Cobra Coverage Complete With Iron
Description
How to fill out COBRA Continuation Coverage Election Form?
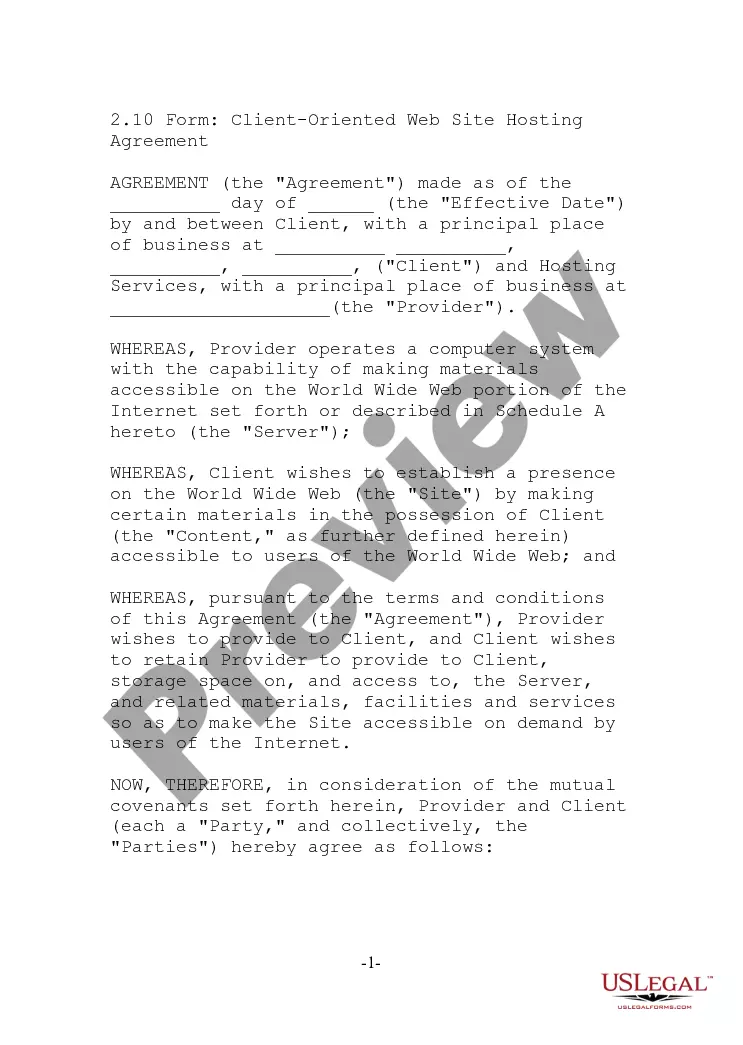
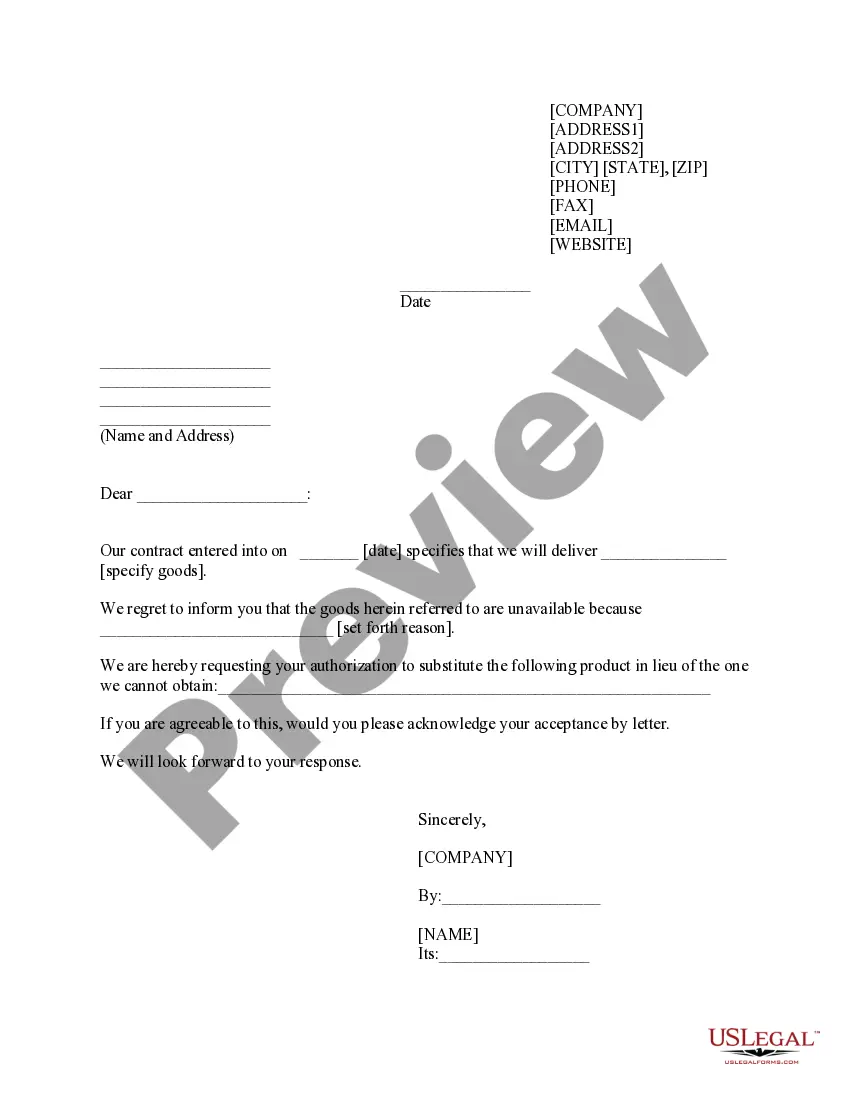
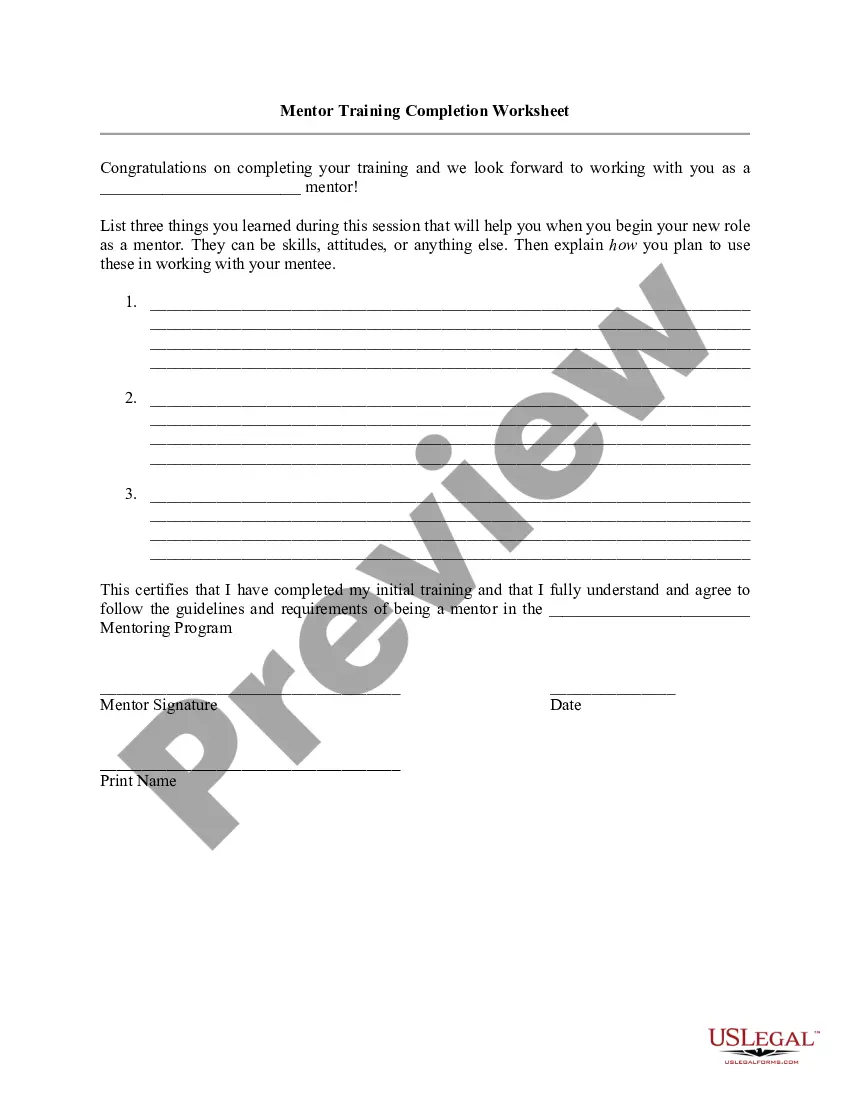
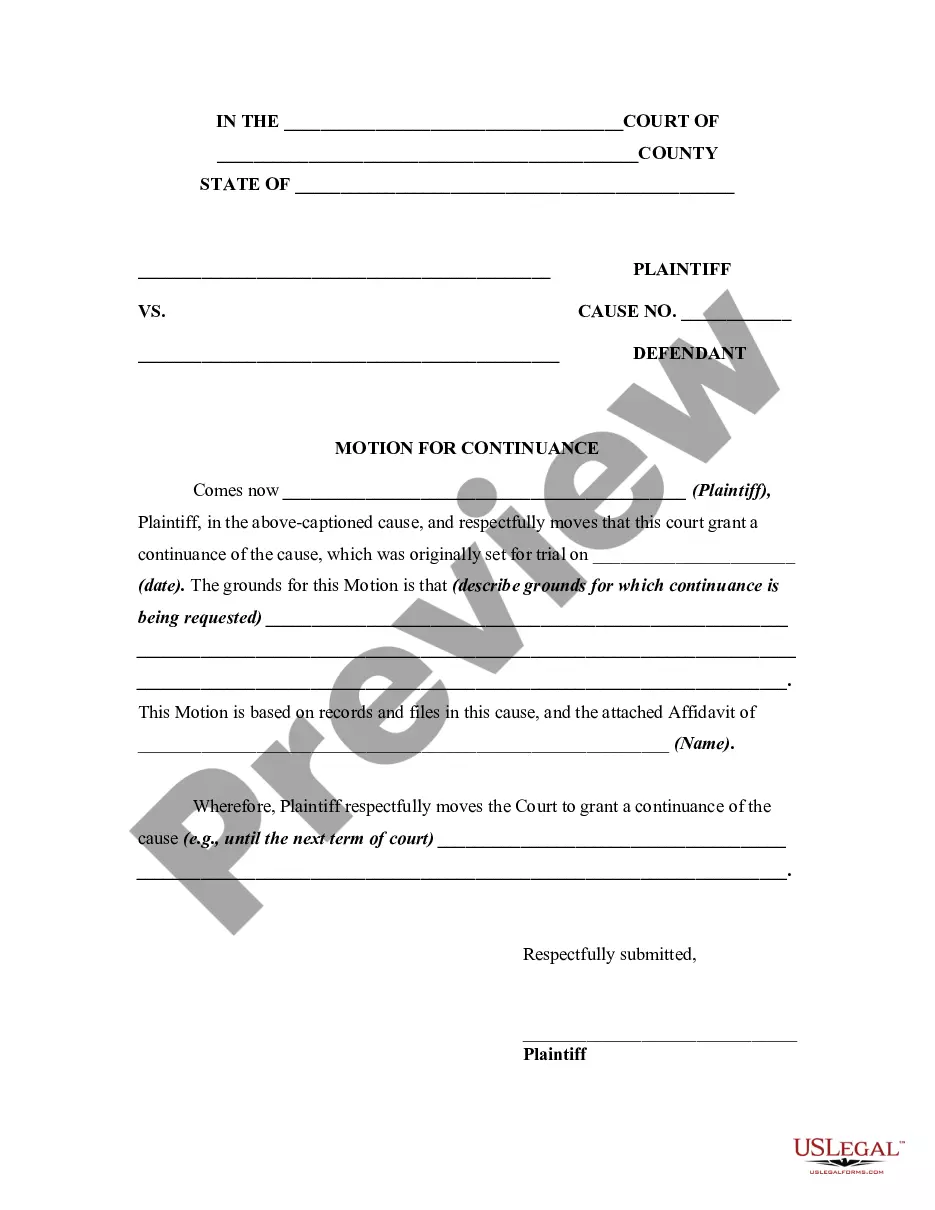
Acquiring legal document samples that comply with federal and state regulations is essential, and the internet provides numerous choices to select from.
However, what is the benefit of spending time searching for the suitable Cobra Coverage Complete With Iron template online if the US Legal Forms digital library already compiles such forms in one location.
US Legal Forms is the largest online legal repository with over 85,000 fillable documents prepared by legal professionals for any commercial and personal circumstances.
Review the template using the Preview feature or via the text description to verify it satisfies your requirements.
- They are easy to navigate with all documents organized by state and intended usage.
- Our specialists keep updated with legislative modifications, so you can always trust that your documents are current and compliant when acquiring a Cobra Coverage Complete With Iron from our site.
