Psychotherapy Form Template With Notes
Description
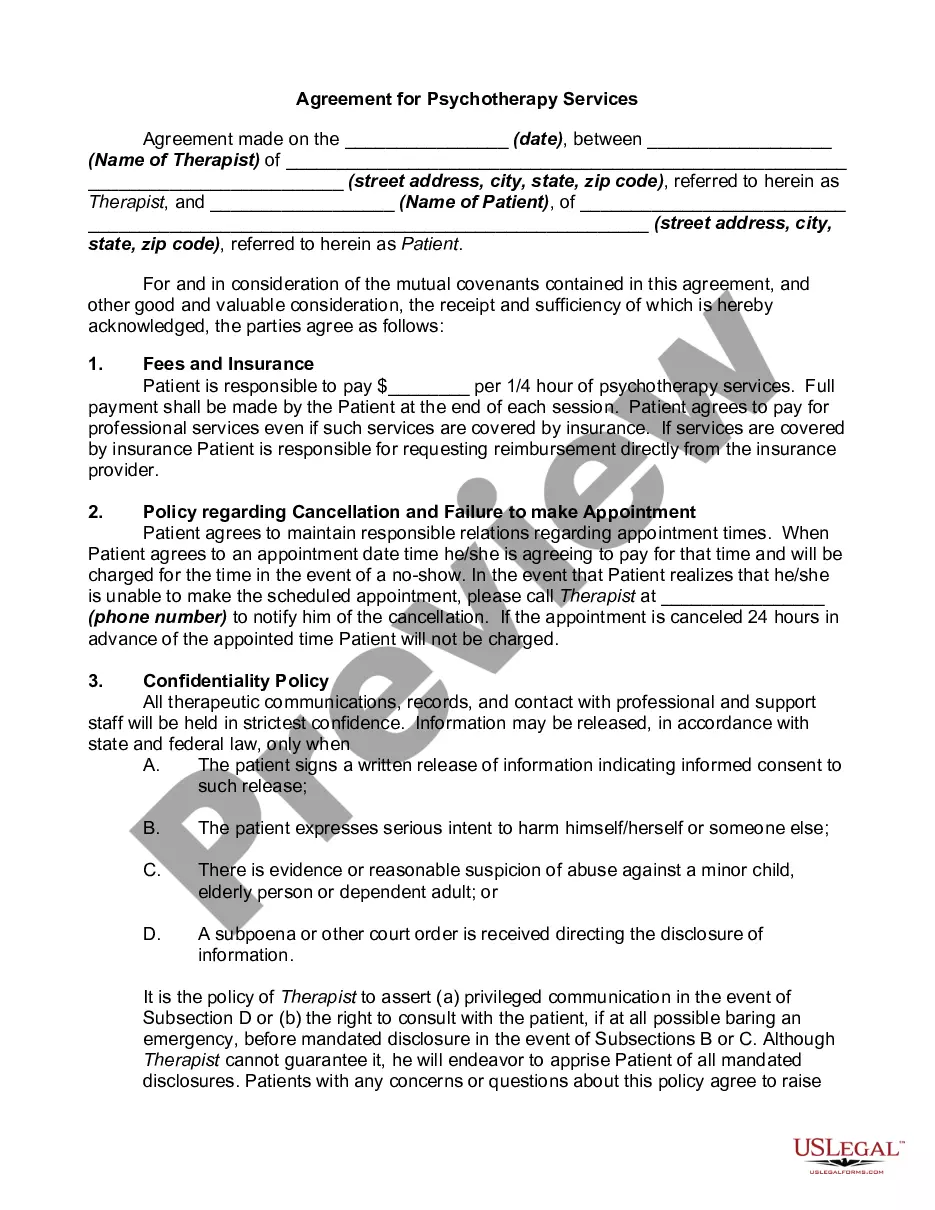
How to fill out Agreement For Psychotherapy Services?
Finding a go-to place to take the most recent and appropriate legal templates is half the struggle of dealing with bureaucracy. Finding the right legal files calls for precision and attention to detail, which is the reason it is very important to take samples of Psychotherapy Form Template With Notes only from reputable sources, like US Legal Forms. A wrong template will waste your time and delay the situation you are in. With US Legal Forms, you have very little to be concerned about. You may access and check all the details regarding the document’s use and relevance for your circumstances and in your state or region.
Consider the following steps to finish your Psychotherapy Form Template With Notes:
- Use the library navigation or search field to find your sample.
- Open the form’s description to see if it matches the requirements of your state and region.
- Open the form preview, if there is one, to ensure the form is definitely the one you are looking for.
- Get back to the search and look for the proper template if the Psychotherapy Form Template With Notes does not fit your requirements.
- If you are positive about the form’s relevance, download it.
- When you are an authorized user, click Log in to authenticate and access your selected templates in My Forms.
