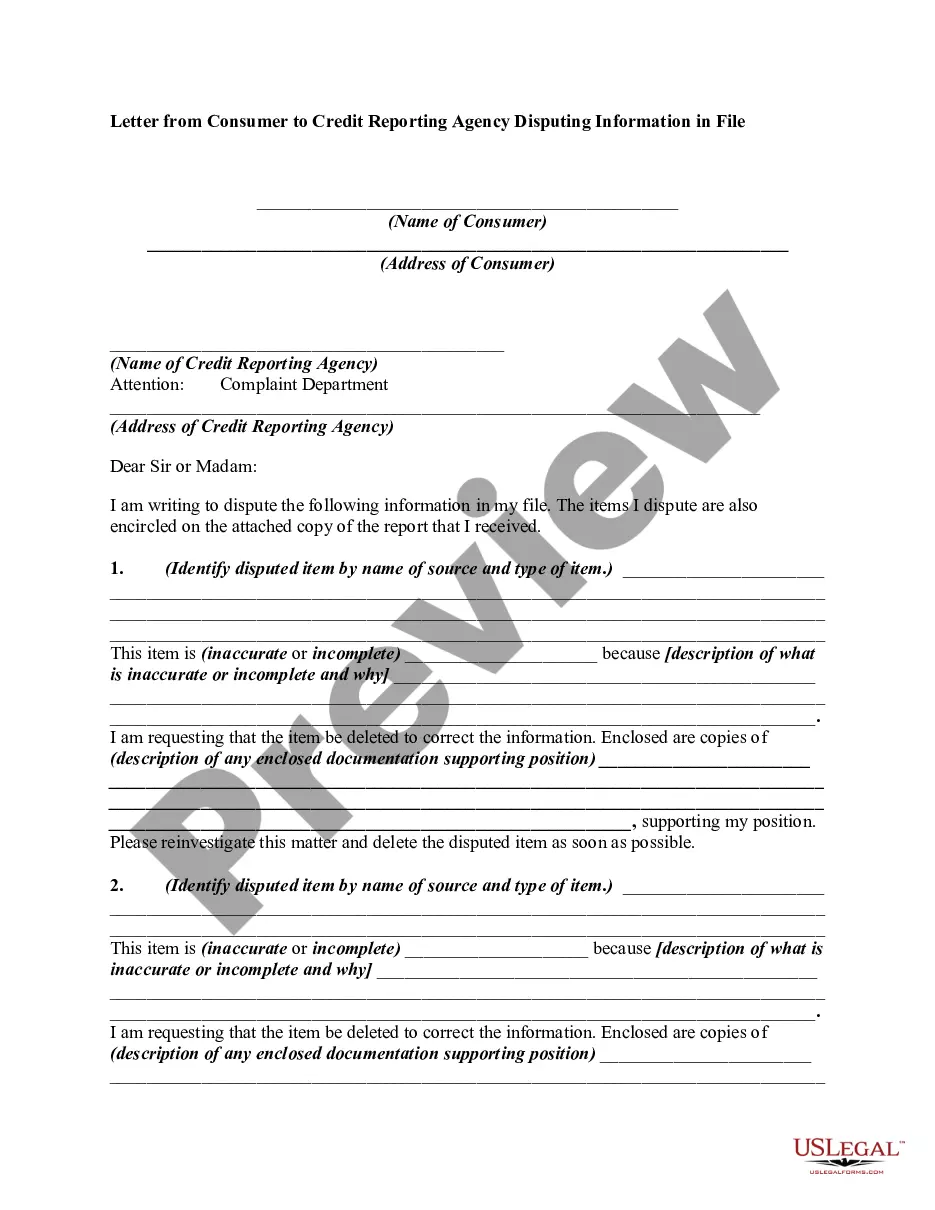
The parties may agree to a different performance. This is called an accord. When the accord is performed, this is called an accord and satisfaction. The original obligation is discharged. In order for there to be an accord and satisfaction, there must be a bona fide dispute; an agreement to settle the dispute; and the performance of the agreement. An example would be settlement of a lawsuit for breach of contract. The parties might settle for less than the amount called for under the contract.
