Here Denied Claim For Authorization In Ohio
Description
Form popularity
FAQ
Steps to Appeal a Health Insurance Claim Denial Step 1: Find Out Why Your Claim Was Denied. Step 2: Call Your Insurance Provider. Step 3: Call Your Doctor's Office. Step 4: Collect the Right Paperwork. Step 5: Submit an Internal Appeal. Step 6: Wait For An Answer. Step 7: Submit an External Review. Review Your Plan Coverage.
Authorization Denial Rate is a key metric in healthcare revenue cycle management that measures the percentage of denied claims due to lack of proper authorization.
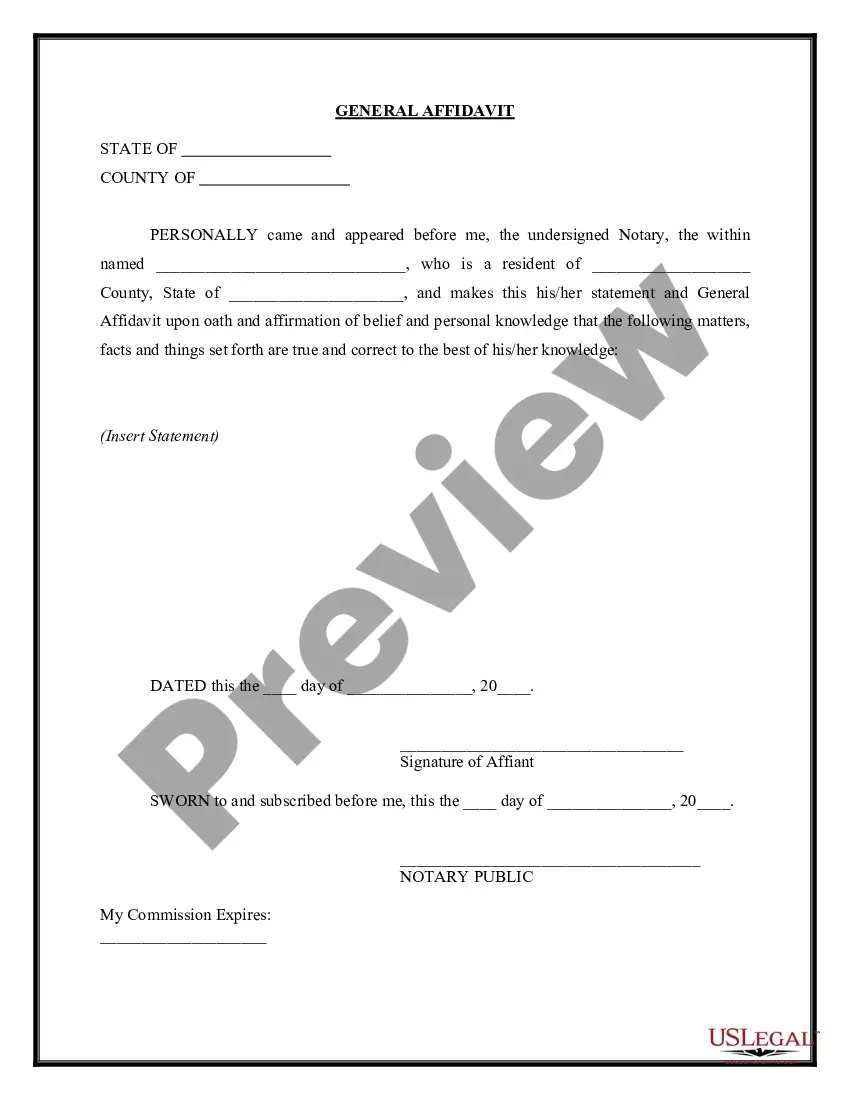
Expert-Verified Answer The proper response to a failure to obtain preauthorization denial is to request a retrospective review. This allows the insurance company to evaluate the claim post-service and potentially approve coverage based on provided documentation.
Thorough documentation based on a respected clinical source is the best way to obtain preauthorization or appeal a denial. In addition to government sources such as AHRQ, it may be worth asking your most frequent payers what guidelines they use. Clearly document any deviation from evidence-based guidelines.
