Certificate Health Plan With Secondary Coverage
Description
How to fill out Certificate Of Group Health Plan Coverage?
Obtaining legal templates that adhere to national and state regulations is crucial, and the web presents numerous selections to consider.
However, what’s the benefit of spending time hunting for the appropriate Certificate Health Plan With Secondary Coverage example online if the US Legal Forms digital library already has such templates compiled in a single location.
US Legal Forms is the largest digital legal resource featuring over 85,000 customizable templates created by attorneys for any professional and personal situation. They are simple to navigate, with all documents organized by state and intended use. Our experts stay updated with legal modifications, ensuring that your documents are always current and comply when obtaining a Certificate Health Plan With Secondary Coverage from our site.
All templates accessible through US Legal Forms are reusable. To re-download and fill out previously saved forms, visit the My documents section in your profile. Make the most of the most extensive and user-friendly legal document service!
- Acquiring a Certificate Health Plan With Secondary Coverage is fast and straightforward for both existing and new users.
- If you already possess an account with an active subscription, Log In and save the document template you require in the appropriate format.
- If you are new to our site, adhere to the steps provided below.
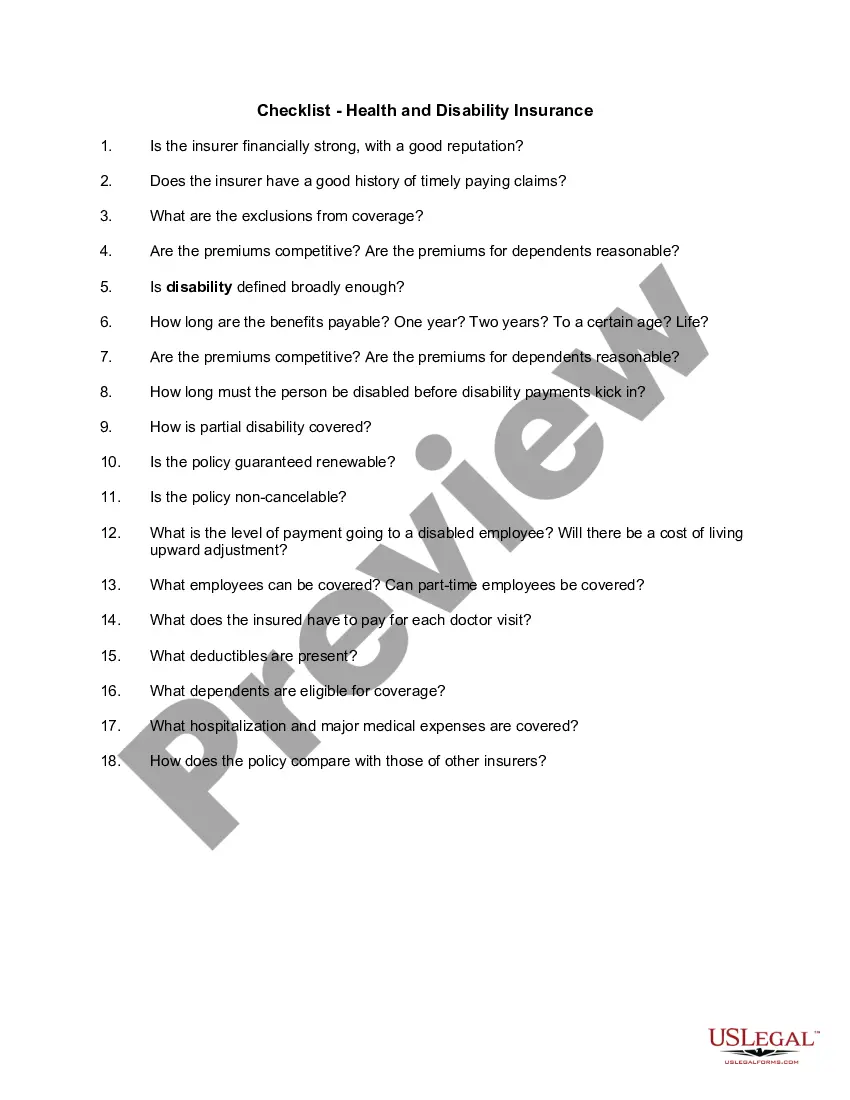
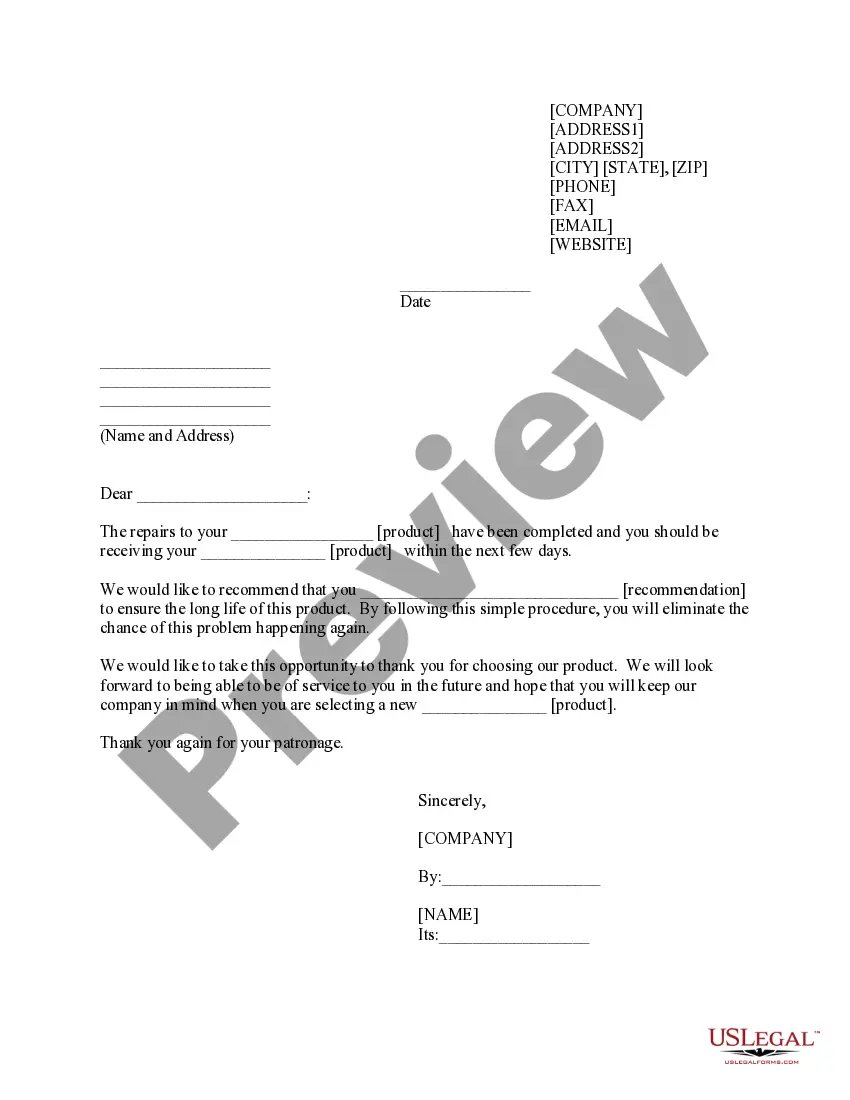
- Review the template using the Preview feature or through the text outline to verify that it fulfills your requirements.
- Search for another template using the search function at the top of the page if necessary.
- Click Buy Now once you’ve found the correct form and choose a subscription option.
- Create an account or Log In, and complete your payment via PayPal or a credit card.
- Select the right format for your Certificate Health Plan With Secondary Coverage and download it.