Anthem Claim Dispute Form For Medication In Nevada
Description
Form popularity
FAQ
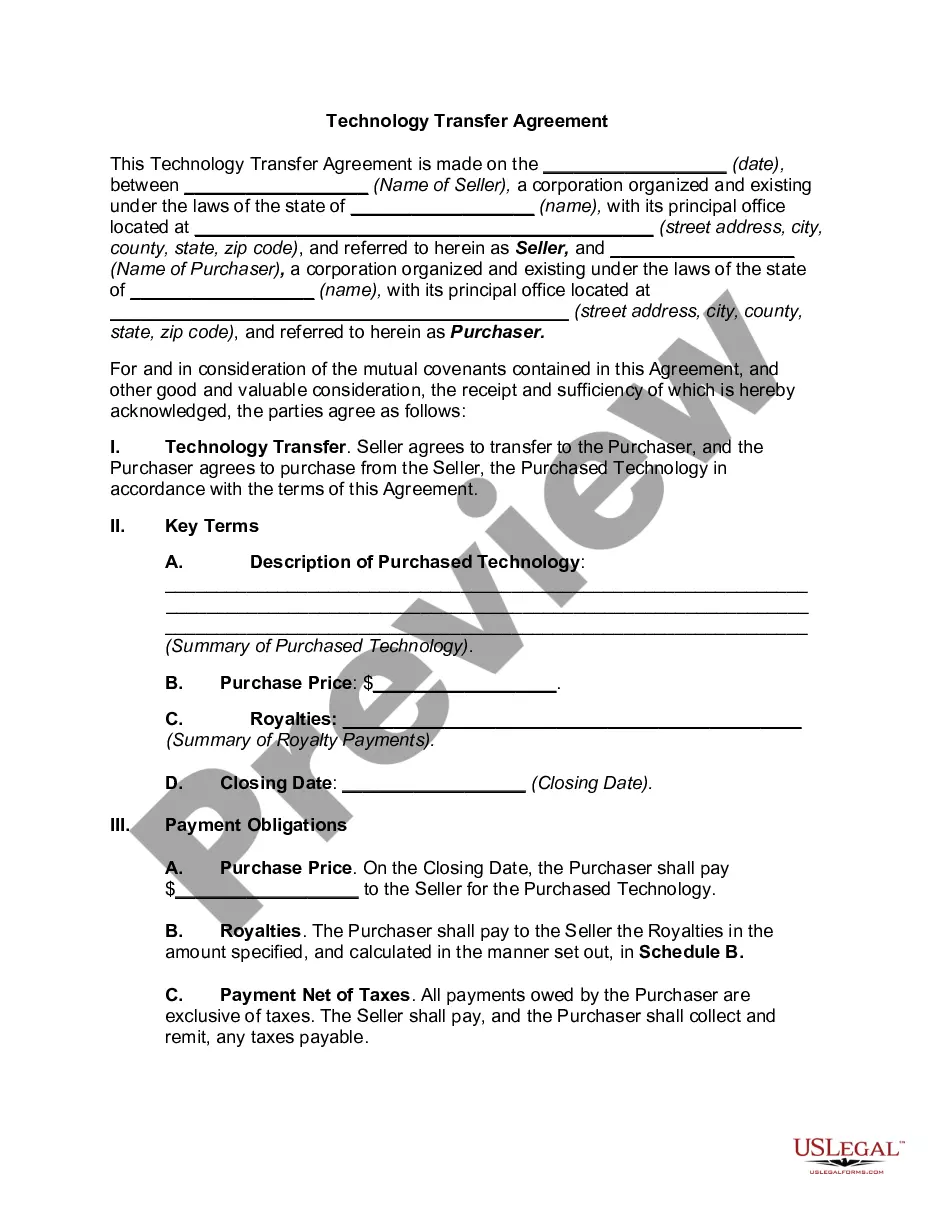
Our clearinghouse uses payer ID BS001 for Blue Shield, and BC001 for Anthem Blue Cross. In addition to reaching out to the payer directly to confirm where claims need to be submitted, you can also use this Claims routing tool.
Member Services: 1-844-396-2329 (TTY 711)
Your payer name is Anthem BCBS Nevada and the payer ID is 00265 (If you use a billing company or clearinghouse for your EDI transmissions, please work with them on which payer ID they want you to use.)
When submitting your 837 (I & P) files, please use our Payer ID: MLNNV.
Our individual & family health plans in Nevada are designed to be affordable for different needs and budgets. With a variety of coverage options, we make it easier for you and your family to live your healthiest lives. A ZIP code helps us find plans in your area.
Your payer name is Anthem BCBS Nevada and the payer ID is 00265 (If you use a billing company or clearinghouse for your EDI transmissions, please work with them on which payer ID they want you to use.)
Claims – Payor ID 76342 or 76343 Please contact us to discuss options for submitting attachments with your electronic claims.
-Timely filing is within 180 days of the date of service or per the terms of the provider agreement. Out-of-state and emergency transportation providers have 365 days from the last date of service.
Timely filing is when an insurance company put a time limit on claim submission. For example, if a insurance company has a 90-day timely filing limit that means you need to submit a claim within 90 days of the date of service.
The appeal must be received by Anthem Blue Cross (Anthem) within 365 days from the date on the notice of the letter advising of the action.