Here Denied Claim For Primary Eob In Pima
Description
Form popularity
FAQ
The EOB is your insurance company's written explanation for that claim, showing the name of the provider that covered the service and date(s) of service. The insurer is also required to send you a clear explanation of how they computed your benefits.
Steps to Appeal a Health Insurance Claim Denial Step 1: Find Out Why Your Claim Was Denied. Step 2: Call Your Insurance Provider. Step 3: Call Your Doctor's Office. Step 4: Collect the Right Paperwork. Step 5: Submit an Internal Appeal. Step 6: Wait For An Answer. Step 7: Submit an External Review. Review Your Plan Coverage.
Business people commonly use COB and EOB interchangeably. EOB stands for “end of business,” a phrase that has the same meaning as “close of business.” In other words, the time when a company closes its doors at the end of the day.
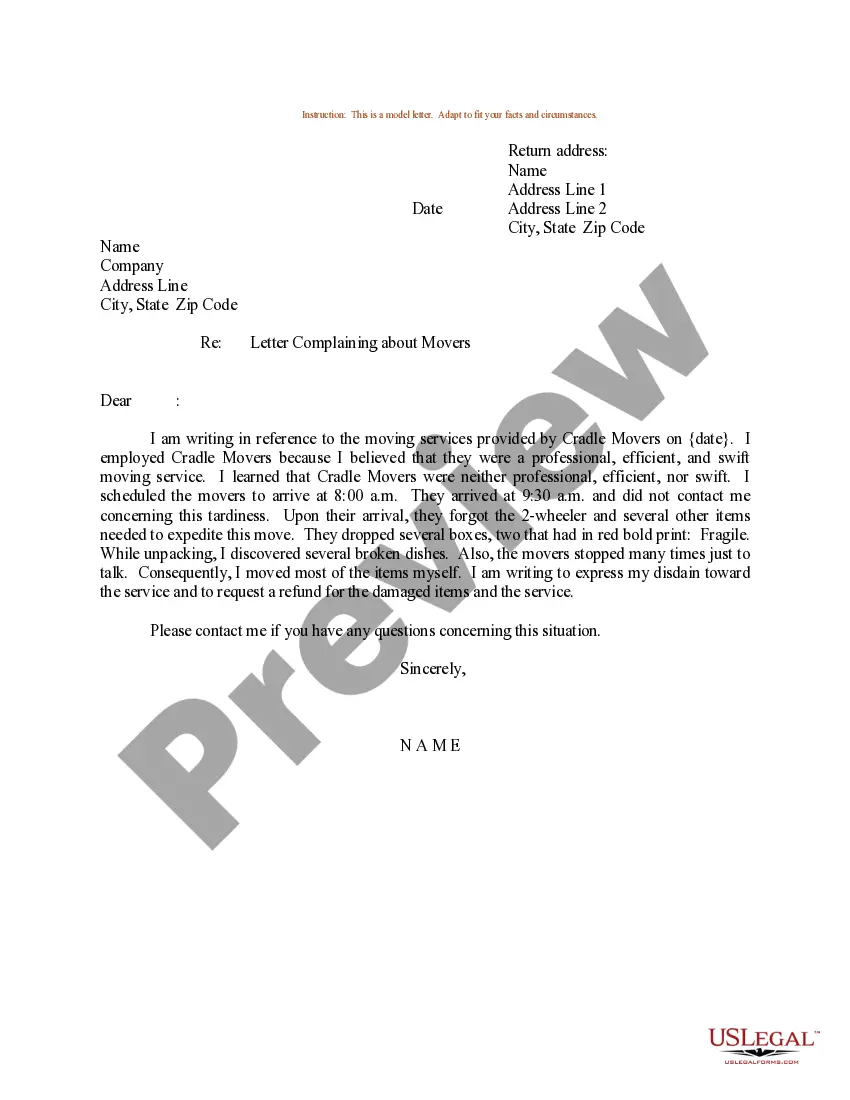
To Whom It May Concern: I am writing to request a review of your denial of the claim for treatment or services provided by name of provider on date provided. The reason for denial was listed as (reason listed for denial), but I have reviewed my policy and believe treatment or service should be covered.
Explanation of Benefits (EOB) Lookup.
Claim Denials are claims that have been received and processed by the insurance carrier and have been deemed unpayable for a variety of reasons. These claim denials typically contain an error that was flagged after processing.
Claim Denial: If a healthcare claim is denied because one code was unbundled, it indicates there was a breach of these coding guidelines. This means that the healthcare provider did not follow the standard procedure for billing, which necessitates adherence to ethical practices.
This denial code indicates that the necessary supporting documentation or information was not included with the claim, leading to its denial.
Some of the effective tips to improve denial management in healthcare are: Understand Why Claims were Denied. Streamline the Denial Management Process. Process Claims in a Week. Implement a Claims Denial Log. Identify Common Healthcare Claims Denial Trends. Outsource Your Medical Billing Denial Management Process.