Form popularity
FAQ
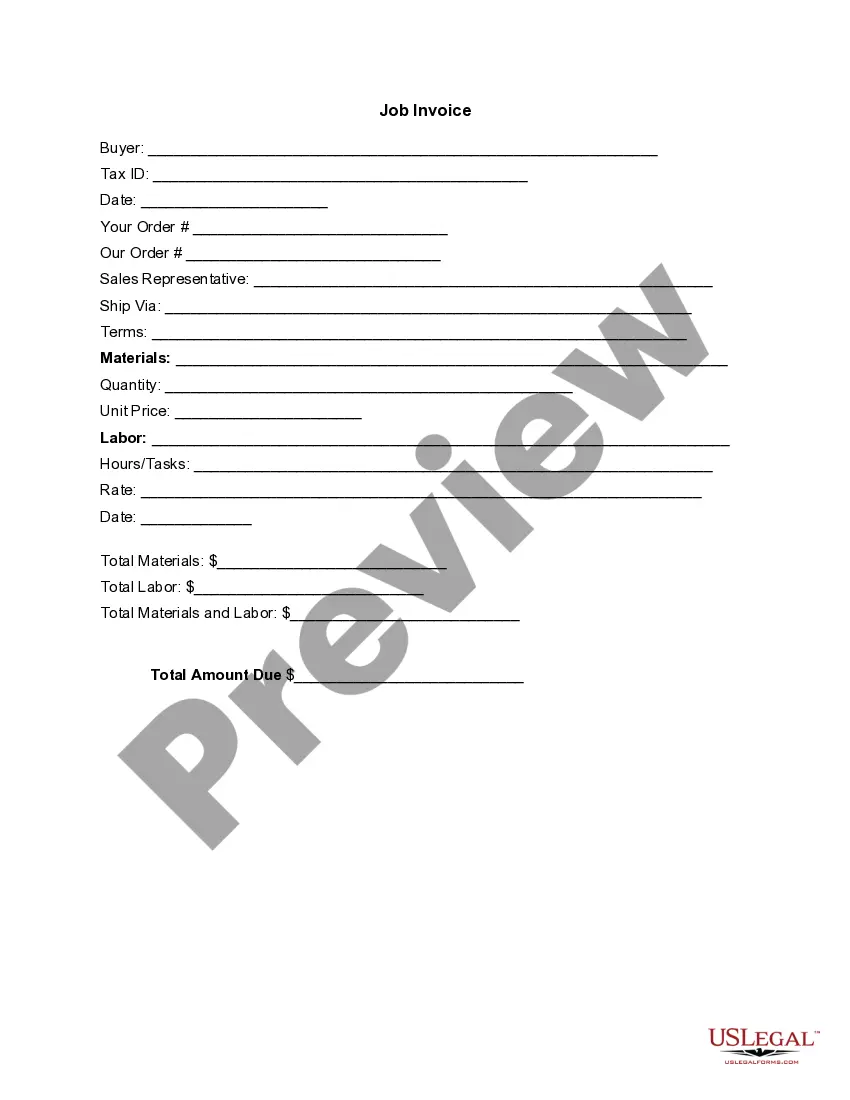
To submit a bill to your secondary insurance after using a Certificate health plan with secondary coverage, start by ensuring your primary insurance has processed the claim. Gather all necessary documents, including the Explanation of Benefits (EOB) from your primary insurer. Then, fill out the claim form for your secondary insurance and submit it along with the required documentation. Utilizing platforms like uslegalforms can simplify this process by providing the forms and guidance you need.
Having two health insurance plans, including a Certificate health plan with secondary coverage, allows you to enhance your overall coverage. The primary plan will cover your healthcare expenses first, while the secondary plan steps in to cover any remaining costs. This dual coverage can significantly reduce your financial burden and provide you with access to a broader range of services.