- Getting a Cobra Coverage Complete With Iron is quick and straightforward for both existing and new users.
- If you already possess an account with a valid subscription, Log In and retrieve the document sample you require in the correct format.
- If you are new to our site, follow the steps below.
Form popularity
FAQ
COBRA coverage can be costly and may create a financial burden for individuals and families. While it allows you to maintain your existing health insurance, the premiums can be high, putting a strain on your budget. Additionally, COBRA coverage is temporary, typically lasting up to 18 months, which might leave you needing to seek new insurance sooner than anticipated. To navigate these challenges, consider using a platform like US Legal Forms to explore health insurance options that best fit your budget and needs.
COBRA is Retroactive. When you receive your COBRA letter, you have 60 days to submit the paperwork with your insurance company. However, no matter when you submit the paperwork during this time, you are covered retroactively from day 1. The catch: you will also be responsible for all premiums from day 1.
Applying for COBRA begins with the employer who provided the health plan to notify you of your right to continuation. The employer has 30 days to notify the group health plan of the qualifying event. After that, the employer has 14 days to notify you of your COBRA right to keep your work health insurance.
This period is measured from the later of the date of the qualifying event or the date the COBRA election notice is provided. COBRA coverage is retroactive if elected and paid for by the qualified beneficiary.
When Federal COBRA ends, eligible employees can buy 18 months additional health coverage under Cal-COBRA. All qualified beneficiaries are generally eligible for continuation coverage for 36 months after the date the qualified beneficiary's benefits would otherwise have terminated.
With COBRA, you can use your health insurance plan like you did when employed. However, you'll pay all the costs without help from your former employer. You can keep COBRA for at least 18 months. Sometimes, you can have a COBRA plan for up to 36 months, depending on the qualifying event.