Release Of Information Consent Form Psychology In Palm Beach
Description
Form popularity
FAQ
Basic Elements of Informed Consent Purpose of the Research. Description of the Research. Risks. Benefits. Alternatives to Participation.
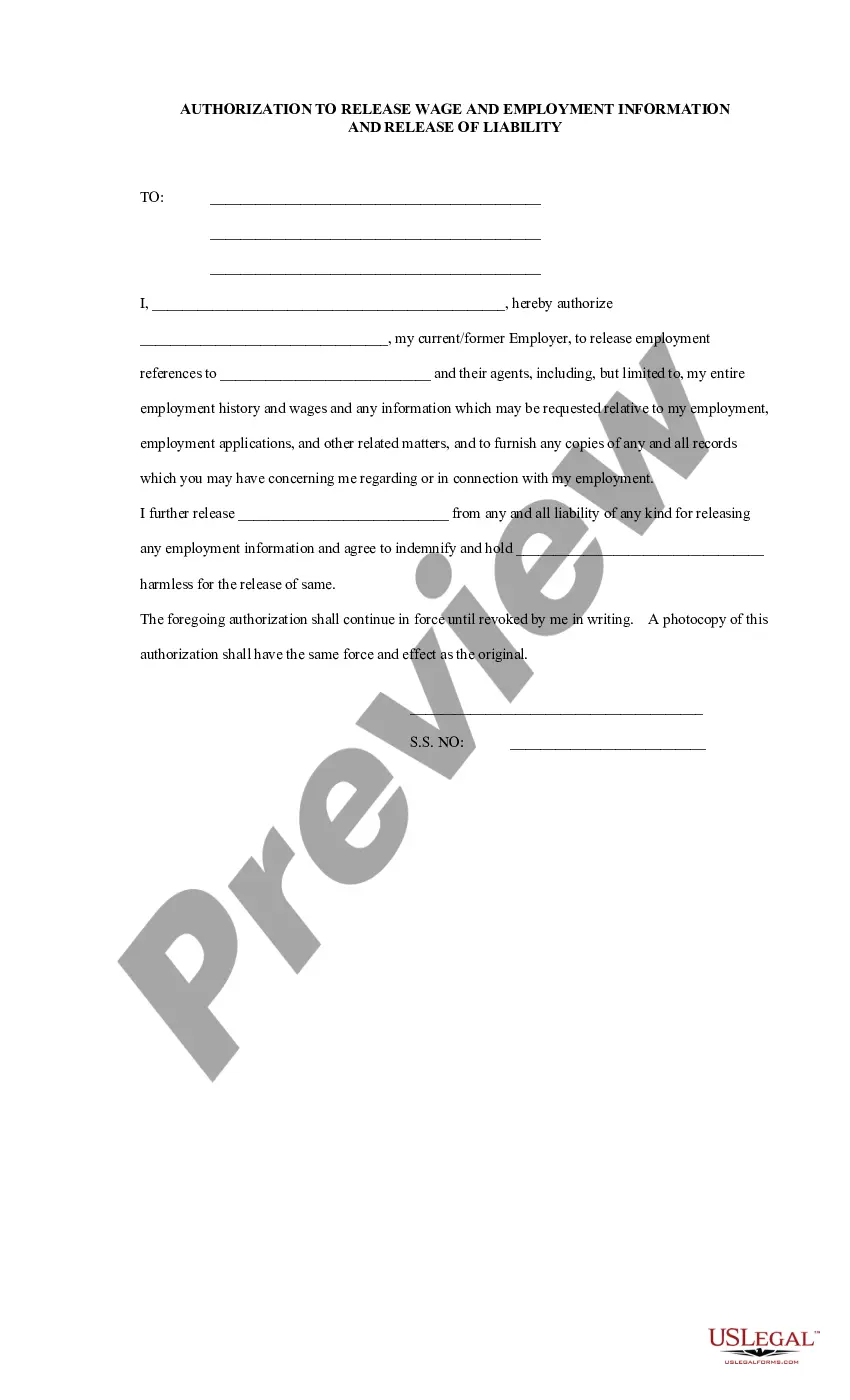
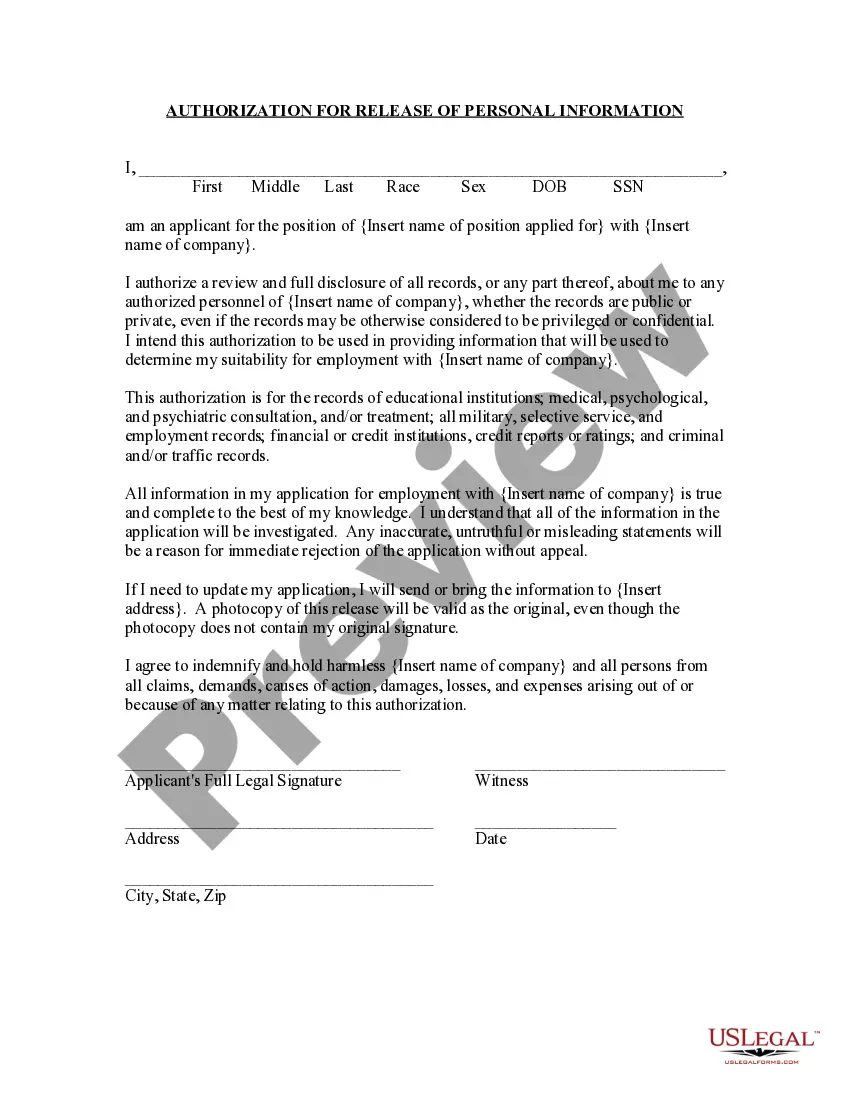
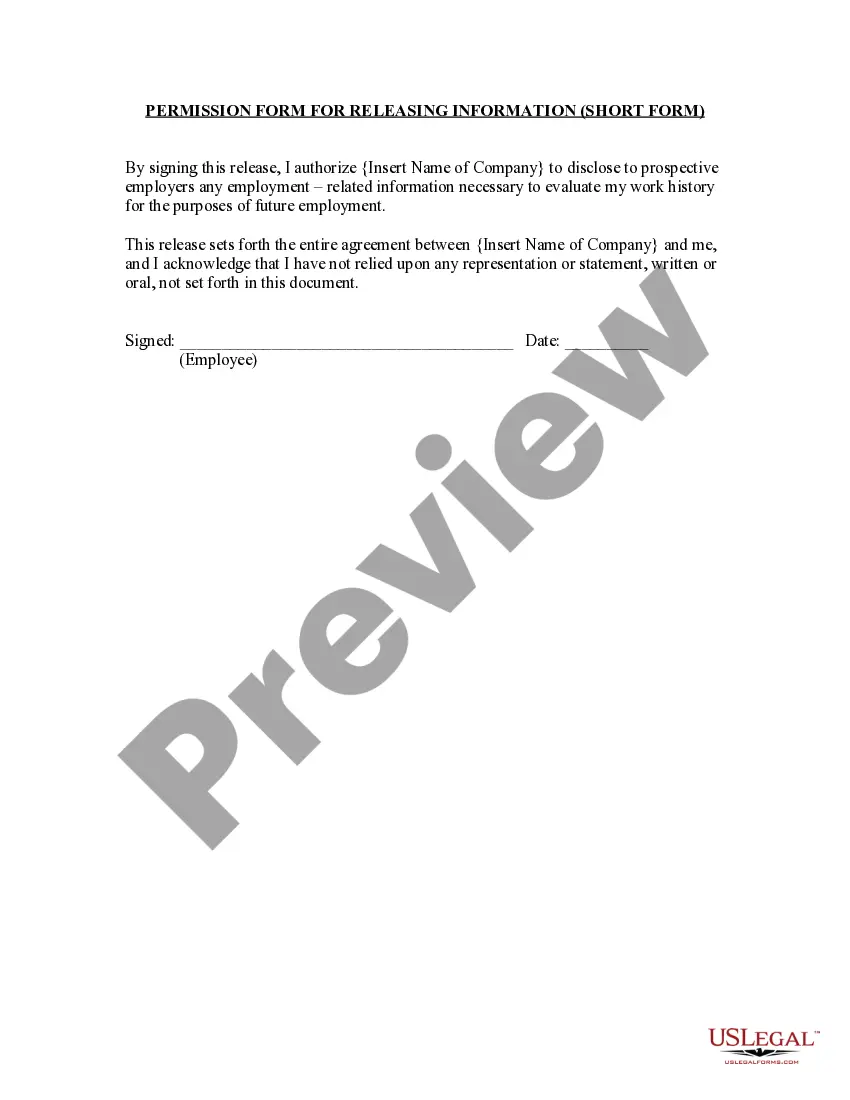
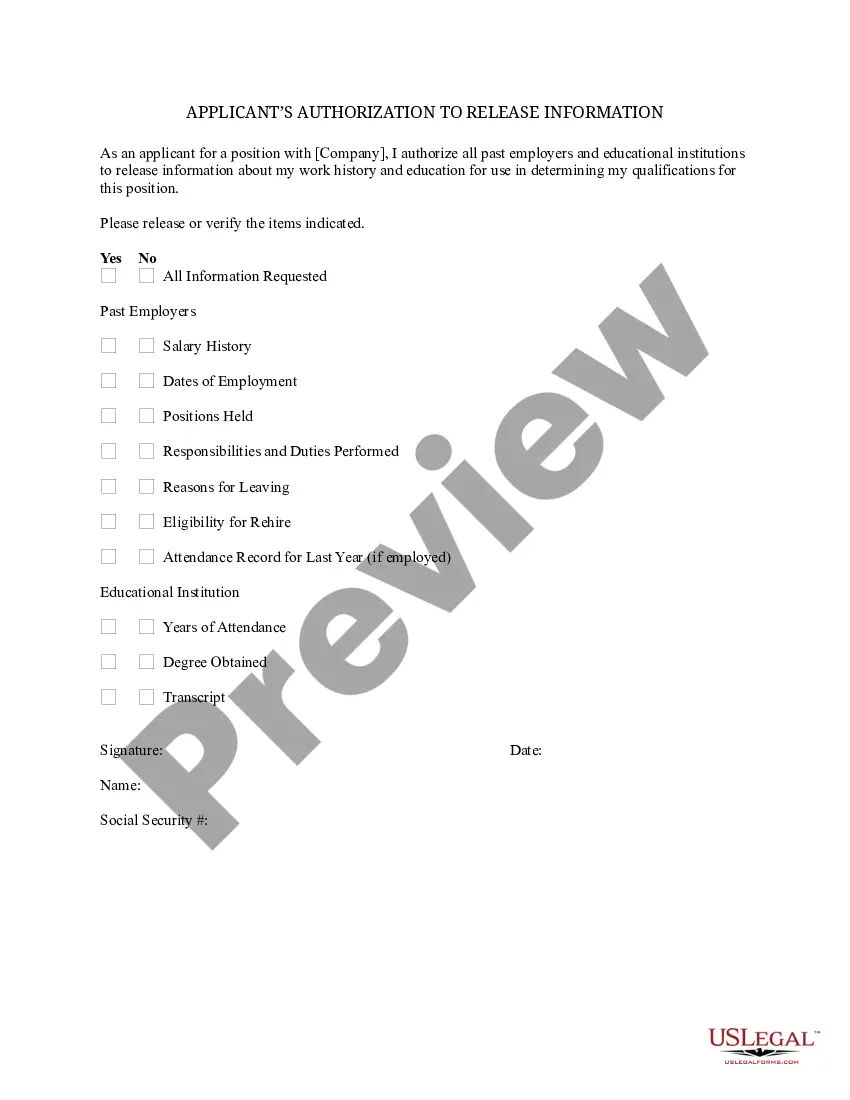
Contained in a consent form are the contact information for the creator of the form, details of the services to be provided (or a summary of the research), a voluntary participation statement, and a statement for privacy and liability. At the end should always include a place for the participant to sign.
Instructions for Developing an Informed Consent Document General Information. Describe the purpose(s) of this research study in lay terms. Purpose of the Study. Procedures. Risks. Benefits. Compensation, Costs and Reimbursement. Withdrawal or Termination from Study. Confidentiality.
