Denied Claim Agreement For Authorization In Phoenix
Description
Form popularity
FAQ
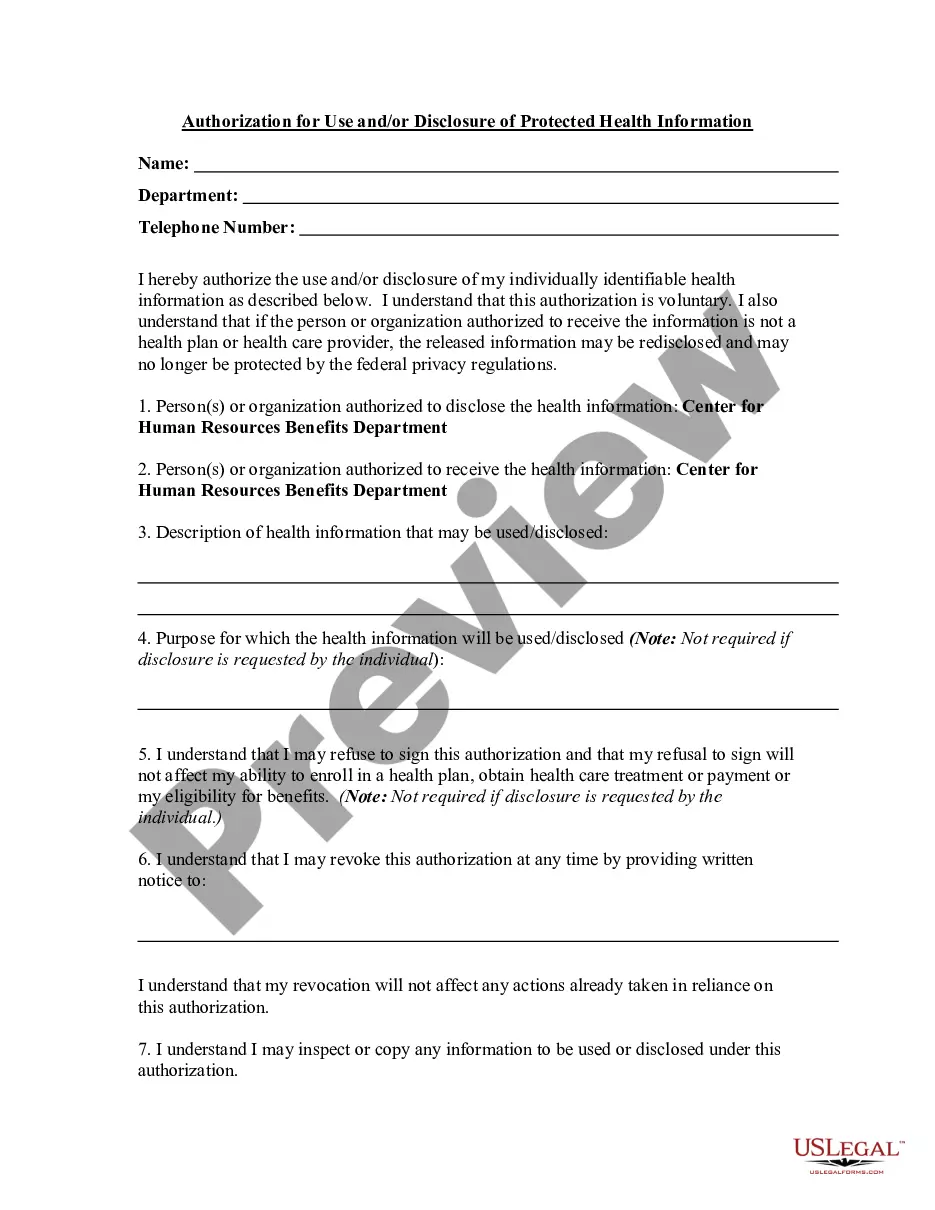
Arizona Complete Health-Complete Care Plan (Medicaid Only) Information on that process can be obtained by calling the AHCCCS Help Desk at (602) 417-4451. AHCCCS has developed a Web application that allows providers to verify eligibility and enrollment using the Internet.
Steps to Appeal a Health Insurance Claim Denial Step 1: Find Out Why Your Claim Was Denied. Step 2: Call Your Insurance Provider. Step 3: Call Your Doctor's Office. Step 4: Collect the Right Paperwork. Step 5: Submit an Internal Appeal. Step 6: Wait For An Answer. Step 7: Submit an External Review. Review Your Plan Coverage.
Appeals must be filed with the RBHA (or AHCCCS for the TRBHAs) and must be initiated no later than 60 days after the decision or action being appealed.
Denial code 197 means that the precertification, authorization, notification, or pre-treatment requirement was not fulfilled or was absent.
Filing an Appeal. Appeals can be filed orally or in writing within 60 days after the date of a Notice of Adverse Benefit Determination or Notice of Decision and Right to Appeal. The Notice explains to you how to file an appeal and what the deadline is for filing an appeal.
You have 60 calendar days from the date of BCBSAZ Health Choice's Notice of Adverse Benefit Determination or the date of any adverse action to file your Appeal. Health Choice will send you a letter stating we received your request. This will be sent to you within five working days.
If your request for prior authorization is denied, then you and your patient will be notified about the denial. The first step is to understand the reason behind the denial, so contact the health insurance company to find out the problem. For example, a PA request for a medication might be rejected due to many reasons.