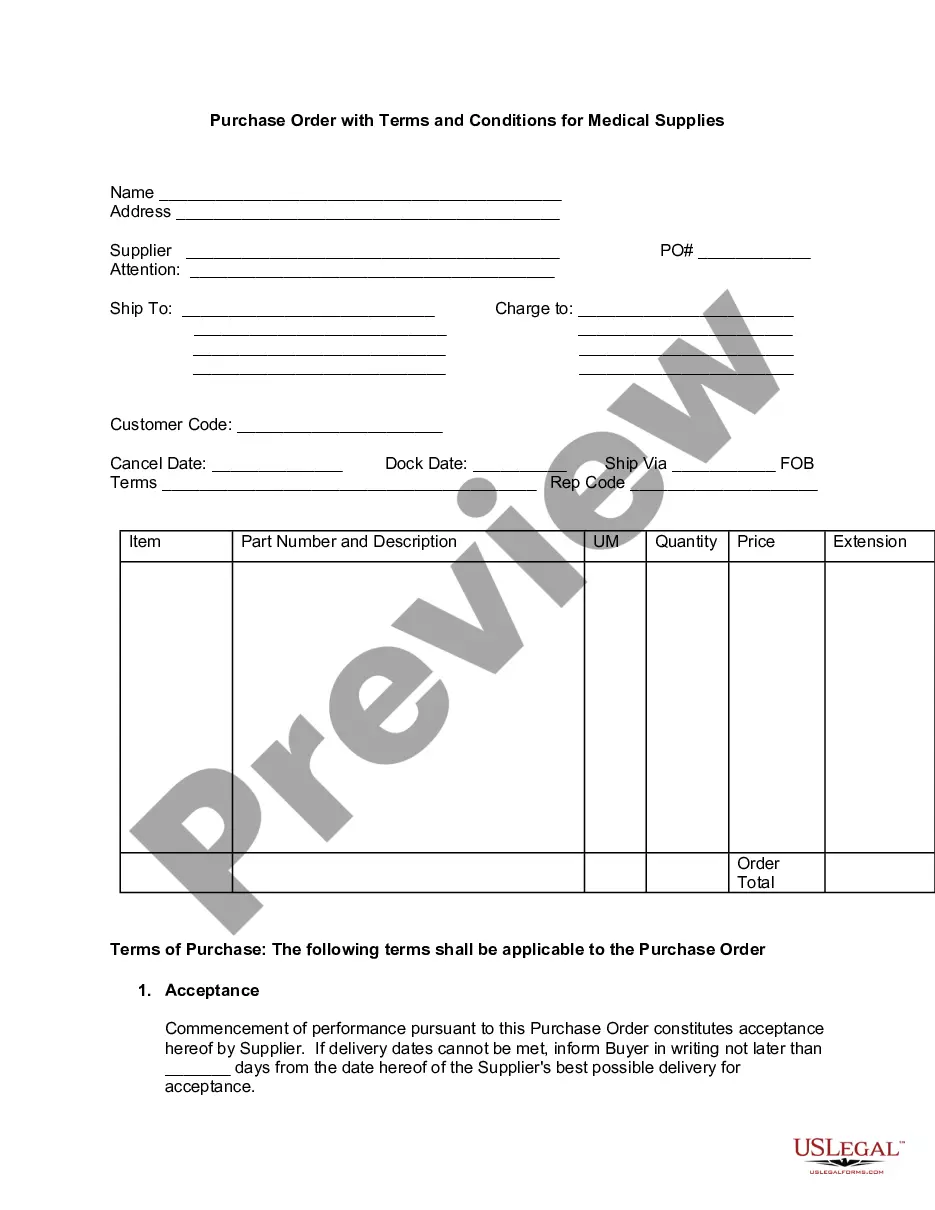
Noncontributory Insurance a plan of insurance for which the employer pays the entire premium and the employee does not contribute to premium payment.
The Coordination of Benefits (COB) provision applies when a person has health care coverage under more than one Plan. Plan is defined below. The order of benefit determination rules govern the order in which each Plan will pay a claim for benefits.
A contributory pension plan requires the employees to pay into the plan from their salary (the employees' pay stub would show the money was taken out of their pay to go into the pension plan). In a non-contributory pension plan only the employer contributes.
Noncontributory - Group life insurance plans are those in which the employer pays the entire premium and the employee supplies no portion of the premium costs. Employers have the option of contributing to the employees' premium payments in part or in full.