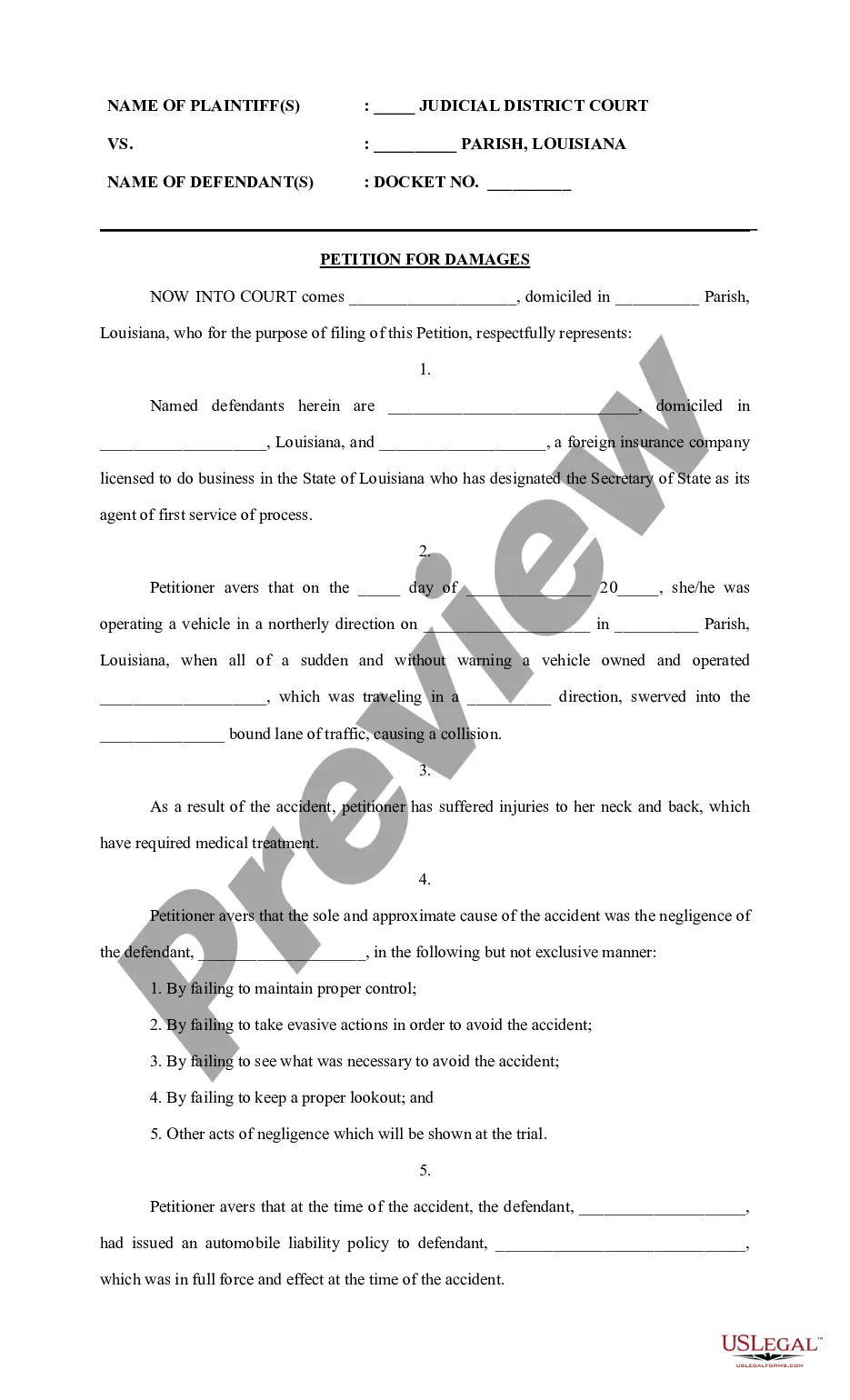
You may also file an appeal if your health plan denies pre-approval (called prior authorization) for a benefit or service. There are two types of appeals—an internal appeal and an external review. You file an internal appeal to ask your health plan to review its decision to deny a claim.
