The Reconsideration form for Amerigroup is an essential process that enables members to request a review of a denied claim or a coverage decision. It provides an avenue for members to challenge a decision made by Amerigroup and request a second look at their case. The Reconsideration form for Amerigroup plays a crucial role in ensuring fairness and transparency in the insurance provider's decision-making process. It acts as a recourse for members who believe that their claim was unjustifiably denied or their coverage decision was incorrect. By submitting this form, members can advocate for their rights and present additional evidence or arguments to support their case. Keywords: Amerigroup, Reconsideration form, denied claim, coverage decision, review, second look, recourse, insurance provider, fairness, transparency, unjustifiably denied, additional evidence, arguments, rights. Types of Reconsideration forms for Amerigroup: 1. Medical Claim Reconsideration Form: This form is specifically designed for members who wish to challenge a denied medical claim. It allows them to provide additional medical records, correspondence, or other relevant documents that can potentially influence the decision. 2. Prescription Medication Coverage Reconsideration Form: This type of Reconsideration form is utilized when a member disagrees with a coverage decision related to prescription medications. Members can outline why they believe the decision was incorrect and provide supporting documentation such as a doctor's prescription or medical necessity evidence. 3. Prior Authorization Reconsideration Form: This form is for members who have had their prior authorization request denied by Amerigroup. It enables them to present arguments, medical records, or any other information that can demonstrate the necessity or eligibility for the requested services or treatments. 4. Utilization Review Reconsideration Form: If Amerigroup has performed a utilization review and determined that certain services or treatments are not medically necessary or appropriate, members can use this form to contest that decision. They can provide evidence showing why they believe the services are indeed necessary for their health and well-being. 5. Appeals for Denial of Coverage Form: This type of Reconsideration form is used when a member's request for coverage is entirely denied. By submitting this form, members can express their disagreement and provide any supporting documentation or arguments to support their case for obtaining the desired coverage. Keywords: Amerigroup, Reconsideration forms, medical claim, denied claim, prescription medication coverage, prior authorization, utilization review, appeals, coverage denial.
Reconsideration Form For Amerigroup
Description
How to fill out Reconsideration Form For Amerigroup?
Working with legal paperwork and operations could be a time-consuming addition to your day. Reconsideration Form For Amerigroup and forms like it often require that you search for them and navigate the best way to complete them appropriately. As a result, regardless if you are taking care of economic, legal, or individual matters, using a extensive and convenient web catalogue of forms close at hand will help a lot.
US Legal Forms is the best web platform of legal templates, offering more than 85,000 state-specific forms and numerous tools to help you complete your paperwork easily. Discover the catalogue of appropriate documents available to you with just one click.
US Legal Forms offers you state- and county-specific forms available at any time for downloading. Safeguard your papers administration operations using a high quality support that lets you prepare any form within a few minutes without having extra or hidden cost. Just log in to your profile, locate Reconsideration Form For Amerigroup and acquire it straight away within the My Forms tab. You may also gain access to previously saved forms.
