Alaska Introductory COBRA Letter
Description
How to fill out Introductory COBRA Letter?
Are you presently in a situation where you frequently require documents for either corporate or personal reasons.
There are numerous legal document templates accessible online, but finding trustworthy versions can be challenging.
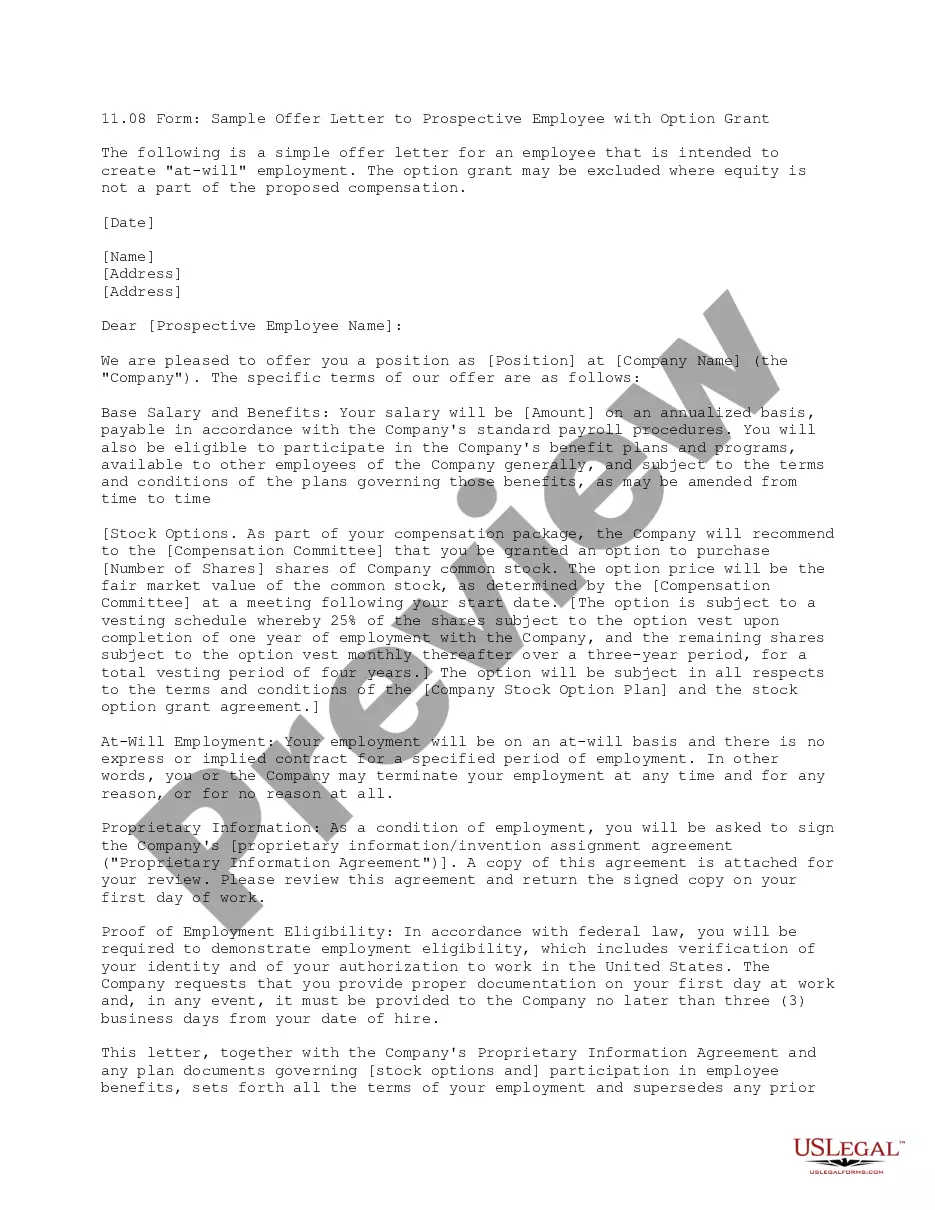
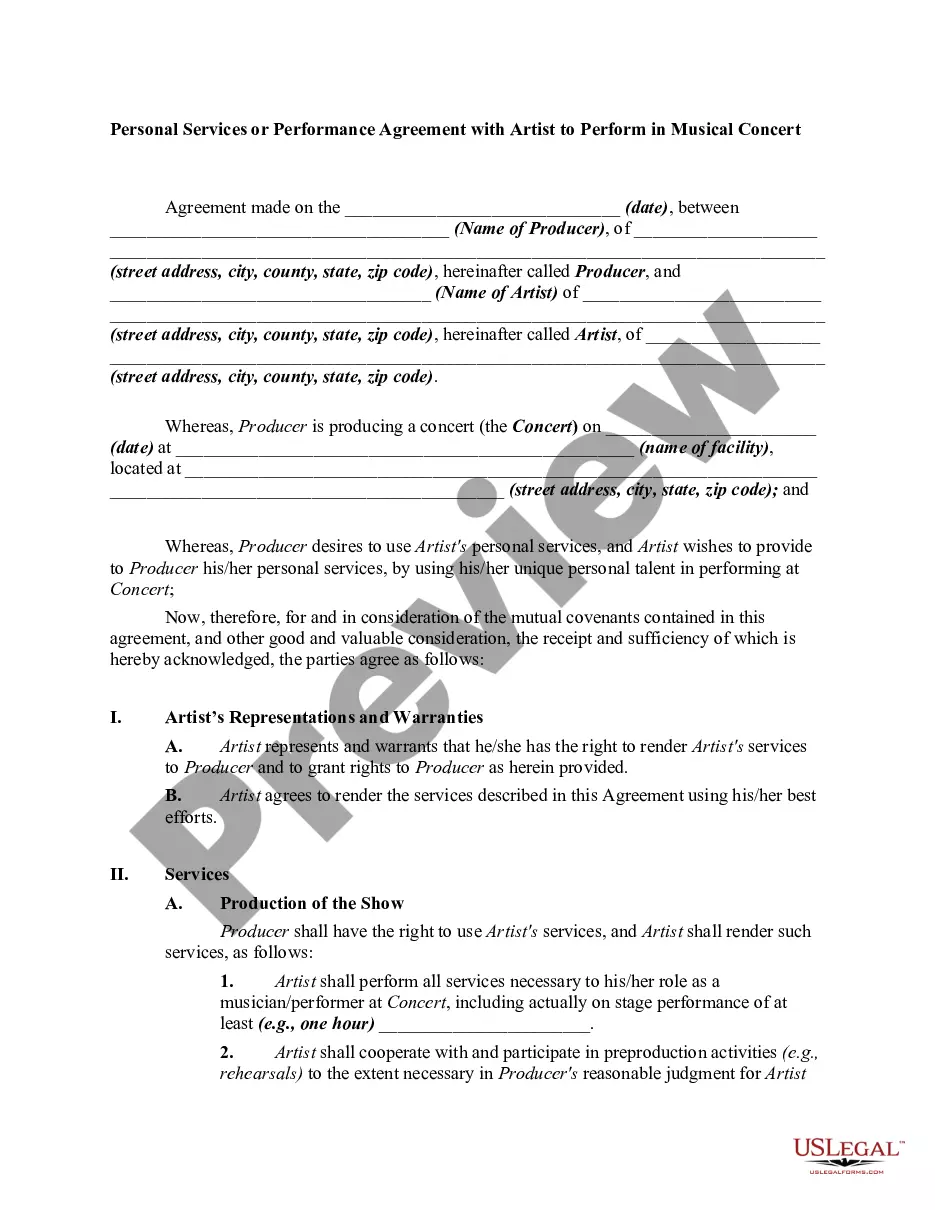
US Legal Forms offers a wide array of form templates, such as the Alaska Introductory COBRA Letter, which can be crafted to meet federal and state requirements.
Access all of the document templates you have purchased in the My documents section.
You can obtain an additional copy of the Alaska Introductory COBRA Letter at any time, if needed. Just click the necessary form to download or print the document template.
- If you are already familiar with the US Legal Forms website and have an account, simply Log In.
- Then, you may download the Alaska Introductory COBRA Letter template.
- If you do not have an account and wish to start using US Legal Forms, follow these steps.
- Find the form you need and ensure it is for the correct city/state.
- Utilize the Preview button to review the form.
- Check the details to confirm you have selected the correct form.
- If the form is not what you are looking for, use the Lookup field to find the form that fits your needs and criteria.
- Once you secure the appropriate form, click Get now.
- Select the payment plan you prefer, complete the required information to create your account, and pay for the order using your PayPal or credit card.
- Choose a suitable file format and download your copy.