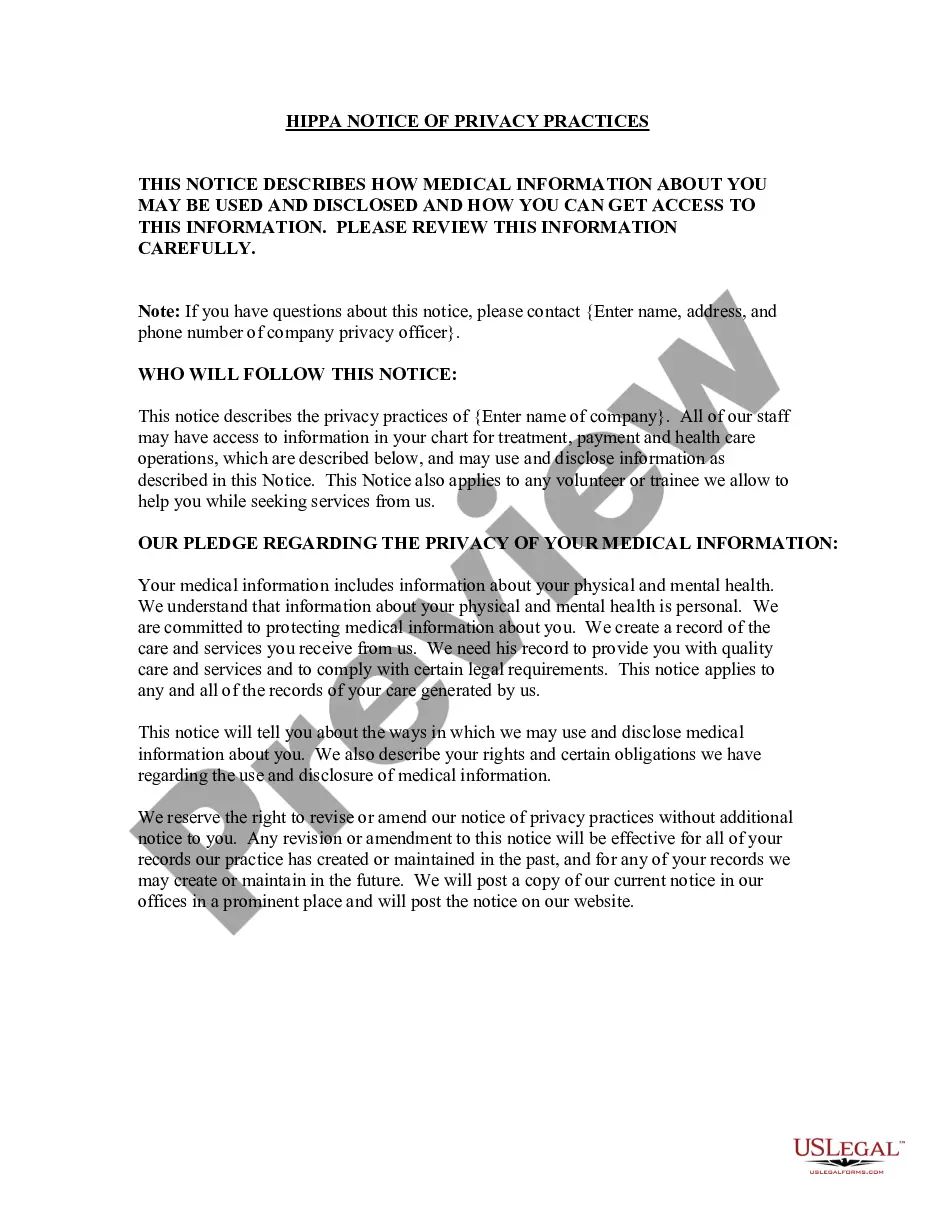
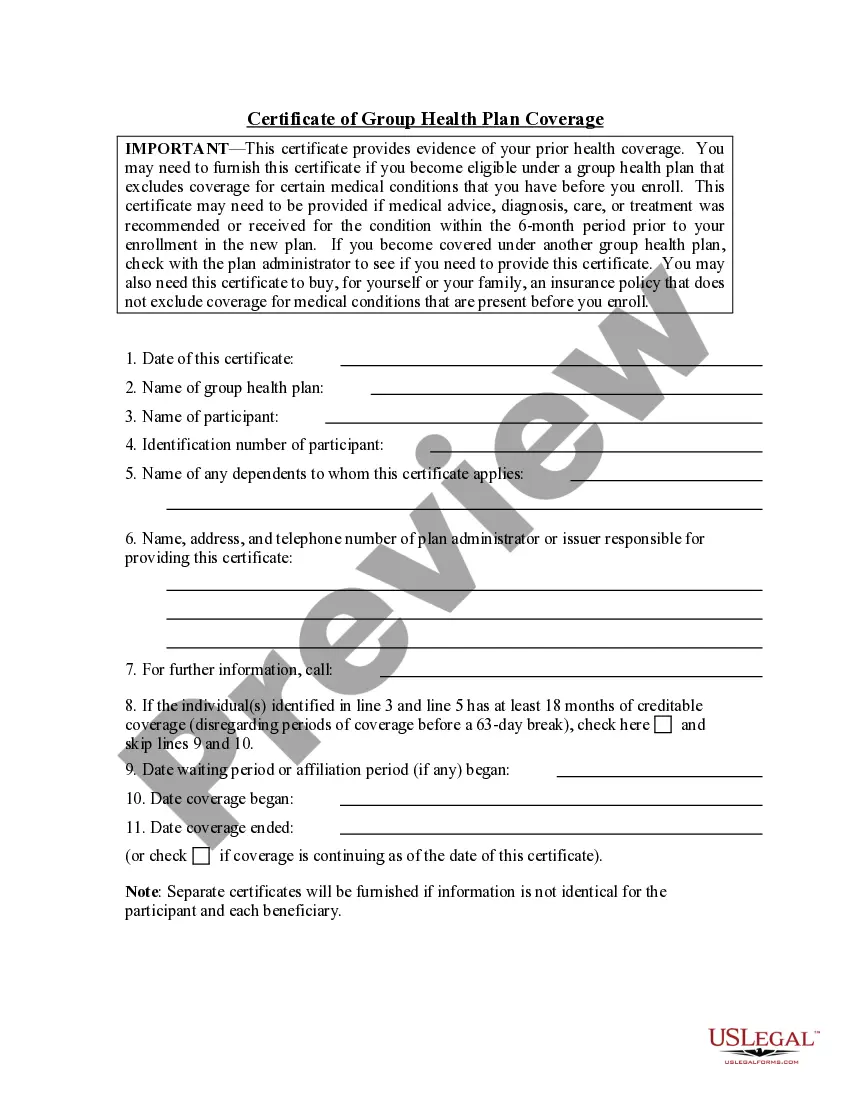
Coordination of Benefits (COB) is essential when dealing with a Certificate health plan with secondary coverage. COB determines which insurance pays first based on various factors, such as the order of enrollment or specific plan rules. Understanding how COB functions helps you avoid billing errors and ensures that both your primary and secondary plans work together effectively.
When you have a Certificate health plan with secondary coverage, billing can become straightforward. Typically, your primary insurance pays first, covering its share of the costs. After that, the remaining balance is sent to your secondary insurance for additional coverage. This process ensures you maximize your benefits and minimize out-of-pocket expenses.
The insurance that pays first is called the primary payer. The primary payer pays up to the limits of its coverage. The insurance that pays second is called the secondary payer. The secondary payer only pays if there are costs the primary insurer didn't cover.
Is Secondary Insurance Worth It? Secondary health insurance can help reduce out-of-pocket costs, but having multiple health plans isn't always a great situation. Paying two premiums and deductibles and juggling two provider networks and health plan benefits may be costly and a health insurance headache.
Secondary insurance is health insurance that pays after primary insurance on a claim for medical or hospital care. It usually pays for some or all of the costs left after the primary insurer has paid (e.g., deductibles, copayments, coinsurances).