What is the contract called that is issued to an employer for a Group Medical Insurance plan? (An employer would be a possible applicant and contract policyholder of a single master contract or master policy for group health benefits.)
However, the following individuals are NOT eligible to participate in Section 125 Cafeteria Plan, Flexible Spending Account (FSA), or Premium Only Plan (POP), or any of its qualified benefits: More than 2% shareholder of an S-corporation, or any of its family members, Sole proprietor, Partner in a partnership, or.
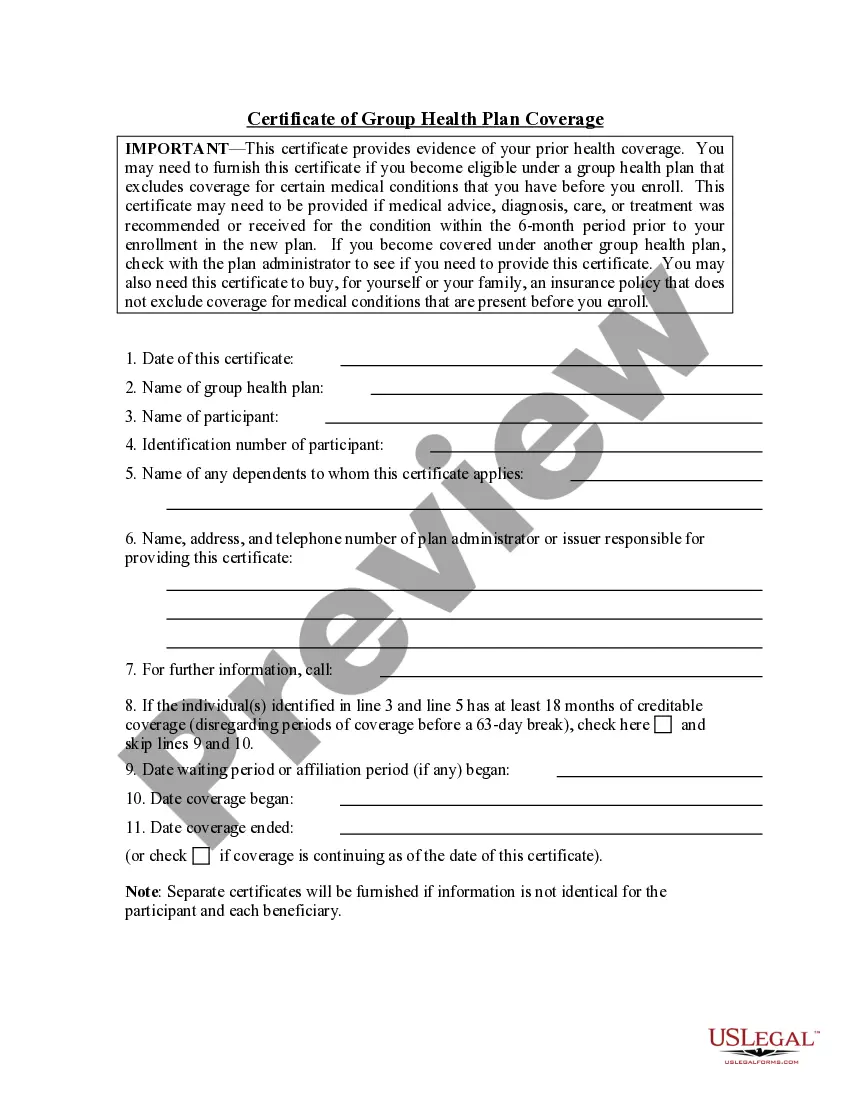
The primary purpose of the certificate is to show the amount of creditable coverage that you had under a group health plan or other health insurance coverage, because this can reduce or eliminate the length of time that any pre-existing condition clause in a new plan otherwise might apply to you.
The purpose of the coordination of benefits (COB) provision is to avoid duplication of benefit payments and over insurance when an individual is covered under more than one group health plan.
When can a group health policy renewal be denied according to the Health Insurance Portability and Accountability Act (HIPAA)? When contribution or participation rules have been violated. Mark continues working after the age of 65 and is covered through his employer's group health plan.
For the most part, insurance companies prefer to cover only your immediate family on your health insurance policy. But there are situations in which people outside of your immediate family could qualify to be covered by your health insurance plan.