Please indicate with your signature on the space below that you understand your rights and agree to participate in the experiment. Your participation is solicited, yet strictly voluntary. All information will be kept confidential and your name will not be associated with any research findings.
I have read and understand the information in this form. I have been encouraged to ask questions and all of my questions have been answered to my satisfaction. I have also been informed that I can withdraw from the study at any time. By signing this form, I voluntarily agree to participate in this study.
How to write a consent form: A step-by-step guide Step 1: Title and introduction. Step 2: Description of the activity. Step 3: Risks and benefits. Step 4: Confidentiality and data handling. Step 5: Voluntary participation and withdrawal. Step 6: Consent statement. Step 7: Signature and date. Step 8: Contact information.
At a minimum, a well-designed informed consent form will address the following information: Risks and benefits of treatment. Fees and payment policies. Confidentiality and its limits. Contact information and communication. Social media policy and general boundaries. Emergency procedures.
Consent refers to the patient's giving permission for electronic medical records to be released to third parties involved in treatment, utilization review, insurance payment, quality assurance, and continuity of care. Authorization is required for all other uses to which a patient's medical records may be put.
A Florida patient generally must given written consent to the release of medical records. Florida physicians, meanwhile, must report cases of tuberculosis and STDs to the state Department of Health.
Release of Information Authorization Under the HIPAA Privacy Rule, when a release of information is intended for purposes other than medical treatment, healthcare operations, or payment, you'll need to sign an authorization for ROI.