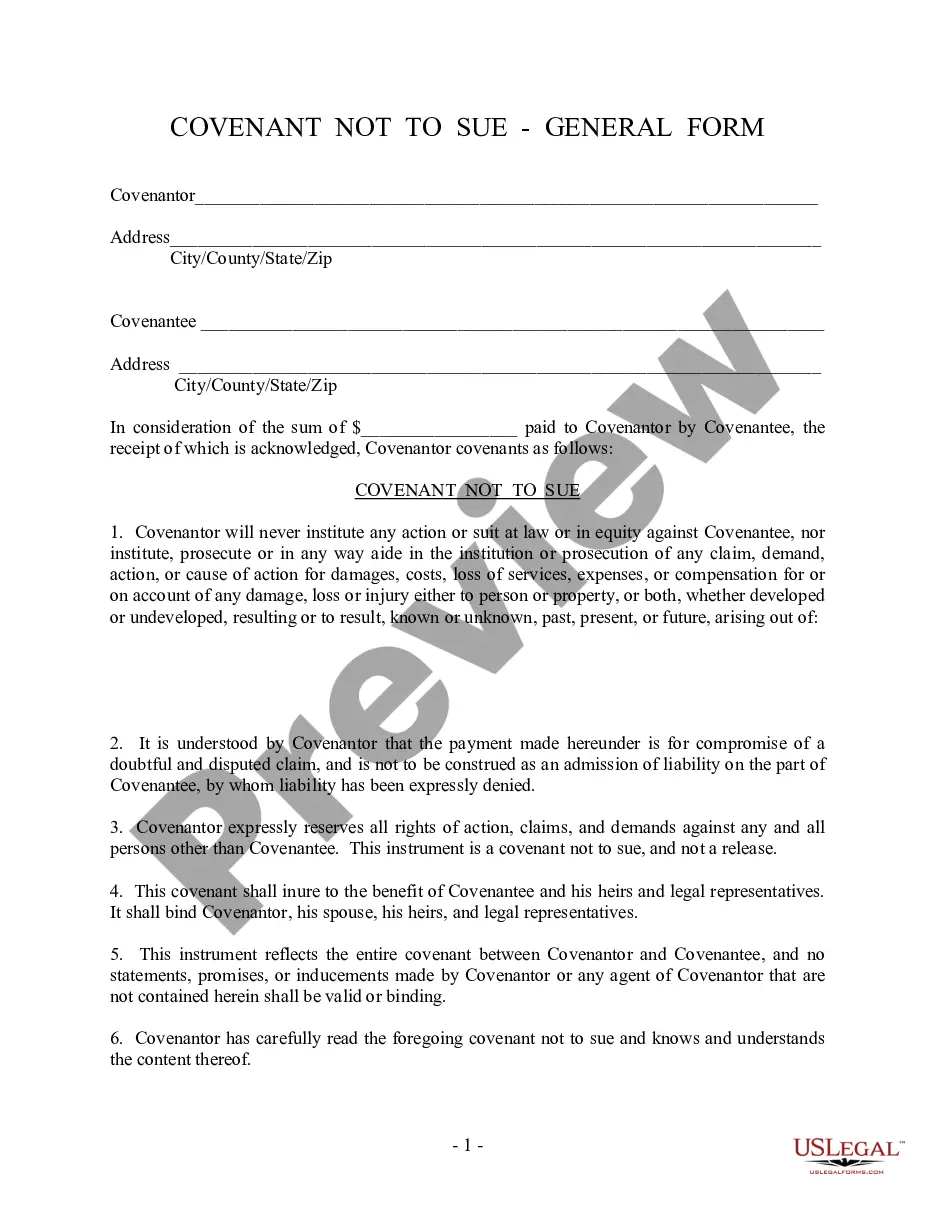
The parties may agree to a different performance. This is called an accord. When the accord is performed, this is called an accord and satisfaction. The original obligation is discharged. In order for there to be an accord and satisfaction, there must be a bona fide dispute; an agreement to settle the dispute; and the performance of the agreement. An example would be settlement of a lawsuit for breach of contract. The parties might settle for less than the amount called for under the contract.
Anthem Claim Dispute Form For Reimbursement In Texas
Description
Form popularity
FAQ
BCBSTX requires all health care providers to file electronic claims using National Standard Format (NSF), American National Standards Institute (ANSI 837) or UB-04 format or paper claims utilizing the CMS-1500 or UB-04 forms. ALL paper claims for health care services MUST be submitted on one of these forms/formats.
Important Note: You must submit your appeal within 180 days of the date on the Adverse Benefit Determination or denial letter.
You must request an appeal by 60 days from the date your notice for denial of services was mailed. We will give you a decision on your appeal within 30 days.
Anthem and Blue Cross Blue Shield are related, but they are not the same company. While they are both top health insurance providers in the USA, the big difference is that Blue Cross Blue Shield is the umbrella that is made up of several independent companies, and one of these smaller companies is Anthem.
An administrative appeal is a request for review of (not a hearing on) claims that are denied by TMHP or claims processing entity for technical and nonmedical reasons. There are two types of administrative appeals: Exception requests to the 95-day filing deadline or 120-day appeal deadline.
You must request an appeal by 60 days from the date your notice for denial of services was mailed.
Anthem is a separate company with which BCBSTX works to administer certain aspects of your health care plan with us when you receive health care services in one of the following states: California, Colorado, Connecticut, Georgia, Indiana, Kentucky, Maine, Missouri, Nevada, New Hampshire, New York, Ohio, Virginia, or ...
Find out more about filing complaints, appeals, emergency appeals, state fair hearings and external medical reviews by calling one of the following numbers: BCBSTX Customer Advocate Department: 1-888-657-6061 (TTY: 711). STAR Member Advocate: 1-877-375-9097 (TTY: 711)
About Premera Blue Cross Premera is headquartered in Washington State and provides health benefits to 2.8 million people nationwide. Our SEBB plans are designed with school employees in mind and are backed by best-in-class customer service and the Blue Cross Blue Shield Association.