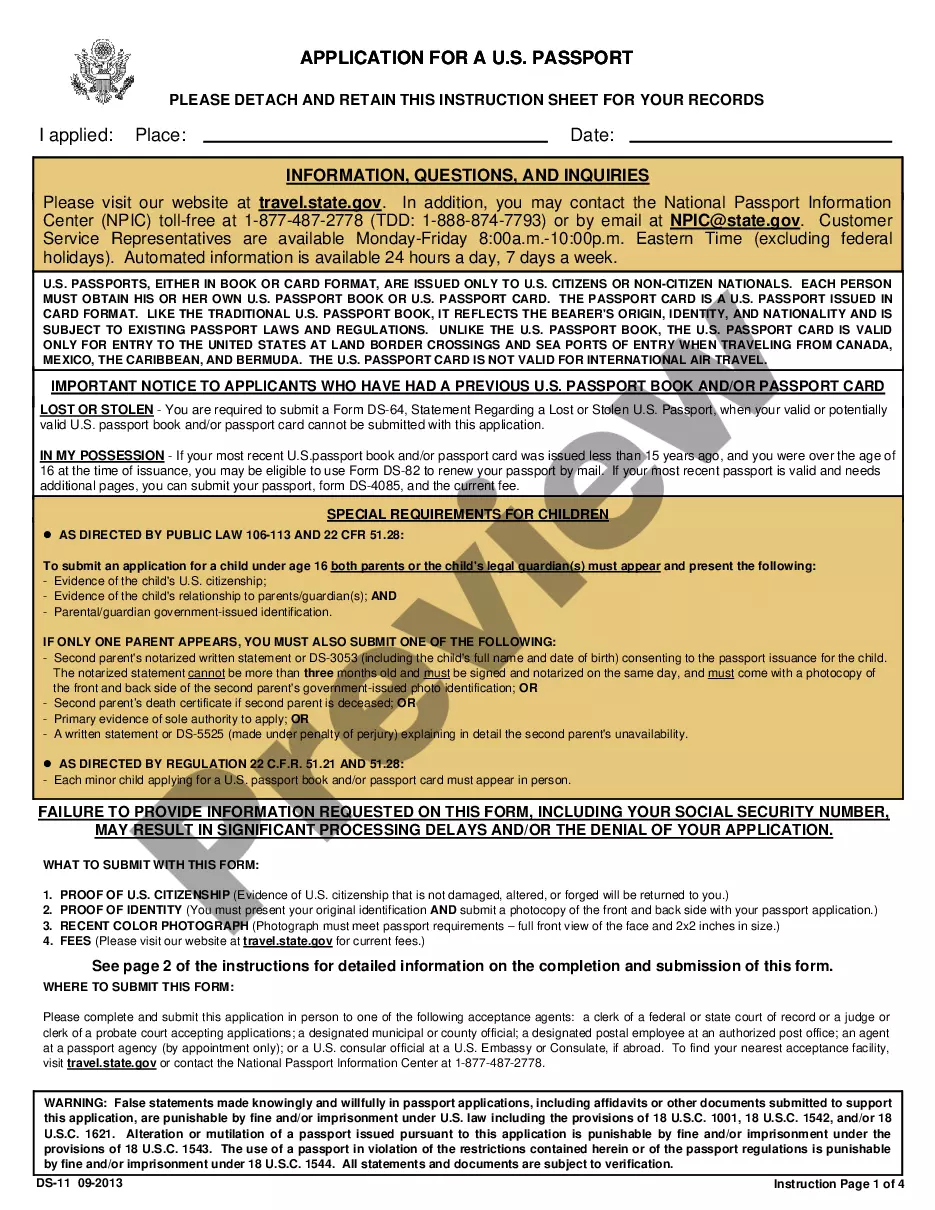
Is it the first time using US Legal Forms? Register and set up a free account in a few minutes and you’ll have access to the form catalogue and Reconsideration Form For Amerigroup. Then, adhere to the steps below to complete your form:
- Ensure you have the correct form using the Preview feature and reading the form information.
- Choose Buy Now when all set, and select the subscription plan that is right for you.
- Press Download then complete, sign, and print out the form.
US Legal Forms has twenty five years of expertise helping users deal with their legal paperwork. Find the form you require today and improve any operation without having to break a sweat.
Form popularity
FAQ
How do I file an appeal? If you have received a Notice of Agency Action, instructions for requesting an appeal are included on the notice. If you have not received a notice, contact 2-1-1 or visit your local office. An appeal may be requested in person, by phone, fax or mail.
How to request an appeal. You must submit your appeal within 60 days of the date on our first denial letter.
Amerigroup follows the timely filing standard of 365 days for participating and nonparticipating providers and facilities. Timely filing is determined by subtracting the date of service from the date Amerigroup receives the claim and comparing the number of days to the applicable federal or state mandate.
Written complaints can also be sent to the attention of the Provider Relations department of the local health plan or faxed to 1-844-664-7179. Complaints may also be sent by email to TXproviderrelations@amerigroup.com or via the provider website at .