If your request for prior authorization is denied, then you and your patient will be notified about the denial. The first step is to understand the reason behind the denial, so contact the health insurance company to find out the problem. For example, a PA request for a medication might be rejected due to many reasons.
To ask for a hearing, call or write your local agency or write to the Ohio Department of Job and Family Services, Bureau of State Hearings, PO Box 182825, Columbus, Ohio 43218-2825. If you receive a notice denying, reducing or stopping your assistance or services, you will receive a state hearing request form.
(1) An insurer shall within twenty-one days of the receipt of properly executed proof(s) of loss decide whether to accept or deny such claim(s).
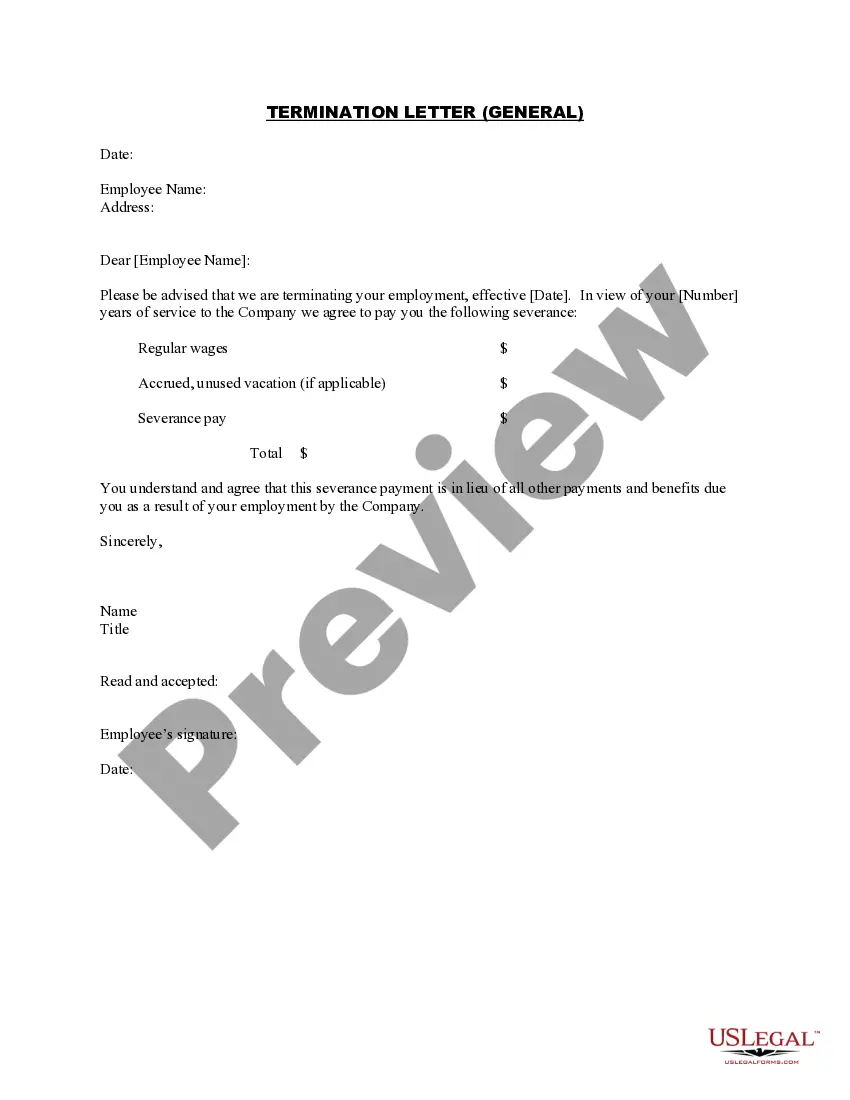
To Whom It May Concern: I am writing to request a review of your denial of the claim for treatment or services provided by name of provider on date provided. The reason for denial was listed as (reason listed for denial), but I have reviewed my policy and believe treatment or service should be covered.
Ans: You can file a complaint with the IRDAI's Grievance Cell of Consumer Affairs via phone or email to complaints@irdai.in if you do not agree with the rejection of your health insurance claim. You can also file a complaint on the Integrated Grievance Management System (IGMS) online on their website.