Form popularity
FAQ
Failure to pay premiums. When a participant fails to make a timely payment of any required COBRA premium, the employer may terminate COBRA coverage. Employers must provide participants with at least a 30-day grace period for payment of any late premiums.
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
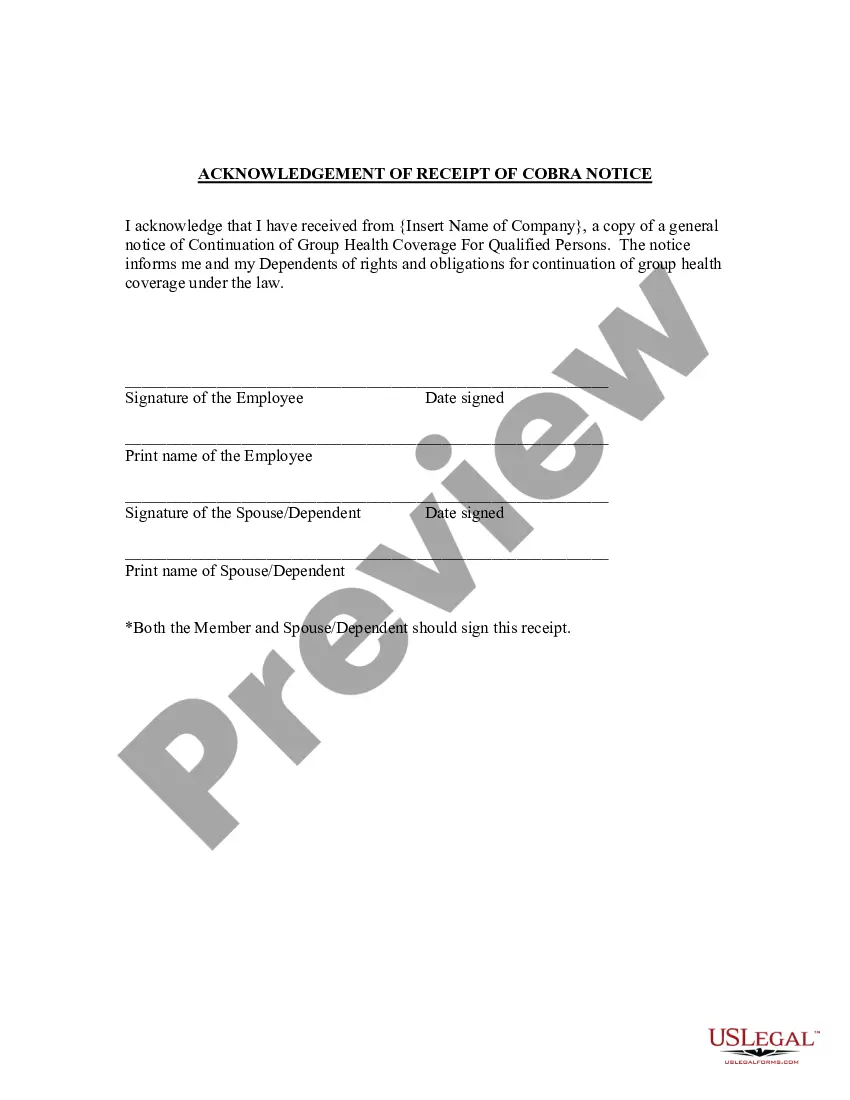
The initial notice, also referred to as the general notice, communicates general COBRA rights and obligations to each covered employee (and his or her spouse) who becomes covered under the group health plan.
COBRA the Consolidated Omnibus Budget Reconciliation Act -- requires group health plans to offer continuation coverage to covered employees, former employees, spouses, former spouses, and dependent children when group health coverage would otherwise be lost due to certain events.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
The American Rescue Plan Act and COBRA AssistanceARPA creates a new 100 percent subsidy for COBRA coverage premiums from April 1, 2021, through September 30, 2021. Additionally, ARPA opens up the ability to enroll in COBRA coverage even if a person declined coverage earlier or if their enrollment window closed.
When does COBRA continuation coverage startCOBRA is always effective the day after your active coverage ends. For most, active coverage terminates at the end of a month and COBRA is effective on the first day of the next month.
If You Do Not Receive Your COBRA PaperworkReach out to the Human Resources Department and ask for the COBRA Administrator. They may use a third-party administrator to handle your enrollment. If the employer still does not comply you can call the Department of Labor at 1-866-487-2365.