- If you do not have a profile yet, click Buy now to get the template.
- Pick the pricing plan that fits your preferences.
- Proceed to the registration to complete your purchase.
- Complete your purchase by picking a transaction method (credit card or PayPal).
- Pick the file format for downloading Psychotherapy Form Template With Notes.
- When you have the form on your device, you may change it with the editor or print it and complete it manually.
Get rid of the headache that comes with your legal paperwork. Discover the extensive US Legal Forms catalog to find legal templates, check their relevance to your circumstances, and download them on the spot.
Form popularity
FAQ
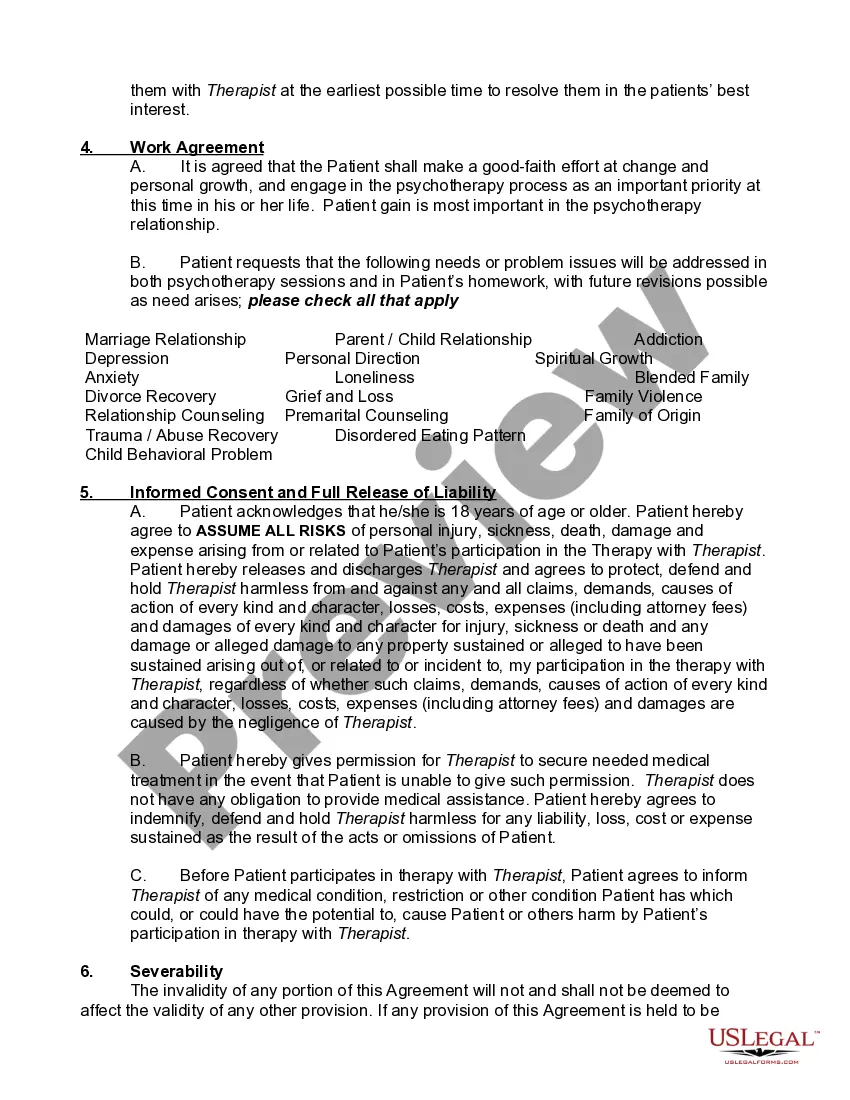
There are some requirements for what must be included in a good example of counseling session notes include: Name. Type of Visit. Date. Length of Visit. Developments From Previous Sessions. Observations About the Client/Patient. Review of the Plan Previously Set in Place. Details of the Session.
Writing Effective Therapy Notes Write clear, easy-to-understandable notes. Be selective, clear, and concise. Familiarize yourself with the HIPAA requirements. Ensure data security. Use simple note-taking templates. Final Thoughts.
7 tips on how to write therapy progress notes Be clear, professional, and to the point. ... Use third-person, objective language. ... Back up your observations with clear evidence. ... Double-check information like date, time, place, and diagnostic code. ... Record any corrections formally. ... Use a note template.
There are several widely used formats for progress notes that can provide a template for making your note-keeping more efficient, while including all of the necessary key points: DAP (Description, Assessment, Plan) BIRP (Behavior, Intervention, Response, Plan) SOAP (Subjective, Objective, Assessment, Plan)
These separate "process notes" are what we are calling "psychotherapy notes." Summary information, such as the current state of the patient, symptoms, summary of the theme of the psychotherapy session, diagnoses, medications prescribed, side effects, and any other information necessary for treatment or payment, is ...