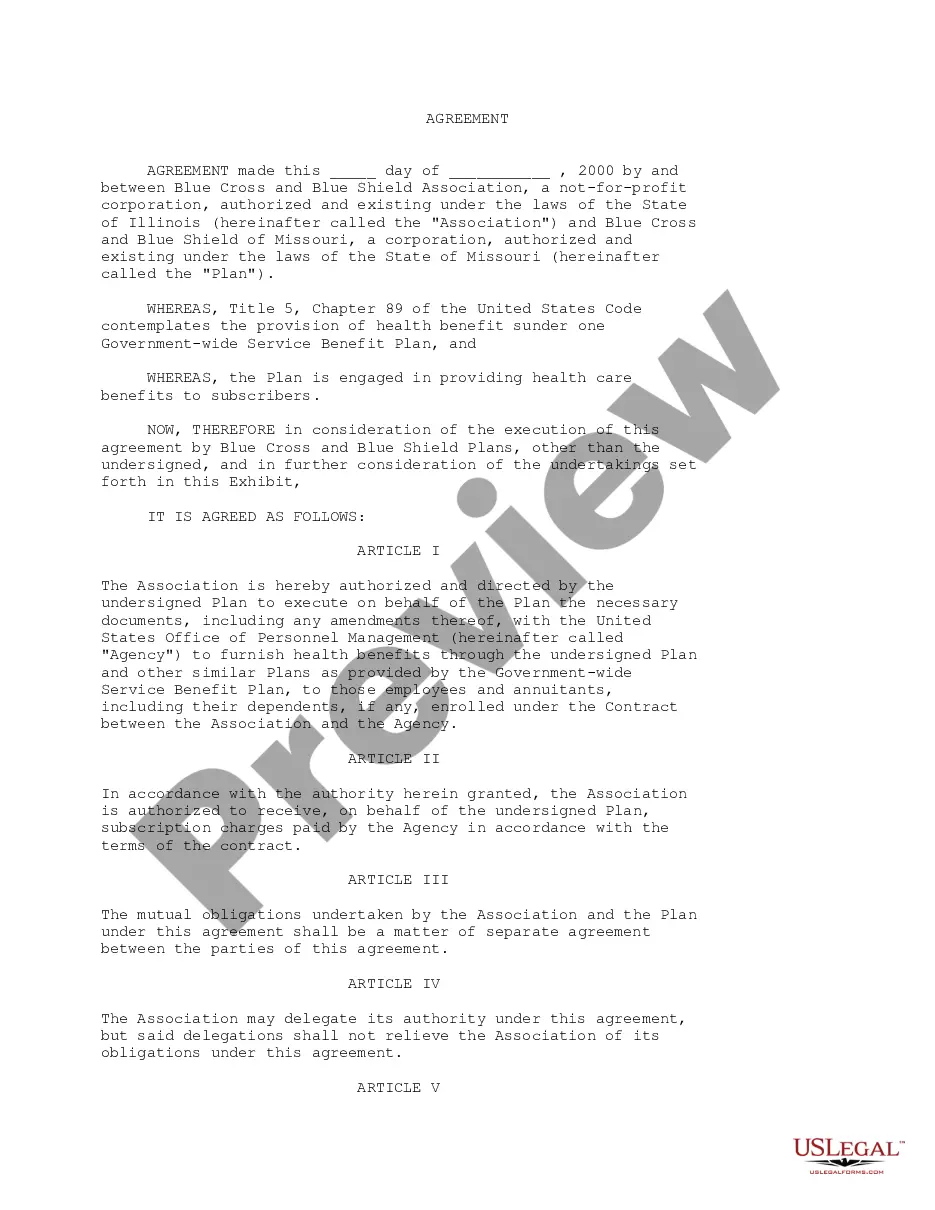
The primary insurance is where health claims are submitted first. The secondary insurance will then pay for whatever remaining costs are eligible for coverage under its health plan. When two health insurance providers work together in this way to provide coverage, this is called coordination of benefits.
There are drawbacks to consider too. The secondary plan may not pay all the costs left uncovered by your primary plan. And, you may have more paperwork and headaches dealing with two plans rather than one. You'll have to notify each insurer about the other.