Cobra Enrollment Form For Child Care
Description
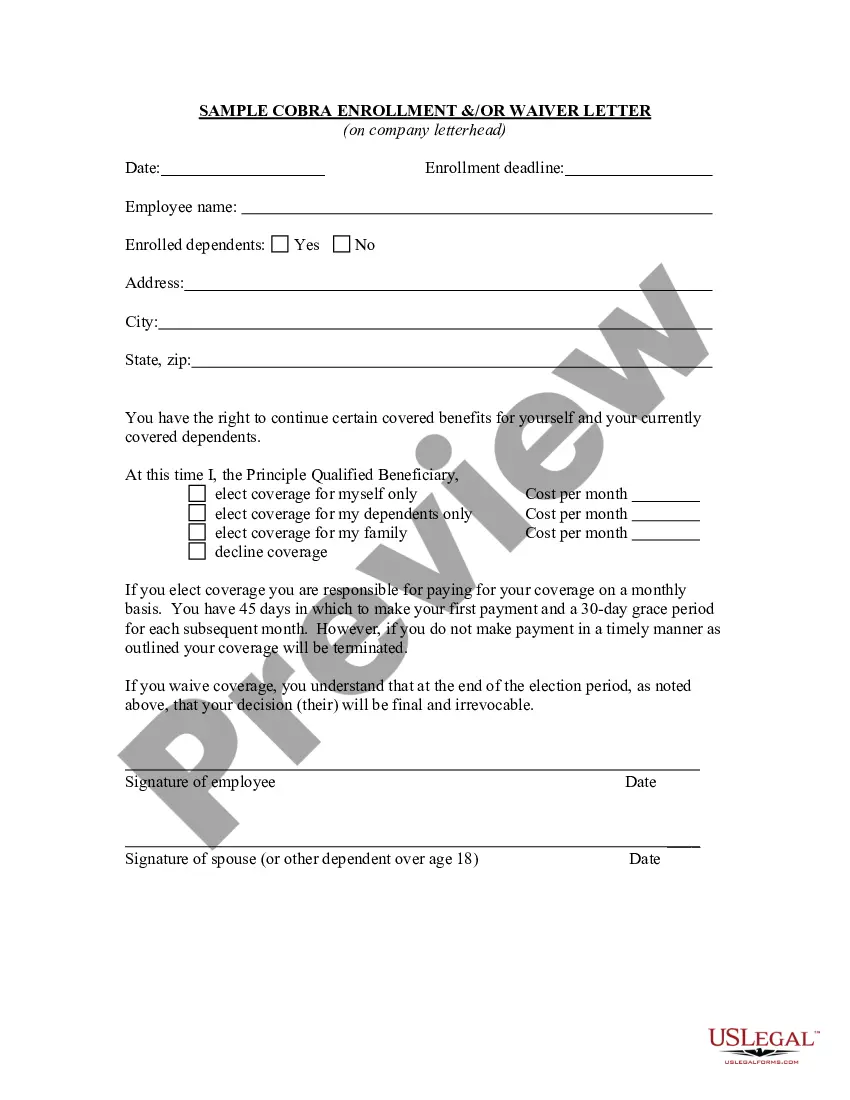
How to fill out Sample COBRA Enrollment And / Or Waiver Letter?
The Cobra Registration Document For Child Care you observe on this page is a reusable official template crafted by qualified attorneys in accordance with federal and local laws.
For over 25 years, US Legal Forms has been delivering individuals, businesses, and legal professionals with more than 85,000 authenticated, state-specific documents for any commercial and personal circumstance. It is the fastest, easiest, and most dependable approach to acquire the paperwork you require, as the service ensures the utmost level of data protection and anti-malware safeguards.
Subscribe to US Legal Forms to access verified legal templates for all of life’s situations at your fingertips.
- Search for the document you want and examine it.
- Select the pricing option that suits your needs and create an account. Use PayPal or a credit card for prompt payment. If you already possess an account, Log In and verify your subscription to proceed.
- Choose the file format you prefer for your Cobra Registration Document For Child Care (PDF, DOCX, RTF) and store the template on your device.
- Complete and endorse the documentation. Print the template to fill it out manually. Alternatively, utilize an online multifunctional PDF editor to swiftly and accurately complete and sign your form with a valid signature.
- Access your documents again. Utilize the same file anytime it's required. Navigate to the My documents tab in your profile to redownload any previously purchased documents.
Form popularity
FAQ
Having A Newborn Is A Qualifying Event Your newborn child can be added on to COBRA for additional premiums.
How to get COBRA coverage. When a qualifying life event happens, you or your employer will notify the health plan. The plan will send an election notice that you will have 60 days to respond to. If you elect to take COBRA coverage, your employer may pay a portion of or the full amount of your insurance premium.
They must be enrolled during either the plans' special 30-day enrollment period or some other period such as open enrollment. In summary although a newborn or newly adopted child is automatically considered a qualified beneficiary, the child is not covered until enrollment occurs.
You may change plans and add/delete eligible dependents. Dependents added during open enrollment will not have the same COBRA rights as the ?qualified beneficiaries.? What are the special application rules in California?
Applying for COBRA begins with the employer who provided the health plan to notify you of your right to continuation. The employer has 30 days to notify the group health plan of the qualifying event. After that, the employer has 14 days to notify you of your COBRA right to keep your work health insurance.